1. Introduction
Primary malignant melanomas (MM) of the female urogenital tract are extremely rare and aggressive neoplasms (1). The majority of genital tract melanomas occur in postmenopausal women, originate from the vulva and vagina, and involvement of the uterus, cervix, and ovary is exceedingly uncommon (2, 3). Herein, we report a case of primary MM of uterine cervix metastatic to internal and external genital organs, which has been treated with low anterior exenteration, pelvic radiation therapy, and immunotherapy.
2. Case Presentation
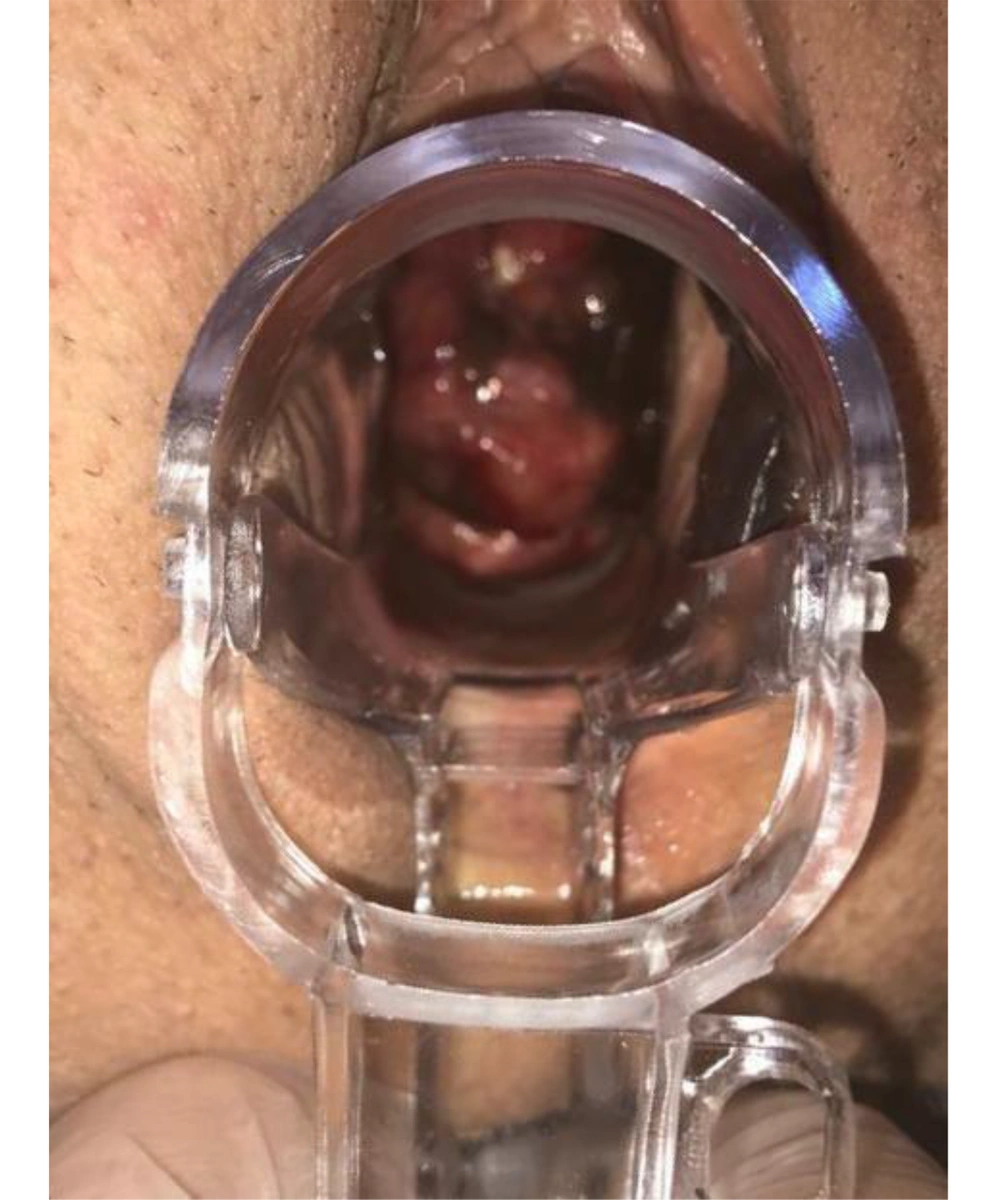
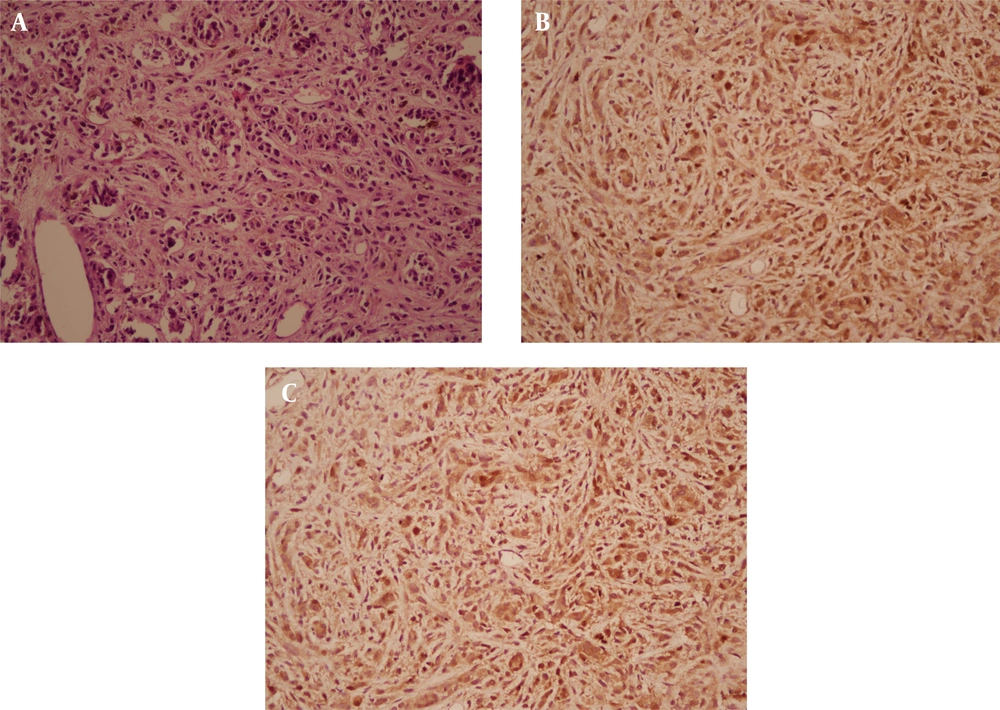
A 71-year-old healthy multiparous woman presented with a mass-like sensation in her vagina for the past 2 months. Her pelvic examination revealed a 4 cm blackish-pigmented tumor based on the cervix and multiple small blackish-pigmented lesions were found throughout the vaginal wall, spreading to the lower third of the vagina, and disseminated black lesion in the labia minora especially the inner part, vulvar vestibule and periurethral (Figure 1). We performed a cervical punch biopsy and its pathologic examination showed MM (Figure 2A). Immunohistochemistry showed strong positivity for HMB-45 and Melan A (Figure 2B) and S100 (Figure 2C). Her full body inspection to rule out the presence of any other suspicious lesions was negative. Her abdominal and pelvic magnetic resonance imaging did not demonstrate inguinal or pelvic lymphadenopathy or any signs of intraabdominal metastasis. Computed tomography of her chest also releveled no signs of distant metastasis. The patient underwent a low anterior pelvic exenteration including (abdominal radical hysterectomy, bilateral salpingo-oophorectomy, pelvic lymphadenectomy, bladder resection, total vaginectomy, and radical vulvectomy) without any major complication and no residual disease (Figure 3). Reconstruction of the urinary tracts was carried out with an Indian pouch operation. The operative time was 400 minutes and the estimated blood loss was 1550 mL. She received 3 units of packed RBC during the operation and in recovery. Histological examination confirmed malignant melanoma originating from the cervix. The tumor size of the exocervix was 4 × 4 × 4 cm and extended to the endocervical canal. Melanoma in situ was present in the cervix with the mitotic rate of 46/10 HPF = 23/mm2. Lymphovascular invasion was positive and there was the involvement of the vagina, vulva with free labial margin, total uterine endometrium and myometrium, bladder serosa, and urethral margin. Also, there was the involvement of 1 pelvic lymph node. The ovaries, fallopian tubes, and bladder wall were free of tumors. Histopathologically, this was a FIGO stage of III-A. The patient was hospitalized for 10 days after surgery and her postoperative course was complicated with transient ileus, which resolved with conservative management.
A, section shows infiltration of isolated and small nests of atypical cells with hyperchromatic nuclei, anisonucleosis and irregular nuclear border. There is also brown pigment in cytoplasm of some of the atypical cells (Hematoxylin and EosinX200); B, positive diffusely for the cocktail of HMB45 and Melan A markers (X200); C, positive diffusely for S100 marker (X200)
Subsequently, 4 weeks after surgery, she started to receive 25-course radiotherapy (external beam radiotherapy below the pelvic brim to pelvic lymph nodes and perineum) and later immunotherapy by interferon-alpha (IFN-α), which has been continued for 6 months. She has been scheduled for follow-up in 3 monthly intervals with performing lung CT scan and abdominopelvic CT and brains MRI, the results of which were negative for disease progression until 6 months after completing radiotherapy. Now, she is active in her daily life, 1 year following her diagnosis. All data are published after taking patient consent.
3. Discussion
Primary cervical MM is an extremely rare malignancy, which accounts for 3% to 9% of all MM of the female genital tract (1). The overall median age at diagnosis is 59 years old, and almost two-thirds of the patients are over 50 years old (2, 3). The most common symptoms of cervical MM are vaginal bleeding, vaginal discharge, abdominal pain, dyspareunia, and post-coital bleeding (4). Cervical MM usually remains asymptomatic until the ulceration and infection of the tumor revealed the symptoms (3). In the present case, the patient had a fullness sensation inside the vagina with no vaginal bleeding may be due to a non-ulcerative cervix. The diagnosis is based on a gynecologic examination, colposcopy, and biopsy for pathology evaluation. Also, they may be diagnosed with a routine pap smear, which reveals findings ranging from oval and polygonal to spindle-shaped cells. On examination, it reveals a mass-like lesion, which is an exophytic, polypoid, or ulcerated nodule with a size range of 0.5 cm to 9 cm (2, 5). The pathology evaluation is made by immunostaining as MMs are frequently positive for S100, vimentin, melanin A, MART1, and HMB 45. Among these markers, S100 is more sensitive and HMB45 is more specific, especially in the combination with each other (6). In pathology examination, there are 4 diagnostic criteria for valid cervical MM including (a) the presence of melanin in the cervical epithelium; (b) the absence of melanoma in other sites of the body; (c) evidence of junctional activity in cervical epithelium near to lesion; (d) metastases according to the cervical carcinoma pattern (3, 7). The best treatment approach for cervical MM is a matter of debate due to its rarity. But, surgery is the cornerstone of treatment, which includes radical hysterectomy, pelvic lymphadenectomy, and partial vaginectomy with a free margin of 2 cm in stage I-II disease and pelvic exenteration in locally advanced stages. However, some authors advise performing lymphadenectomy in cases with bulky lymph nodes (2). According to a literature review by Pusceddu et al., most cases with cervical MM initially underwent surgery, which at least was total abdominal hysterectomy and bilateral oophorectomy (3). In our case, we selected low anterior pelvic exenteration, total vaginectomy, and wide local excision of the vulva according to diffuse spread of tumor beyond the vagina, vulva in internal part of labia minor and urethral margin. Similar to our case, Clark et al. described a cervical MM in FIGO stage IIIB, which underwent total pelvic exenteration (8). Malignant melanoma is a proven radio-resistant tumor. However, adjuvant pelvic radiotherapy might be considered in patients with positive surgical margins, parametrium involvement, and histologically positive lymph nodes, where it is used in patients with contraindications of radical surgery in means of palliative treatment (6). The use of adjuvant chemotherapy is not effective in improving progression-free survival and overall survival. Recently immunotherapy agents such as INF-a, IL-2, and bio chemotherapy in combination with the mentioned drugs achieved disappointing results in advanced cases. Target therapy is another novel option for treatment in MM. One of immunotherapy agents are programmed cell death-1 (PD-1) and PD-ligand (PD-L1) inhibitors, which blocks the interaction between PD-1 and its ligands. However, there is still not good evidence in the therapeutic role of these agents in MM of female genital tract (2, 9). Cervical MM prognosis is very poor according to its diagnosis in advanced stages of disease. Recent review estimated the 5-year survival about 18.8 % for stages I, 11.1% for stage II, and 0% for stage III, IV (1). In our case due to diffused involvement of genital tract, we decided to perform pelvic exenteration followed by radiotherapy and INF-a, which to date, progression free survival in our patient is 6 months and overall survival is 7 months fallowing her radiotherapy. In the literature, we found a case report by Myriokefalitaki et al., which reported a patient with cervical MM spread to vagina, which had been operated by pelvic exenteration and they achieved good result of no recurrence after 8 years of fallowing up (6). We suggest to consider this surgical management and RT and using INF-a (less insure to efficacy of this drug) for primary and locally advanced disease of cervical MM as initial approach. When feasible, pelvic exenteration offers an appropriate initial management in cervical MM. It is necessary to follow up patients in long-term period and collaborative studies between all oncologist’s specialist to achieve improvement in treatment of this rare and aggressive disease.