1. Background
Breast cancer is the most frequently diagnosed cancer all around the world as well as the leading cause of death in women (1).
The most important independent factor that can predict the survival and risk of recurrence in patients with breast cancer is the histopathologic status of axillary lymph nodes (2). Accordingly, axillary lymph node dissection has been considered a routine part of the management for patients with early breast cancer. This method affects disease control, has a high prognostic value, and guides treatment selection for the patients (3). However, it causes anatomic disruption and can be associated with complications, such as lymphedema, nerve injury, and shoulder dysfunction, which can diminish functionality of the patients and affect the quality of their life (4).
Axillary lymph node dissection is still the standard procedure performed for women with clinically palpable axillary nodes or positive nodes confirmed by methods, such as ultrasound guided fine needle aspiration (5). Recently emerged as an accepted substitute for axillary dissection in staging breast cancer in patients with clinically negative axillary nodes, sentinel lymph node (SLN) biopsy yields a high accuracy with a low false negative rate and is associated with less morbidity while performed by an experienced physician (6, 7).
The pathologic evidence of axillary metastasis will only be present in approximately 30% of patients with T1-2, n0 breast carcinomas (6, 8). Although frozen section is known to be less accurate than permanent section analysis, it can help avoid a second surgical intervention for axillary lymph node dissection in patients with positive metastases (9).
SLN has been shown, by various studies, to have a high detection rate and an acceptable accuracy for predicting axillary lymph node status (10-13); however, few studies have compared its compatibility with the results of permanent section analysis in breast cancer. Therefore, the present study aims at investigating the compatibility of intraoperative frozen section analysis with permanent section analysis of SLN in patients who had been referred to Shohadaye Tajrish Hospital during 2008 - 2014 with a diagnosis of breast cancer.
2. Methods
In this descriptive retrospective study, patients with definite diagnosis of breast cancer, made through histopathological assessment, were identified by reviewing the archives of pathology reports documented in the department of pathology of Shohadaye Tajrish hospital during 2008 - 2014. Of these patients, those who had undergone intraoperative frozen section analysis of the SLN biopsy and had had a report of a permanent section analysis were included as the study population, using a convenience sampling method.
Hence, the inclusion criteria of the study included making a definite diagnosis of breast cancer made through histopathological assessment, having undergone intraoperative frozen section analysis of the SLN biopsy, and having the patient’s permanent section analysis report. Incomplete medical record was also considered the exclusion criteria.
For pathological assessments, lymph nodes were obtained fresh, and after sampling, were frozen as quickly as possible at temperature -20°C to -30°C. Then, the prepared slides were stained according to the standard protocol of Hematoxylin and Eosin (H and E) staining.
The sentinel nodes would be considered negative on frozen section if we were not able to find tumoral involvement in at least three-step sections stained with H&E. Immune staining for Keratin was not performed on the specimens during intraoperative consultation.
The data of frozen section and permanent section analyses were extracted from the medical records and processed by SPSS (statistical software v.22) (14). The results of analyses were recorded as dichotomous variables of positive and negative states and their compatibility were compared, using Pearson’s correlation analysis. Sensitivity, specificity, negative predictive value and positive predictive value were, then, calculated accordingly. A P value of less than 0.05 was considered statistically significant in all analyses.
The patients’ information was remained confidential throughout the survey and the extracted data were used anonymously. The study protocol was evaluated and approved by the ethics committee of Shahid Beheshti University of Medical Sciences.
3. Results
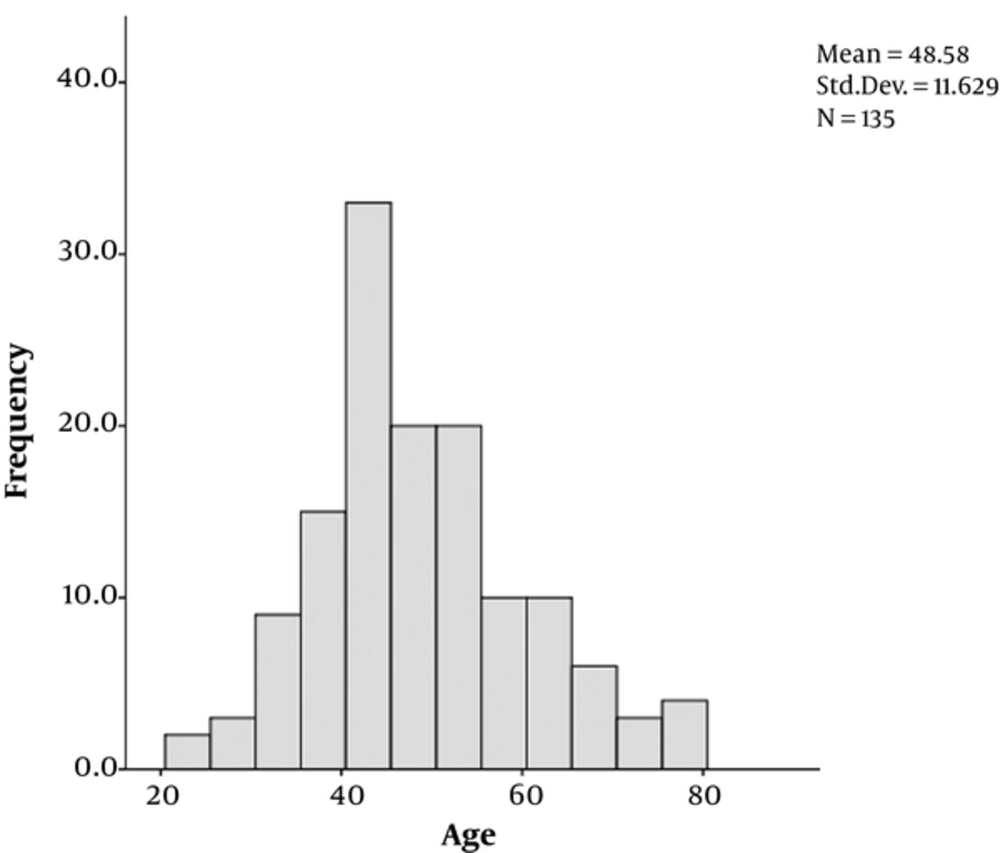
A total of 135 eligible women diagnosed with breast cancer and recorded frozen section analysis of SLN and permanent section analysis were included in this study. The mean age of the subjects was calculated to be 48.85 ± 11.62 years with a minimum of 23 and a maximum of 79 years. Figure 1 depicts the age distribution of the study population.
The frozen section analysis of SLN biopsies was positive in 38 patients (28.1%) and negative in 97 (71.9%), while the results of permanent section analysis was positive in 44 (32.6%) and negative in 91 subjects (67.4%) (Table 1).
| Variable | Number / Mean |
|---|---|
| Age (mean ± standard deviation) | 48.85 ± 11.63 years |
| Frozen section analysis | |
| Positive | 38 (28.1%) |
| Negative | 97 (71.9%) |
| Permanent section analysis | |
| Positive | 44 (32.6%) |
| Negative | 91 (67.4%) |
Table 2 presents the correlation between 2 histological analyses performed for the patients. Based on these results, frozen section analysis of SLN biopsy accurately identified 36 positive cases and 89 negative cases; thus, the overall accuracy of this method is 92.6%. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated to be 81.8%, 97.8%, 94.7%, and 91.7%, respectively. The false negative rate (1-sensitivity) and false negative predictive value (1-NPV) were also found to be 18.2% and 8.3%, respectively.
The correlation between these 2 analyses was evaluated and it was found to be statistically significant with a Pearson’s correlation coefficient of 0.830 (P < 0.001).
| Permanent Section | Total | |||
|---|---|---|---|---|
| Positive | Negative | |||
| Frozen section | Positive | 36 | 2 | 38 |
| Negative | 8 | 89 | 97 | |
| Total | 44 | 91 | 135 | |
4. Discussion
Based on the results of the present study, a significant correlation was found between frozen section and permanent section analyses. Although the diagnostic characteristics calculated for frozen section analysis confirm the usefulness of this method in patients with breast cancer, the small risk of false positive results (1.5%) should also be recognized. However, 81.8% (36 out of 44) of the patients who are spared the need for reoperation seem to outweigh the mentioned small risk.
In recent decades, a growing tendency towards less invasive procedures has been observed in the treatment of breast cancer inasmuch as currently more than 50% of these patients undergo breast-conserving surgeries instead of extensive total and radical mastectomies (15). Accordingly, in the early stages of cancer axillary lymph node, biopsy and pathologic evaluation of the specimens are performed as a superior method to completion dissection of these nodes, which is accompanied by multiple debilitating complications. In this setting, patients with positive lymph nodes require re-operative lymphadenectomy. To spare the need for such interventions in these patients, intraoperative frozen section analysis of SLN biopsy is introduced as an alternative method so that patients with positive SLN biopsies would undergo lymphadenectomy in their first surgery and would not need a reoperation (6, 7).
Table 3 presents the results of previous studies on the accuracy of SLN frozen section analysis in breast cancer. As can be seen, discrepancies are observed among the results of these studies. These differences can be attributed to the various clinical and pathological factors that affect the accuracy of frozen section analysis. For instance, nodal metastases from infiltrating ductal carcinomas are generally considered easier to visualize than those from invasive lobular carcinomas (9, 16). The tumor size is another factor that might affect the accuracy; the false negative rate might decrease with increasing tumor size (17). Technical issues can also affect the results yielded from frozen section analysis. Although the differences can be minimized by employing the proper techniques and appropriate experience, some tissues still may be lost during the frozen section processes and cause the diagnosis to be missed due to a suboptimal technique (16, 18-21). The number of frozen section levels examined is another factor that can influence the accuracy of the procedure (16). An increase in sampling nodal sections can also improve the accuracy and sensitivity of frozen section analysis, but it may be impractical, since it consumes much more time than the routine protocol for this means (22, 23). And finally, expertise of the operator is also of utmost importance in the results of analyses (16, 18).
| Authors | Number of Patients | Accuracy | Sensitivity | NPV |
|---|---|---|---|---|
| Cavanese et al. (24) | 96 | 91% | 73% | 88% |
| Turner et al. (16) | 278 | 93.2% | 73.9% | 91.6% |
| Veronesi et al. (22) | 119 | 97% | 94.5% | 95.5% |
| Hingston et al. (25) | 97 | 95% | 89% | 96% |
| Van Diest et al. (19) | 54 | 95% | 87% | 93.5% |
| Zurrida et al. (23) | 192 | 86% | 68% | 81% |
| Weiser et al. (17) | 890 | 89% | 58% | 87.3% |
| Rahusen et al. (18) | 100 | 84% | 57% | 80% |
| Chao et al. (9) | 200 | 92.6% | 67.9% | 89.8% |
| Current study | 135 | 92.6% | 81.8% | 91.7% |
Despite the discrepancies observed among these studies, all of them are indicative of the fact that frozen section analysis of SLN is generally accurate for breast cancer and can be used to determine the need for immediate axillary dissection and it can spare patients with positive results, the need for reoperation.