1. Background
The DNA mismatch repair (MMR) system is responsible for correcting genetic errors in the coding and non-coding DNA regions throughout the genome (1). However, when the MMR system is defected, these errors could pass to the next generation of cells. MMR system deficiency may lead to genetically uncorrected cellular proliferation and, consequently, to the development of a number of neoplasms in the human body (2). Microsatellites are small, repetitive sequences of DNA, consisting of 1- to 6-base pairs that are distributed throughout the human genome. When the defined number of each microsatellite is altered, through insertion or deletion of 1 or more base pairs, it is called microsatellite instability (3). Microsatellite instability (MSI) is a reflection of the defects in a DNA mismatch repair system.
The most well-established link between MSI and malignant neoplasm has been reported in colorectal cancers, where 15% to 20% of sporadic tumors are MSI related (4). Another less studied, yet important neoplasm that has been associated with MSI is ovarian epithelial cancer, which is the fifth most common cancer among women worldwide. Ovarian cancers are commonly diagnosed at later stages, and are among the most deadly gynecological malignancies in women (5). Limited studies in our country have investigated the etiology and prognosis of this type of malignancy. Therefore, in ovarian carcinomas, molecular and genetic prognostic and predictive factors, including DNA mismatch repair system and its reflection, MSI, are worth investigating.
Ovarian cancers that are associated with MSI, like other organs with similar genetically based errors, may have distinct characteristics in terms of age at presentation, mortality rate, and response to standard chemotherapeutical regimens.
MMR-related colon cancers have better prognosis compared to those without this genetic defect (3). The same phenomenon may be true with ovarian cancers. Classic platinum-based chemotherapies are the mainstay in the treatment of both early and advanced carcinomas. Nevertheless, some studies have shown, although not definitively, that these particular types of cancer may show some sort of resistance to routine chemotherapy regimens, including platinum (cisplatin and carboplatin) and taxane (paclitaxel) (6). Hence, the detection of the underlying MMR system defects in ovarian epithelial neoplasms may lead clinicians to select more efficacious treatment strategies, alongside better imagination of the natural course of the disease.
To date, no study has been conducted in Iranian, and even among Middle Eastern populations, to determine the prevalence and associated factors of microsatellite instability in ovarian epithelial carcinomas. Given the different outcomes described for these types of tumors, this study could provide a clearer picture of ovarian epithelial cancers’ profile in the Iranian population.
2. Methods
2.1. Preparation of Samples
In this study, the specimens with previously confirmed diagnosis of ovarian epithelial carcinoma, from 2010 to 2014, were retrieved from the archives and prepared for molecular studies. The patients had given informed consents at the time of admission in order that their specimens in pathology laboratory would be available for research purposes in future. Institutional review board and ethics committee confirmed the study design. First, authors reviewed all slides and the original paraffin-embedded tissue blocks were sent to the molecular pathology laboratory. The samples were prepared as three 5-micrometer thick slices from tumor tissue. The first 2 slices were sent for DNA extraction and the third was stained with H&E to confirm the presence of tumor in the sliced areas. A sample would be excluded if the DNA extraction failed or if there was no tumor cell present in the light microscopic evaluation. In order to prevent contamination of samples, each slice was cut by a new blade and, then, the slices were transferred to 1.5-mL Eppendorf tubes by disposable applicators. Subsequently, paraffin was removed by adding xylene and the samples were washed with pure ethanol. In the next step, tissue lysis buffer and proteinase K were added to microtubes and were placed at a temperature of 55°C. After complete dissolution of all the tissue fragments, a binding buffer, isopropanol, and an inhibitor-removal buffer were added and centrifuged briefly. Finally, the tumor DNA was purified, using DNA extraction kit (Roche diagnostics GmbH, Mannheim, Germany). The extracted tumor DNA was diluted to 1:10 by adding elution buffer.
2.2. Microsatellite Analysis
Forward and reverse primers for amplification of sequences NR27, BAT26, BAT25 NR24, and NR21 were ordered at Macrogen (Geum Chun-Gu, Seoul, Korea) with their previously defined sequences (7). The PCR for target sequences was performed in 20 µL reaction containing 10 µL of 2x SYBER premix ex Taq master mix (Takara Bio, Ostu, Shiga, Japan), 1 µL of forward and reverse primers with concentration of 10 PM/µL, and about 50 ng extracted tumor DNA. Finally, the PCR reaction was performed in light cycler Nano machine (Roche diagnostics GmbH, Mannheim, Germany) with PCR condition, being initial denaturation at 94°C for 0.5 minutes; then, 45 two-step cycles as follows: 95°C for 10 seconds; and 60°C for 30 seconds. Finally, a 5-minutes terminal extension was performed at 72°C, followed by a melting analysis of the PCR product. The melting graphs were assessed, and if acceptable, the samples were sent to Macrogen (Geum chun-gu, Seoul, Korea) for capillary electrophoresis. The results of electrophoresis were analyzed, using peck scanner software version 1.0 (applied biosystems, CA, USA). Instability in 2 or more markers was considered MSI-H, and instability in 1 marker was considered MSI-L.
2.3. Immunohistochemistry
IHC staining was carried out on the MSI-H specimen with anti-MLH1, MSH2, MSH6, and PMS2 antibodies (Dako, Glostrup, Denmark).
2.4. Statistical Analysis
To analyze the correlations of microsatellite instability with histological grade, FIGO stage, tumor laterality, and omental involvement among ovarian carcinomas, Chi-squared tests were carried out. P value < 0.05 was regarded as statistically significant.
3. Results
In this study, the specimens belonging to 37 malignant ovarian epithelial tumors were assessed for microsatellite instability. The mean age of the patients was 45.13 ± 9.50. The mean size of the tumors was 11.40 ± 5.96 cm. Nineteen tumors (51.4%) were unilateral. Among various histological types, serous adenocarcinoma was the predominant type, with 54.1% of all carcinomas, while others were endometrioid with 21.6%, clear-cell with 13.5%, and mucinous with 10.8%. Based on the world health organization (WHO) classification for histological grading, 61.1% were high grade, while 16.7% and 22.2% were low and intermediate grade, respectively. According to the FIGO staging system, 47.2%, 5.6%, and 47.2% of the tumors were stage I, II, and III, respectively. About 43% of the tumors were associated with omental involvement.
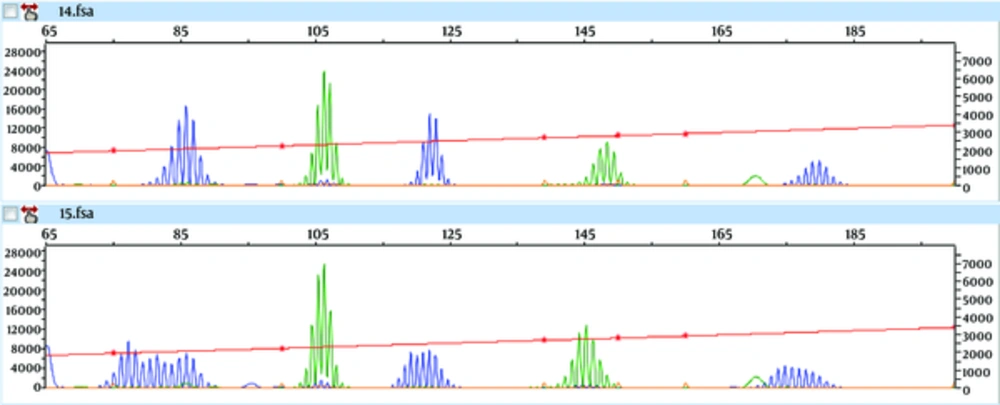
Of our specimens, only 4 out of 37 (10.8) were microsatellite unstable (CI95% = 2.7 - 21.6). The rate of MSI-H and MSI-L were 2.7% (1.37) and 8.1% (3.37), respectively. The only tumor with MSI-H, in which capillary electrophoresis graph shows instability in BAT26, NR24, NR27 (Figure 1), was a unilateral, 9 cm, Grade II endometrioid adenocarcinoma, with FIGO stage IIB, and without omental involvement. Shown in Table 1, the rate of microsatellite instability is higher among patients under 45, with larger than 10 cm, and unilateral tumors, compared to older women, who had smaller and bilateral tumors. One of the major endpoints of this study was the assessment of the relationship between MSI status with tumor histological type, grade, and FIGO stage. Our study showed that microsatellite instability was more prevalent in non-serous, low-intermediate grade, and stage I neoplasms. Also, the MSI was more pronounced in cases with no omental involvement. According to a significance level of 0.05, the histological type was the only parameter having a significant relationship with the MSI tumors.
| Characteristic | Microsatellite Instability, N (%) | Microsatellite Stable, N (%) | P Value | ||
|---|---|---|---|---|---|
| High | Low | Total | |||
| Age group | 0.99 | ||||
| < 45 Years | 1 (6.2%) | 1 (6.2%) | 2 (12.5%) | 14 (87.5%) | |
| > or = 45 Years | - | 2 (9.5%) | 2 (9.5%) | 19 (90.5%) | |
| Size | 0.6 | ||||
| < 10 cm | 1 (5.9%) | - | 1 (5.9%) | 16 (94.1%) | |
| > or = 10 cm | - | 3 (15.0%) | 3 (15.0%) | 17 (85.0%) | |
| Side | 0.1 | ||||
| Unilateral | 1 (5.3%) | 3 (15.8%) | 4 (21.1%) | 15 (78.9%) | |
| Bilateral | - | - | 0 (0%) | 18 (100%) | |
| Histologic type | 0.036 | ||||
| Serous | - | - | 0 (0%) | 20 (100%) | |
| Non-serous | 1 (5.9%) | 3 (17.6%) | 4 (23.5%) | 13 (76.5%) | |
| Histologic grading | 0.63 | ||||
| Low to moderate | 1 (7.1%) | 1 (7.1%) | 2 (14.3%) | 12 (85.7%) | |
| High | - | 2 (9.1%) | 2 (9.1%) | 20 (90.9%) | |
| FIGO staging | 0.32 | ||||
| I | - | 3 (17.6%) | 3 (17.6%) | 14 (82.4%) | |
| II or III | 1 (5.3%) | - | 1 (5.3%) | 18 (94.7%) | |
| Omentum status | 0.11 | ||||
| Involved | - | - | 0 (0%) | 16 (100%) | |
| Free | 1 (5.0%) | 3 (15.0%) | 4 (20.0%) | 16 (80.0%) | |
The characteristics of microsatellite unstable ovarian epithelial cancers have been depicted in Table 2, where NR21 and BAT26 loci were predominant mutations, each found in the 2 cases.
| Age | Side | Size (cm) | Histology | Grade | FIGO Stage | Omentum | Mutant Mono/Dinucleotide | MS Status |
|---|---|---|---|---|---|---|---|---|
| 42 | Unilateral | 13 | Mucinous | Low | IA | Free | NR21 | MSI-L |
| 51 | Unilateral | 13 | Clear Cell | High | IA | Free | BAT26 | MSI-L |
| 48 | Unilateral | 11 | Clear Cell | High | IA | Free | NR21 | MSI-L |
| 35 | Unilateral | 9 | Endometrioid | Moderate | IIB | Free | BAT26, NR24, NR27 | MSI-H |
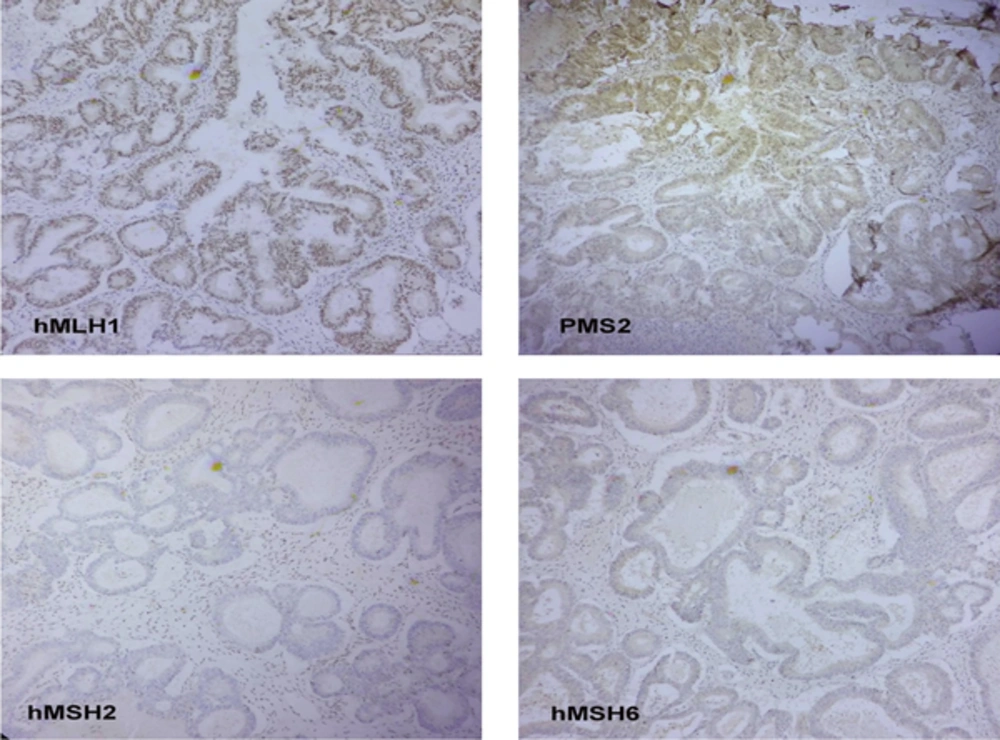
Nuclear immunoreactivity for hMLH1, hMSH2, hMSH6, and PMS2 proteins was performed on the only MSI-H tumor of our specimens. In addition, hMLH1 and PMS2 showed positive nuclear reaction, whereas hMSH2 and hMSH6 showed a negative result that is consistent with the molecular method (Figure 2).
4. Discussion
Generally, immunohistochemistry and molecular genetic studies have been used to assess MMR proteins or their coding genes. According to the literature, the MSI detection method has been the more cost-effective and accurate, along with the fact that it is suitable in clinical settings (8). Following an NCI workshop in 1977, Bethesda markers were introduced for the detection of MSI in colon cancer. Despite the well-known efficacy in colon carcinoma of Lynch syndrome, it remained uncertain whether these markers were the best option for assessing MMR-related ovarian cancers (4). We used 5 mononucleotide markers included in the MSI analysis system, of which BAT25 and BAT26 are shared with the Bethesda panel. Recent studies have shown that the use of pentaplex panel of mononucleotide markers show superior results in terms of sensitivity and specificity compared to NCI panel. Moreover, there is no need for simultaneous normal DNA matching because of the quasimonomorphic nature of pentaplex panel (9-12).
In our study, about 11% (CI95%: 2.7 - 21.6) of specimens were positive for MSI, of which, 3 were MSI-L and only 1 was MSI-H. Moreover, in other studies among non-selected cases of ovarian cancers, between 0% to 37% have been MSI-H positive (13). The wide range was due to differences in study design, number, and type of detector markers and the criteria for the definition of MSI-H (14, 15). However, in the studies using Bethesda panel markers or MSI analysis system, the rate of MMR system defects has been reported at about 10% (CI95% = 6 - 14) in ovarian epithelial cancers (16-18). Therefore, our results are consistent with previous findings regarding the overall rate of MSI in all histological types.
In previous reports, the overall rate of BAT25 and BAT26 positivity was 6.7% and 4.8%, respectively, using different MSI panels (16). Similarly, 5.4% of our samples were instable for BAT26, while none showed instability for BAT25.
In the present study, the prevalence of MSI was significantly higher among non-serous carcinomas, while all serous tumors were microsatellite stable. The only MSI-H case was an endometrioid adenocarcinoma (12.5% of this type). Other studies also pointed out that non-serous malignant ovarian tumors were more likely to be MSI positive (13). This finding is considered important because serous histology is the dominant type in all ovarian carcinomas (more than 50% in our study).
This higher rate of microsatellite instability among non-serous tumors can be explained by the fact that such ovarian tumors, endometrioid and mucinous in particular, may be metastatic sites of undiagnosed primary endometrial or colon cancers, and we know that the MMR defect is responsible for a considerable fraction of these carcinomas (14).
Immunohistochemical staining was performed on the only case that showed MSI-H in molecular method. This case showed negative reaction for MSH2 and MSH6, while it was positive for MLH1 and PMS2 that is consistent with a deficiency in the MMR system. Other studies have shown a frequency of about 6.4% loss in MLH1 or MSH2 in ovarian carcinomas (16). Meanwhile, the loss of MSH6 is more common in certain variants of ovarian carcinomas, such as clear-cell, endometrioid, and mucinous types (19).
4.1. Conclusions
In this study, we used microsatellite assay to find the genomic defects in DNA mismatch repair system. We could say that the DNA mismatch repair system defects, to which a small but critical fraction of ovarian epithelial carcinomas is attributable, deserve routine investigation. The latter is especially important in the case of non-serous ovarian epithelial cancers. Pathologists should be aware of the importance of reporting MSI as indicated, because it may help define the best treatment strategy for MMR defected cases.