1. Background
Millions of people develop cancer worldwide each year, whose disease can be treated, controlled, and recovered easier when detecting timely and in early stages (1, 2). Based on the 2020 GLOBOCAN statistics, colorectal cancer (CRC) is considered the third most common new cancer case in Iran (3). CRC ranks as the 4th prevalent cancer among Iranian men after gastric, prostate, and lung ones, while it is the second new cancer case among Iranian women after breast cancer (3). In Iran, CRC incidence is more than 14 per 100000 individuals (4). In addition, the proportion of those diagnosed under 50 years old is higher due to the youngness of the population in Iran compared to the developed countries (2, 5, 6).
Changing lifestyle, as well as recognizing and controlling risk factors, can decrease the likelihood of cancer since CRC is among the most preventable cancers. Further, the disease can be prevented from progression and treated in the primary stages by performing screening and early detection measures (7, 8). In recent years, the early diagnosis and screening program for CRC has been integrated with the primary health care provider system of Iran, which was implemented at the national level since 2016. The program aims at identifying patients with CRC and suspected ones, as well as organizing and recording the data related to the patient care and treatment in the Sib system (integrated health system). In the program, health workers or health care providers register the data related to all of the individuals aged 50 to 70 years old recalled for CRC evaluation, as well as reviewing risk factors and symptoms based on the form in the system through patient self-reporting. Furthermore, a fecal immunochemical test (FIT) is requested when there are suspicious symptoms. Based on the risk assessment chart, the cases requiring more evaluations are referred for examining by a physician, among whom the approved ones are directed to the second level for specialized examinations and colonoscopy (9).
It is worth noting that distributing CRC and its risk factors is different in the various areas of Iran (1), which is affected by diverse factors (7, 10-13).
2. Objectives
Based on the cases recorded in the Sib system, the present study evaluated the CRC risk factors, symptoms, and participation rate of individuals aged 50 to 70 years old in the screening program covered by health centers in Arak, along with assessing CRC Crude incidence rate from 2016 to 2019.
3. Methods
The present cross-sectional study was conducted among all of the individuals aged 50 to 70 years old referred to the rural, urban, and suburban health centers in Arak for screening CRC since the beginning of implementing the CRC screening program from September 2016 to 2019, and their data were registered in the Sib system. The population was selected since the individuals aged 50 to 70 years old are supposed as the target population in screening CRC by considering the national CRC screening guideline. The data were recorded in the system based on the interviews done with the subjects by the health workers or health care providers, as well as patient self-reporting. Considering the symptoms (lower gastrointestinal bleeding, constipation with or without diarrhea, and weight loss) and risk factors (family and individual history of CRC, colorectal adenoma, and inflammatory bowel disease) and based on the executive guideline for CRC prevention and early diagnosis program, the cases needing more assessments were directed to the center physician and, then, the second level for performing colonoscopy and other specialized examinations and tests, if required. In addition, the CRC incidence in the age range was calculated based on the definitive CRC cases extracted from pathology/hospital reports. Further, the quantitative and qualitative data were expressed as mean (SD) and number (percentage), respectively. Furthermore, the relationship between underlying variables such as age, gender, and residence with the risk factors and symptoms of the disease was evaluated through the chi-squared test. The population of previous years was estimated with a 1% growth rate and applied to determine incidence trend from 2016 to 2019 due to the availability of the data related to the individuals aged 50 to 70 years old referred to health care centers in Arak during 2019 (M = 41,838).
The crude incidence rate among the population aged 50 to 70 years old is calculated by dividing the new cases by the populations at risk of CRC in a specific year.
In addition, the 95% confidence interval (CI) is calculated as follows (14):
The data were analyzed by using SPSS 23 with a significance level of 0.05.
4. Results
A total of 41,838 individuals were referred to the urban, rural, and suburban health care centers in Arak for screening CRC since the beginning of implementing the program among the intended populations from September 2016 to 2019. The individuals’ participation rate in the CRC screening program is 44.2%, which is greater among women and villagers (Table 1).
| Variables | Total Population | Participate in the Screening Program, No. (%) | Participation Rate |
|---|---|---|---|
| Sex | |||
| Female | 47,680 | 26,447 (63.2) | 55.5 |
| Male | 46,947 | 15,391 (36.8) | 32.8 |
| Age (y) | |||
| < 60 | 25,622 (61.2) | ||
| ≥ 60 | 16,216 (38.8) | ||
| Residence | |||
| Urban | 54,131 | 20,465 (48.9) | 37.8 |
| Suburban | 29,337 | 11,045 (26.4) | 37.6 |
| Rural | 11,018 | 10,328 (24.7) | 93.7 |
Table 2 indicates the distribution of CRC risk factors and symptoms among the subjects by gender, residence, and age range. Based on the results, constipation in the last month, as the most common symptom (1.97%), was significantly higher among women compared to men (P ≤ 0.001). In addition, the CRC family history in the first-degree relatives, as the second conventional risk factor, was more prevalent among women, which was significantly different from that of men (P ≤ 0.003). The number of women with CRC family history in the second-degree relatives such as uncles, aunts, grandfathers, and grandmothers under 50 years old was greater than men with significant difference (P ≤ 0.001).
| Symptoms | Total | Sex | Age | Residence | ||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | < 60 | ≥ 60 | Urban | Suburban | Rural | ||
| Lower gastrointestinal bleeding in the last month b | 158 (0.38) | 104 (0.39) | 54 (0.35) | 97 (0.38) | 61 (0.38) | 91 (0.44) | 52 (0.47) | 15 (0.14) |
| Constipation (with or without diarrhea, abdominal pain) in the last month b, c | 825 (1.97) | 611 (2.31) | 214 (1.39) | 493 (1.92) | 332 (2.05) | 424 (2.07) | 243 (2.20) | 87 (0.84) |
| Weight loss ≥ 10% in the last 6 months | 56 (0.13) | 31 (0.12) | 25 (0.16) | 36 (0.14) | 20 (0.12) | 31 (0.15) | 15 (0.14) | 10 (0.10) |
| Family history of colorectal cancer in first-degree family members b, c | 648 (1.55) | 446 (1.69) | 202 (1.31) | 414 (1.62) | 234 (1.44) | 419 (2.05) | 167 (1.51) | 62 (0.60) |
| Family history of colorectal cancer in second-degree family members under 50 years of age b, c, d | 205 (0.49) | 152 (0.57) | 53 (0.34) | 143 (0.56) | 62 (0.38) | 119 (0.58) | 66 (0.60) | 20 (0.19) |
| Individual history of colorectal cancer | 78 (0.19) | 53 (0.20) | 25 (0.16) | 50 (0.19) | 28 (0.17) | 40 (0.19) | 23 (0.21) | 15 (0.14) |
| Individual history of colorectal adenoma | 39 (0.09) | 23 (0.09) | 16 (0.10) | 20 (0.08) | 19(0.12) | 20 (0.10) | 9 (0.08) | 10 (0.10) |
| Individual history of inflammatory bowel disease b | 113 (0.27) | 70 (0.26) | 43 (0.28) | 63 (0.25) | 50 (0.31) | 77 (0.38) | 21 (0.19) | 15 (0.14) |
a Values are indicated as No. (%).
b Indicates significance for residence.
c Indicates significance for sex.
d Indicates significance for age.
Further, no significant difference was observed between the two genders in terms of the prevalence of the other symptoms and risk factors such as lower gastrointestinal bleeding (rectal bleeding) in the last month, more than 10% weight loss during the last 6 months, as well as the personal history of CRC, colorectal adenoma, and inflammatory bowel disease (Crohn's disease or ulcerative colitis).
Furthermore, constipation and CRC family history among the first- and second-degree relatives were determined as the most common symptoms and risk factors among the urban, rural, and suburban populations in Arak, respectively. In this regard, a significant difference was reported between various residences (P ≤ 0.001) so that the symptoms and risk factors were less among the villagers.
The gastrointestinal bleeding and the personal history of inflammatory bowel disease were prevalent among the suburban and urban populations, respectively, the rate of which was significantly different from that of the others (P ≤ 0.001).
Based on the results, no significant difference was observed between the symptoms and risk factors among the individuals under and above 60 years old, whereas CRC family history among the second-degree relatives under 50 years old was more common in the age range of under 60 years old (P ≤ 0.012).
As shown in Table 3, 41838 individuals referred for screening since the beginning of the program implementation in 2019, among whom 30584 (73.1%) were normal based on the CRC screening guideline. The FIT test was requested for 8889 individuals (21.2%), among whom 2365 (5.7%) were guided to the physician for further evaluations based on the FIT test result, as well as the indicated risk factors and symptoms. The frequency distribution of detections by gender and age range is presented in Table 3.
| Diagnosis | Total | Sex | Age | ||
|---|---|---|---|---|---|
| Female | Male | < 60 | ≥ 60 | ||
| Normal | 30584 (73.1) | 19160 (72.4) | 11424 (74.2) | 18870 (73.6) | 11714 (72.2) |
| Need the result of FIT test | 8889 (21.2) | 5657 (21.4) | 3232 (21.0) | 5333 (20.8) | 3556 (21.9) |
| Suspected of colorectal cancer, requires referral for further investigation based on FIT test results and risk factors | 2365 (5.7) | 1630 (6.2) | 735 (4.8) | 1419 (5.5) | 946 (5.8) |
a Values are indicated as No. (%).
Table 4 represents CRC frequency among the individuals aged 50 to 70 years old covered by the health centers in Arak based on the pathology and hospital reports in the follow-ups performed by the experts employed in health care centers regarding the status of those referred for further assessments, as well as the results of the definitive diagnosis of their disease.
| Year | Total | Sex | Age | ||
|---|---|---|---|---|---|
| Female | Male | < 60 | ≥ 60 | ||
| 2016 | 33 (20.4) | 16 (21.3) | 17 (19.5) | 19 (25.0) | 14 (16.3) |
| 2017 | 38 (23.5) | 22 (29.3) | 16 (18.4) | 16 (21.1) | 22 (25.6) |
| 2018 | 41 (25.3) | 16 (21.3) | 25 (28.7) | 17 (22.4) | 24 (27.9) |
| 2019 | 50 (30.9) | 21 (28.0) | 29 (33.3) | 24 (31.6) | 26 (30.2) |
| Total | 162 (100) | 75 (100) | 87 (100) | 76 (100) | 86 (100) |
a Values are indicated as No. (%).
Table 5 presents the mean (SD) age of patients with CRC by gender and year. As displayed, the mean (SD) age is 59.72 (5.56) years. In addition, the mean (SD) ages for men and women are 59.91 (5.50) and 59.49 (5.66) years, respectively.
| Year | Age | Gender | |
|---|---|---|---|
| Female | Male | ||
| 2016 | 59.15(5.47) | 58.44 (4.80) | 59.82 (6.09) |
| 2017 | 59.95 (5.15) | 59.73 (5.51) | 60.25 (4.77) |
| 2018 | 60.56 (6.18) | 60.63 (6.18) | 60.52 (6.31) |
| 2019 | 59.22 (5.44) | 59.19 (6.20) | 59.24 (4.94) |
| Total | 59.72 (5.56) | 59.49 (5.66) | 59.91 (5.50) |
a Values are indicated as mean (SD).
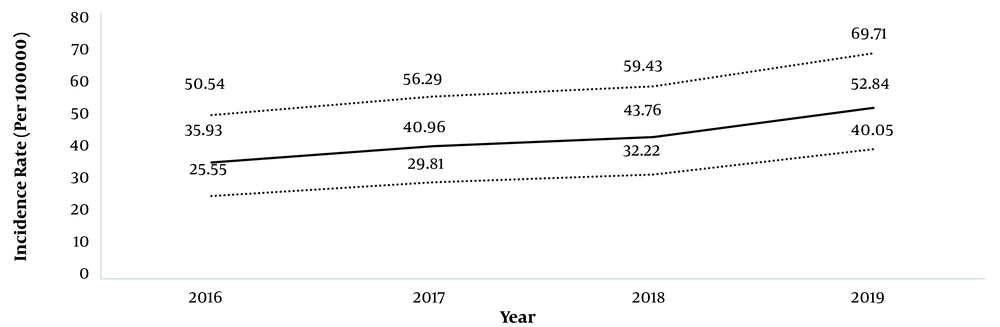
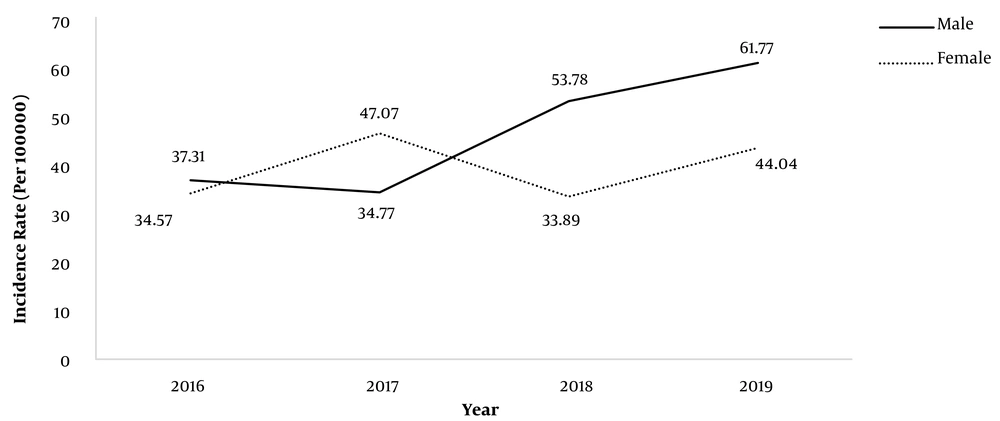
As demonstrated in Figures 1 and 2, an increasing trend is observed in CRC Crude incidence rate among the intended populations aged 50 to 70 from 2016 to 2019. Further, the CRC Crude incidence rates were 35.93 (95% CI: 25.55 - 50.54), 40.96 (95% CI: 29.81 - 56.29), 43.76 (95% CI: 32.22 - 59.43), and 52.84 (95% CI: 40.05 - 69.71) per 100000 individuals during 2016, 2017, 2018, and 2019, respectively (Figure 1).
5. Discussion
The present study aimed at assessing the frequency of CRC symptoms and risk factors among the populations aged 50 to 70 based on the report of the Sib system, as well as their participation rate in the screening program and CRC incidence rate in the age range. The participation rate of the individuals aged 50 to 70 years old in the CRC screening program covered by the health centers in Arak was 44.2%, which was maximized among the villagers (93.7%) and women. Zarychanski (15) reported the participation history in the CRC screening program among 23.5% of the subjects aged 50 years old and older individuals in the different states of Canada (15). According to Navarro et al. (16), women participate more in the program (16), which is consistent with the result of the present study. The higher participation of women can be related to an increase in their awareness about the importance of other screening programs such as breast cancer (16). In the present study, the number of CRC cases was higher among men compared to women. Thus, their awareness should be enhanced by encouraging them to participate in screening programs. The results of a systematic review represented the weakness in the CRC screening awareness, attitude, and behavior in Iran (17). Accordingly, evaluating the barriers and facilitators of CRC screening among the populations is regarded as essential due to the low tendency to the cancer screening, as well as the small participation of moderate-risk individuals (17-19).
Based on the results, constipation and CRC family history were considered the most common complaints of those referred for screening. Wong et al. (20) referred to genetic, family history, ethnicity, and age, as well as lifestyle factors such as diet, physical activity, alcohol consumption, smoking, weight, and chronic diseases as CRC risk factors among Asian populations (20). Based on the results of a systematic review, high consumption of red meat and convenience foods, low consumption of fruits and vegetables, as well as diabetes, obesity, positive CRC family history were among the most important CRC risk factors (10). More precise planning is required to control CRC in the future due to the difference in CRC incidence and risk factors in the various areas of Iran (10).
In addition, the mean ± SD age of CRC was 59.57 ± 5.54 years. In another study, Sabouri et al. (21) evaluated the patients with the mean age of 56.4 ± 14.6 years (21), whose age range was in line with that of most of the studies conducted in Iran.
Further, an increasing trend was attained regarding CRC incidence in Iran from 2016 to 2019, which was consistent with most of the recent studies (5, 6, 11, 22-24). According to Khosravi Shadmani et al. (13), the maximum CRC incidence is related to the central, northern, and western areas of Iran. They reported the age-standardized rate of CRC incidence among the women and men living in Markazi Province as 6.93 and 8.23, respectively, during 2008 (13). In the present study, a higher incidence was achieved due to the calculation based on the populations aged 50 to 70 years old and cancer definitive results (pathology or hospital report) collected from the intended health care centers and integrated with the cancer screening unit in the health centers in Arak. However, other studies indicated that the incidence in the whole population and its rate was low in some age ranges, leading to a less rate.
Expanding the early diagnosis and screening programs for CRC, and attracting the greater participation of individuals in the screening programs are regarded as essential due to the increasing trend of CRC incidence. Furthermore, the individuals should be trained to enhance awareness and recognition regarding CRC risk factors and symptoms, as well as understanding the necessity of performing periodic screening, especially among high-risk groups.
The limitations of the present study are as follows. All of the results of physical examinations and cases guided to the physician were not recorded completely and precisely in the Sib system. In addition, only the subjects referred for FIT, and those who needed more evaluations based on the results and risk factors could be reported during assessing FIT results from the Sib system. Further, it seems that the family physician failed to register precisely all of the reports related to the examinations of CRC-suspected individuals due to the volume of his/her duties. The results related to the cases referred to the second level could not be followed through the system due to the lack of a connection between the Sib system and the second referral level. Accordingly, they were collected by following the referred patients by health care providers and health workers.
Thus, upgrading electronic infrastructures and connecting the Sib system with the second-referral level is necessary for facilitating access to the results of the second level-referred ones. Finally, the forms for reporting the CRC-suspected cases related to the health care provider, health worker, and physician were overlapped. Therefore, the forms should be reviewed and the overlapped items should be integrated for allowing the physician to assess more specialized items among the patients at the minimum time and record the results in the system to obtain more citable and credible responses in the reports.
5.1. Conclusions
The results represented the low participation of individuals in the CRC screening program. In addition, constipation (change in defecation) and CRC family history were determined as the most common symptoms and risk factors among CRC-suspected individuals. Informing about recognizing risk factors and symptoms, as well as the necessity of timely referral for screening, was considered essential since the trend of CRC incidence increased among the populations aged 50 to 70 years old. In the current screening program, the electronic infrastructures of the Sib system should be upgraded and connected to the second referral level for facilitating the follow-up of referral results.