1. Introduction
Gestational trophoblastic disease (GTD) includes hydatiform mole, choriocarcinoma, placental site trophoblastic tumor, and epithelial trophoblastic tumor (1). Also, molar pregnancy can happen as an ectopic pregnancy in the fallopian tube, cornea, and cervix. The coincidence of these complicated pregnancy cases seems to occur extremely rarely (1). To the best of our knowledge, there is only 5 heterotopic molar pregnancy (HMP) reported in the literature; moreover, pure heterotopic molar pregnancy has been reported once in the literature (2). This case report described a patient with heterotopic pregnancy with both intrauterine and ectopic fallopian tubes considered as complete molar pregnancy.
2. Case presentation
The patient was a 26-year-old nulli gravida woman who was referred to our center with the diagnosis of gestational trophoblastic neoplasia (GTN). Serum human chorionic gonadotropin (hCG) titer was 28000 mIU/mL. She underwent suction curettage in the 8th gestational week of pregnancy. Pathology examination confirmed a complete hydatiform mole. One week later, she had a second suction curettage due to an intrauterine tissue remnant of 25 mm and an inappropriate decrease of hCG to 25000 mIU/mL. However, no tissue was attained. During the second curettage follow-up, hCG titer remained plateau, so she was referred to our oncology department. According to the GTN diagnosis, we performed P/E including vaginal examination which was normal. Complete work up for GTN including complete blood cell count (CBC), liver/renal/thyroid function tests/chemistry profile, abdomino-pelvic, and lung computed tomography (CT) was done which was normal. The only symptoms of the disease were nausea and vomiting and mild lower right abdominal pain. We started chemotherapy with a multiday methotrexate regimen (for 7 days and repeated it every 3 weeks) due to post-molar and low-risk GTN. During chemotherapy, hCG decreased to 14000, but after receiving 2 courses of chemotherapy, it raised to 29500 and the patient came to our emergency department with severe right lower quadrant (RLQ) pain. Her vital signs were BP = 100/70 mmHg, PR = 120, RR = 17, and T = 37.1. In physical examination, she had severe RLQ tenderness and her vaginal examination was normal. Emergent pelvic sonography revealed a 9 × 3 × 2 cm vascular mass in the right fallopian tube, suggestive of ectopic pregnancy and moderate to severe free fluid in the abdominopelvic cavity. She underwent laparotomy immediately. There was about 700cc blood and clot in the abdominopelvic cavity, and the right tube was partially ruptured. The tube was full of vesicular tissue of molar pregnancy. A salpingectomy was performed. Pathologic examination revealed complete ectopic molar pregnancy. Twenty-four hours after surgery, hCG decreased to 5000 IU/L. In the weekly follow-up, after 1 week it reached 1000 mIU/mL, but then it remained at plateau levels after 3 consecutive weekly measurements. Thus, we restarted the multiday methotrexate (MTX) regimen. She showed a good response after 4 courses of chemotherapy, reaching to hCG level of 100 mIU/mL, but it remained plateau in the 3 next weeks of follow-up. Due to her poor response to MTX, we changed her regimen to dactinomycin (1.25 mg/m2, every 2 weeks). After receiving 2 courses of the dactinomycin regimen, the hCG level reached less than 5 mIU/mL, and totally she received 5 courses. Now, she is cured after 20 months after her last course of chemotherapy and is pregnant at the gestational age of 28 weeks without any major obstetrical complication. In order to publish all these data written informed consent was taken from the patient.
3. Discussion
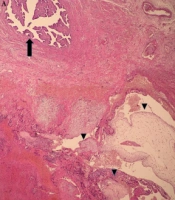
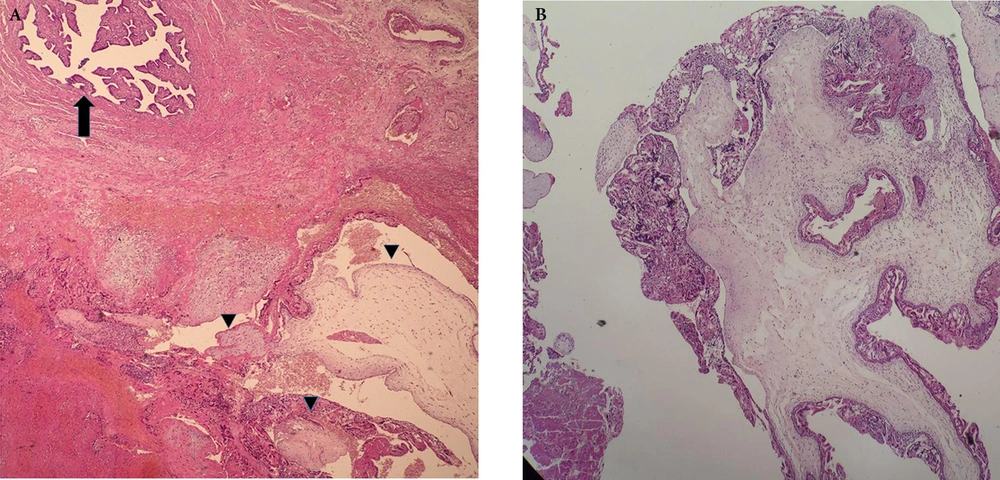
We reported an extremely rare heterotopic pregnancy (HP) with both intrauterine and ectopic complete hydatiform mole (CHM). Heterotopic pregnancy is rare. The incidence has been estimated at 1 in 30000 pregnancy cases. However, it is increased by the higher rate of associated reproductive technology, which is one of the risk factors of HP. Even more rare is HP which consists of molar pregnancy with non-molar pregnancy (3), and even more rare than a pure heterotopic molar pregnancy. Just one case of pure heterotopic molar pregnancy (intrauterine and ovary) has been reported in the literature (2). Diagnosis of HP is extremely difficult and about 50% of cases are diagnosed after tubal rupture (4). It seems that there is no distinguishing value by means of lab tests and signs and symptoms among tubal GTD and usual EP cases (1). However, HPs are diagnosed with higher levels of hCG, especially in CHM. In our case, the diagnosis of molar HP was made with delay, maybe due to receiving 3 courses of MTX therapy leading to tissue necrosis and prevention of fast and high increase. It is important to notice that maybe in ectopic molar pregnancies hCG level is less than the usual EP. It has been suggested by Chauhan et al. cited in Yamada et al. that tubal implantation may prevent adequate vascularization and lead to lower hCG levels in ectopic GTD (5). However, some studies have revealed that ectopic GTD has a higher probability of rupture at the time of presentation versus non-trophoblastic ectopic pregnancy. This may be the result of more trophoblastic tissue in GTD (5, 6). Management of heterotopic molar pregnancy includes evacuation of both intrauterine and ectopic moles. Preferable surgical method in non-molar EP is salpingostomy; however, medical literature prefers to perform salpingectomy rather than salpingostomy in molar EP, avoiding to molar tissue residual in tube (7, 8). As clinical and ultrasonographic results of ectopic molar pregnancy might be non-specific and mimic non-molar EP, it is so crucial to evaluate the tissues histopathologically to achieve an accurate diagnosis. Diagnosis of complete molar pregnancy is easier than partial mole. In macroscopic evaluation, the tissue is bulky and bloody with hydropic changes in all villi, presenting like vesicles, classically named bunch of grapes. Early complete moles may not have the features mentioned (9). In the case of our patient, the vesicular tissue was obvious within the tube. Microscopically diffuse swelling of the villi, diffuse trophoblastic hyperplasia and negative for P57 immuno-histochemical marker are characteristics of CHM (Figure 1A and B) (10). Close follow-up with weekly hCG titer for 3 normal values (less than 5 mIU/mL) and then monthly for 6 months is essential after surgical removal of the molar tissue. The risk of GTN following partial mole and the complete mole is 0.5% and 15%, respectively (11). As we observed in our case, even after salpingectomy, the hCG level decreased from 28500 to 5000, but in the follow-up, she received chemotherapy due to plateau levels of hCG and diagnosis of GTN. When GTN is diagnosed (hCG levels plateau in 4 weekly measurements over 3 weeks, rise in the hCG levels ≥ 10% in 3 measurements for 2 weeks, or abnormal hCG levels persistent over 6 months), it is necessary to repeat metastatic work-up and determine the FIGO stage and prognostic score. Metastatic work-up includes CBC differential and platelet count, liver, renal, thyroid function tests, chemistry profile, and imaging (chest, abdominal-pelvic CT scan with contrast, pelvic ultrasound or magnetic resonance imaging (MRI), and brain MRI if pulmonary metastases are present (12). Our patient was in FIGO stage I and first-line regimen was a multiday MTX regimen (1mg/kg every 2 - 3 weeks). The second line is dactinomycin in cases of initial good response to MTX which then reaches the plateau levels (12), as we prescribed for her in the second line. The limitations of our case were that it was not obvious whether GTN was due to intrauterine molar pregnancy or ectopic molar pregnancy, as both of them were complete mole. Also, Further risks of GTN in ectopic molar pregnancies were not estimated. It is so important to notice that molar pregnancy can happen as ectopic pregnancy, so if we face with poor response to medical or surgical therapy in cases of EP or even in cases of intrauterine molar pregnancy, remember it is probably an ectopic molar pregnancy or heterotopic molar pregnancy, respectively.