1. Background
Cancer refers to a group of diseases, in which abnormal cells divide and spread without control. Most of these abnormal cells may continue growing and form a mass called a tumor. In breast cancer, the tumor can be originated from different cells such as milk-producing ducts and glandular tissues. According to the World Health Organization (WHO), in terms of population, breast cancer has the second rank in the world among women, which leads to deaths (1-4). Breast cancer can be usually detectable by screening examinations (5). Early-stage breast cancer recognition is firmly related to breast self-examination (BSE), especially where the examination by physician or mammography is not conceivable. There are many reasons behind BSE recommendations by health professionals, such as being individual, free of charge, without any harm or pain, accessible and available. Additionally, BSE does not require any specific device (6, 7). Statistics showed that most of the women in developing countries do not perform BSE for a variety of reasons. The previous studies indicated that a person who does BSE also follows up other medical examinations regarding breast cancer (8). BSE is not a screening method suggested by WHO, but it is used as an intervention that raises awareness in endangered women (9). A study on a group of Iranian women noticed age and marital status as predictors of BSE (10). In addition to socio-demographic and cultural characteristics, health beliefs were also associated with breast cancer and subsequently motivated the women’s health behaviors (11). The Health Belief Model (HMB) is a theory developed by Hochbaum, Leventhal, Kegeles, and Rosenstock, which can assess the association between the fear of illness and potential benefits of performing health behaviors (12). Previous studies showed that HBM-based training could significantly improve women’s beliefs toward risk factors, preventive measures, and screening behaviors of breast cancer (13, 14). HBM for screening breast cancer in previous studies was mostly based on western models, and few studies investigated the breast cancer examination behavior of Iranian women.
2. Objectives
This study aimed at finding the frequency of BSE performance and identifying its possible predictors in Iranian women based on the HMB. Path analysis examined one way implicit and explicit effect of HBM parameters concerning BSE.
3. Methods
This research has been conducted as a cross-sectional study from May to June 2018 in a health care center in northwest Tehran, Iran. This health center provides many medical services such as controlling the family population, immunization improvement, and children regular assessment to supervise their health condition; 460 families were registered in this center based on the files of women who have referred to this health center for any reason in the past year. Although the potential telephone numbers of many of the women in this sample were obtained from health care records, the interviewers needed further investigation. This required the use of standard telephone directories and cross-references and contacting information operators and individuals with the same last name as the sample patients. After calling, 225 women over 18 years old were eligible and consented to participate in the study. Women who were pregnant or who were breastfeeding at the time of study and who were previously diagnosed with breast cancer were excluded from the study. Champion’s revised HMB scale, the sample size for this research was finalized (15). Before the study, all participants in this research signed the consent application form. Based on confidentiality, all participants' information in this study has been saved.
In this study, the data were collected, using a 20-minute, self-reporting questionnaire developed by researchers, who used previous scientific literature and scales. The questionnaire was comprised of 3 subjects that have been considered in this research:
- Demographic characteristics: Age, educational status, occupation, marital status, breastfeeding, history of breast cancer in the family, doing breast examination by a doctor, and kind of problem.
- For estimating participants' knowledge, breast cancer knowledge test (BCKT) has been applied for all participants in this research that was developed by McCance et al. (1990) (16). The BCKT is a test that consists of 19 items that measure each individual’s information of breast cancer recognition and screening exams. In this scoring system, 1 point is assigned to any correct answers and 0.3 is assigned to none answered or not correct answers.
- Participants’ perception of BC and BSE: 26 questions have been designed for this item assessment (17) and were measured, using the HBM. The HBM variables consist of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers. This scale is the result of the work of many researchers (18). Aside from that, modified HBM for BC tools includes 26 items in 4 constructs, including perceived sensitivity - "SUS" (3 items), perceived severity - "SER" (7 items), perceived benefits - "BEN" (5 items), and perceived barriers to "BAR" (11 cases). These phrases were ranked, using a 5-point Likert scale (strongly agree, agree, undecided, disagree, and strongly disagree), and each phrase received a score of 1 to 5, with 5 indicating a strong or high understanding and 1 indicating a weak or low understanding. Reliability and internal consistency were measured for the present study. The result was 0.7 for the overall scale. The questionnaire transmits to a panel of 6 specialists, 2 of whom worked in the nursing department, 2 were oncologists in the cancer ward of King Saud Medical Complex, 1 was a doctor in the maternity hospital, and the last one was a family health member section to establish content validity and was reviewed for content validation. Minor changes were recommended (17).
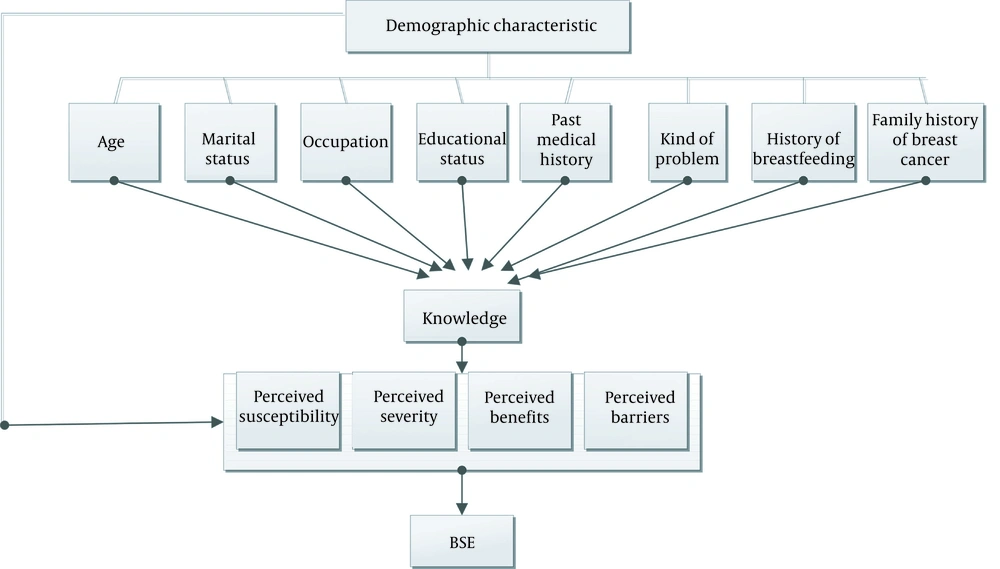
In this study, the conceptual framework of path analysis (Figure 1) about the relationship between demographic characteristics, knowledge, the concept of HBM and BSE among the study population was examined. However, there is a limitation of explanatory power since the mean explanatory power (R2) of each variable is only approximately 20%, HBM measurements, and models, are not sufficient to predict behavior (19). The relationship between specific HBM variables and BSE was also reviewed. Health knowledge added those variables to extensively examine the factors affecting general health examination behaviors. There is a positive relationship between health knowledge and health-promoting behaviors. Accordingly, health knowledge was considered in this work to examine its efficacy on behavioral purposes. A rational and communicative explanation of the perceived relationships and correlations can be inferred based on the results.
To analyze data with the application of path analysis, SPSS software version 22 and Liserel version 8.8 were used. The ANOVA and t test were used to examine the relationship between demographic variables and BSE. Pearson’s Correlation test was used to test the correlation between demographic factors, perceived severity, perceived susceptibility, perceived barriers, perceived benefits, knowledge, and BSE. However, variables remained as predictor factors of how to perform BSE after controlling the confounding factors.
4. Results
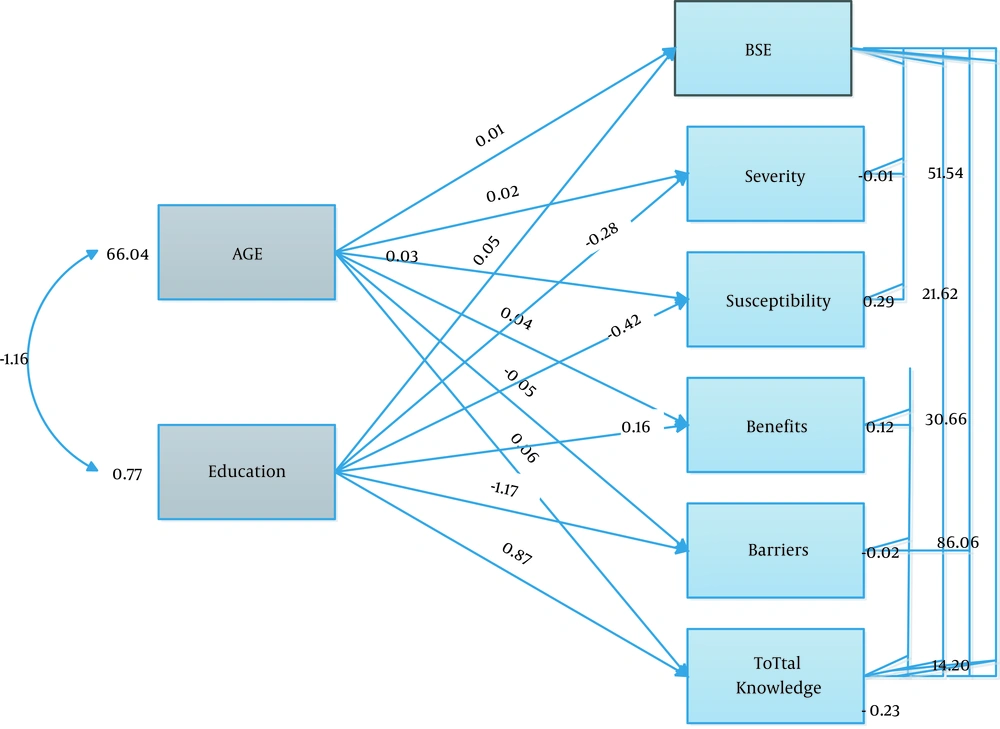
In this study, 225 women with a mean age of 30.16 ± 12.88 years were included. The mean of the BSE (the number of breast self-exam in the year) performance was 0.53 ± 0.52. According to Table 1, there were significant relationships between demographic variables and BSE (P ≤ 0.00). The mean number of times the BSE was higher in self-employed participants, higher education, family history of breast cancer, divorce, and breastfeeding. The mean scores of perceived severity, perceived susceptibility, perceived benefits, and perceived barriers were 24.45 ± 7.28, 9.98 ± 4.70, 19.86 ± 5.58, and 26.56 ± 9.40 respectively. The score of BCKT had a significant difference between women who performed and those who did not perform BSE (P = 0.001). For a path analysis, regression analysis was determined to check which available variables have a significant relationship with the dependent variable in the theoretical framework. Demographic variables (age educational status), knowledge, and HBM concepts were assessed to enter as independent variables. Age, perceived barriers, perceived severity, perceived susceptibility, and perceived benefits had a significant relationship with the dependent variable (BSE); so, they were considered in the final regression model. Bivariate analysis showed that BSE was positively and significantly correlated with educational level and knowledge, perceived benefits, and perceived susceptibility but negatively correlated with perceived barriers. Educational status and perceived severity are directly and significantly correlated with knowledge and perceived benefits (Table 2). The results of a preliminary model showed a good fit, accounting for 18% of the variance found. The logical correlation of the variables following a conceptual model showed a high degree of fitness and acceptance of the proposed model. So, both the proposed and the conceptual model manifested the same result (P = 0. 0.31) (Table 3). Figure 2 indicated empirical path models for effects of educational status, age, knowledge, and HBM concept on BSE. In the direct paths, perceived susceptibility with β = -0.29 and in indirect paths, knowledge with β = 0.77 had the most effects on BSE. Perceived susceptibility, perceived severity, perceived benefits, and perceived barriers affected BSE only through the direct path. Knowledge has a positive effect on BSE both directly and indirectly by affecting perceived susceptibility, perceived severity, perceived benefits, and perceived barriers with overall effect (β = 0.54). As a result, women with high knowledge and information about breast cancer will take BSE. Educational status, directly and indirectly, has a positive effect on BSE by affecting knowledge and perceived susceptibility, perceived severity, perceived benefits, and perceived barriers with overall effect (β = 0.064). Thus, women with high educational status will do BSE. Perceived barriers (β = -0.02), perceived susceptibility (β = 0.29), perceived severity (β = -0.01), and perceived benefits (β = 0.12) affect BSE only directly and have a negative effect on it. Women with more perceived barriers will not take BSE (Table 4).
| Characteristics | N | Means ± SD | Sig |
|---|---|---|---|
| Education | 0.020 | ||
| Under diploma | 8 (3.6) | 0.500 ± 0.53 | |
| Diploma | 67 (29.8) | 0.37 ± 0.48 | |
| Bachelor | 77 (34.2) | 0.61 ± 0.54 | |
| Master | 73 (32.4) | 0.61 ± 0.54 | |
| Occupation | < 0.001 | ||
| Employee | 72 (32) | 0.55 ± 0.50 | |
| Self-employed | 18 (8) | 0.61 ± 0.50 | |
| Housewife | 61 (27.1) | 0.55 ± 0.50 | |
| Unemployed | 64 (28.4) | 0.37 ± 0.48 | |
| Retired | 10 (4.5) | 1.28 ± 0.75 | |
| Marital status | < 0.001 | ||
| Single | 98 (43.6) | 0.32 ± 0.47 | |
| Married | 118 (52.4) | 0.69 ± 0.51 | |
| Divorced | 7 (3.1) | 0.85 ± 0.37 | |
| Widow | 2 (0.9) | 0.50 ± 0.70 | |
| Breastfeeding | < 0.001 | ||
| No | 130 (57.77) | 0.38 ± 0.50 | |
| Yes | 95 (42.2) | 0.74 ± 0.48 | |
| History of breast cancer in your family | 0.016 | ||
| I don’t know and No | 154 (64.4) | 0.48 ± 0.53 | |
| Yes | 71 (31.6) | 0.66 ± 0.47 | |
| Breast examination by a doctor | < 0.001 | ||
| No | 168 (74.7) | 0.44 ± 0.49 | |
| Yes | 57 (25.3) | 0.80 ± 0.51 | |
| Kind of problem | 0.001 | ||
| No problem | 168 (74.7) | 0.44 ± 0.49 | |
| Pain | 16 (7.1) | 0.81 ± 0.54 | |
| Benign | 8 (3.6) | 0.75 ± 0.46 | |
| Cyst | 25 (11.1) | 0.76 ± 0.52 | |
| Fibroma | 2 (0.9) | 1.00 ± 0.0 | |
| Discharge | 1 (0.4) | 1.00 ± 0.0 | |
| Others | 5 (2.2) | 1.00 ± 0.70 | |
| Age | 30.16 ± 12.88 | 0.296 | < 0.001 |
Distribution of the Participants' Characteristics (n = 225)
| Variables | BSE | Educational Status | Perceived Barriers | Perceived Severity | Perceived Susceptibility | Perceived Benefits | Knowledge |
|---|---|---|---|---|---|---|---|
| BSE | 1 | 0.175a | -0.257a | 0.245 | 156a | 0.147a | 0.183a |
| Educational Status | 1 | -0.116 | 0.173 | -0.069 | 0.033a | 0.173a | |
| Perceived Barriers | 1 | -0.111 | -0.151a | -0.352a | -0.114 | ||
| Perceived severity | 1 | 0.086 | 0.137a | 0.158a | |||
| Perceived susceptibility | 1 | 0.104 | 0.097 | ||||
| Perceived benefits | 1 | 0.102 | |||||
| Knowledge | 1 |
Correlations Among Age, Educational Status, HBM Variables, Knowledge, and BSE
| Model Index | ||||||
|---|---|---|---|---|---|---|
| χ2 | df | P | GFI | CFI | RMSEA | |
| Values | 126.05 | 6 | 0.31 | 0.96 | 0.68 | 0.16 |
The Goodness of Fit Indicators for the Model, N = 225
| Predictor Variables | Effects | Model Coefficients | t-Value | R2 | Errorvar | ||
|---|---|---|---|---|---|---|---|
| Direct | Indirect | Total | |||||
| Educational status a | 0.05 | -0.49 | -0.44 | 0.036 | 1.05 | 0.18 | 0.23 |
| Age | 0.01 | 0.55 | 0.56 | ||||
| Perceived barriers | -0.02 | - | -0.02 | -0.028 | 10.54 | ||
| Perceived susceptibility a | 0.29 | - | 0.29 | ||||
| Perceived severity a | -0.01 | - | -0.01 | ||||
| Perceived benefits a | 0.12 | - | 0.12 | ||||
| Knowledge | -0.23 | 0.77 | 0.54 | 0.023 | 2.18 | ||
Path Coefficients of Age, Educational Status, HBM Variables, Knowledge, and BSE
5. Discussion
In the present study, the mean of BSE performance in every month was 0.53 ± 0.52. Agbonifoh stated that female students were well-trained for BSE performance at a tertiary institution in Edo state (3). The study aimed at investigating a remarkable relationship between hypothesis and practical results through path analysis. Studies tried to increase the explanatory power of the model by developing the variables in the HBM, but most of those variables were only applicable to particular research topics (20). As the variables of the study were notably harmonized with the impacts with no limitation, the proposed model was successfully applied to different health examination components. HBM framework is a proper indicator to identify important factors having an impact on Iranian women's BSE utilization (21). According to the results of our study, only perceived barriers had a negative direct effect on BSE. Perceived barriers include not caring about BSE, not knowing the right way to perform BSE, and subsequently fear of being diagnosed with cancer. The most common BSE barrier in African American women was that they felt laughed at the BSE and BSE led to worry about breast cancer (22). In our study, the educational level had both direct and indirect effects on BSE. Relying on education alone is not enough for the promotion of healthy behaviors and paying attention to barriers also has an essential role. Our results indicated that BSE was positively performed in those with higher knowledge about breast cancer and lower perception about barriers. Based on Huang et al., participants in actual health examinations had the opportunity to utilize preventive health examinations; consequently, they received more social support and gained more medical knowledge (19). Studies conducted by Elsie et al. in Uganda (23) and Okolie in Nigeria (24) also showed that participants’ knowledge regarding breast cancer was significantly associated with the rates of BSE performance. Alam stated that the basis of primary prevention of breast cancer was associated with obtaining adequate knowledge of breast cancer’s risk factors (25). In this study, the BSE performance was 5.51 times higher in women with a high level of knowledge. This confirmed the essential role of knowledge for adopting and conducting health-promoting behaviors (19). Sama et al. expressed, however, there is match information regarding breast cancer, and the lack of specific available resources about the reasons and results of this issue is still problematic (1). Bourdeanu et al. found that knowledge of mammography screening was the strongest predictor of performing this screening method in Lebanese-American women and health care providers were the first source of information (26). Our research indicated that performing BSE and having breast cancer experience in first relatives are not related. These results were consistent with the findings of Secginli and Nahcivan (27), Omotara et al. (28), Okobia et al. (29). On the contrary, according to Rosvold et al. BSE had a higher rate of performance in women with a family history of breast cancer (30). General reasons for breast cancer can be considered genetic, family history, quality of life, and reproductive status (31).
5.1. Conclusions
According to the results of this study, self-care behaviors could be increased by eliminating perceived barriers and increasing the level of education and as a result of women's knowledge. Improvement in health education on the importance of health examination by health authorities and medical institutions to increase public health knowledge and decrease perceived barriers have been recommended. Various approaches can be applied to train communities for medical assessment and understanding the prominence of health issues prevention.