1. Background
Laryngeal cancer accounts for approximately 25% of head and neck cancers in developed countries (1). This cancer is known as the second most common airway cancer (after lung cancer). It is most common in men in their sixth and seventh decades of life (2). Due to the lymphatic system and early symptoms such as hoarseness, laryngeal cancers are usually diagnosed early. Therefore, choosing the best treatment option to achieve the best possible oncological outcome with minimal complications is principal. Different treatments are used depending on the location, the stage of the disease, and the patient's preference. According to a general principle, more conservative organ-preserving approaches are taken in primary tumors and more invasive treatments such as total laryngectomy are considered for higher stages of the disease (3).
The early group (T1N0 and T2N0) may be treated initially by radiotherapy (RT), in selected cases, by transoral laser microsurgery (TLM), or in equipped centers, by transoral robotic surgery (TORS) (4). Although TLM has gained a special place in laryngeal oncology being an effective method in the treatment of laryngeal tumors, in many centers, RT is the initial treatment prescribed for T1 and T2 lesions, with surgery reserved for salvage after RT failure or recurrence (5, 6). The decision to choose a treatment method is complex and depends on the clinical characteristics and preferences of the patient and the physician, and standard care for early glottic cancer is still up for controversy (3, 7).
So far, several studies have been performed to evaluate the oncological results of TLM and radiotherapy in patients with early stages of laryngeal cancer. In most of these studies, the results were satisfactory for both groups and there was no significant difference in oncological outcomes.
2. Objectives
This study will demonstrate the differences in oncologic outcomes between the two main approaches for early-stage laryngeal cancer in two major referral centers in Iran and will discuss the effective variables.
3. Methods
3.1. Patients and Data Collection
All patients diagnosed with early-stage (T1-T2N0M0, AJCC staging system for head and neck cancers, Seventh Edition, 2010) laryngeal squamous cell carcinoma between 2010 and 2017 were referred to Ghaem Referral Hospital and Kasra day clinic for TLM, or Radiation Oncology Department of Imam Reza Hospital, Mashhad, Iran, were enrolled, retrospectively.
Demographic information was extracted from the records, which included age, gender, disease stage, tumor location, smoking history, occupation, occupational exposures, and comorbidities.
After the biopsy was taken with the patient intubated and under general anesthesia, if the pathology of SCC was confirmed, TMN (Tumor, Node, Metastasis) staging of the disease was determined according to the intraoperative findings and preoperative intravenous contrast CT scan of the head and neck besides chest X-ray. For T1-T2N0M0 patients, the routine of both centers was to consider one of the two methods of TLM or radiotherapy, in consonance with the overall clinical features of the patient, and preferences of both the patient and the multidisciplinary team.
3.2. Treatments
In patients who had undergone TLM, a CO2 laser with a power setting of 10 watts in super pulse mode and the continuous setting was used for the surgical excision. Depending on the moment of the surgery, the size and shape of the spot were changed, using a micromanipulator. Wherever possible, especially in T1 tumors, attempts were made to remove the tumor en-block, although in larger masses (T2) the procedure was usually performed by piecemeal resection. In glottic tumors, vestibulectomy was performed whenever the lateral or anterior margins of the tumor were hidden due to the presence of a ventricular fold. In all the surgeries, which were carried out by a larynx fellowship head and neck surgeon, attempts were made to remove the tumor with a 2 - 3 mm grossly free margin and to beware vocal cord function preservation.
If the pathological examination report indicated a “free margin”, the case was considered “complete resection” and the patient underwent follow-up. The cases reported as “affected margin” were considered “incomplete resection” and referred for adjuvant radiation therapy. The latter category was not included in the study.
In the radiation group, all patients were treated with a linear accelerator. Treatment planning was performed, using a 2D (based on bony landmarks on radiography) or 3D (based on CT scan findings and superficial landmarks) method. The field sizes ranged from 4 × 4 cm to 6 × 6 cm (for a large T2 lesion). The cervical lymph node chain was not electively treated. The conventional prescribed doses were 66 Gy for T1 and 70 Gy for T2 cancers, given in 2-Gy fractions.
Follow-up after TLM or radiotherapy was the same for all patients: Outpatient indirect laryngoscopy in the first week, the first month, then every 3 months for a year, and annually for life.
In this study, the outcomes are defined as follows (8):
(1) Complete recovery: If the patient has no evidence in favor of recurrence.
(2) Overall survival rate: Percentage of patients who survived until the last follow-up.
(3) Disease-specific mortality rate: The fraction of the patients who underwent TLM or definitive RT and died during the follow-up, as a result of laryngeal cancer.
(4) Locoregional recurrence: During the follow-up, if the patient had evidence related to recurrence in history and physical exam, indirect laryngoscopy, or neck evaluation, the patient underwent biopsy and imaging studies. If the diagnosis of recurrence was confirmed pathologically or the N stage increased, the case was considered a locoregional recurrence.
In case of recurrence after TLM, if the re-staging indicated a T1-2N0M0, the patient underwent TLM again and the follow-up continued. Otherwise, follow-up ended and one of the options of radiotherapy, partial laryngectomy (with or without radiotherapy), or total laryngectomy (with or without radiotherapy) was chosen. In case of a locoregional recurrence in the radiotherapy group, the patient underwent salvage therapy and follow-up ended.
(1) Organ (larynx) preservation rate: The fraction of the patients that did not require total laryngectomy and had a preserved larynx until the last follow-up.
3.3. Statistical Analysis
The study is a retrospective cohort, the sample consists of all the T1-T2N0M0 patients referred to Ghaem Referral Hospital and Kasra day clinic for TLM, or Radiation Oncology Department of Imam Reza Hospital, Mashhad, Iran, between 2010 and 2017.
The data were assessed by Shapiro–Wilk test, using the Statistical Package for Social Science version 22 (SPSS Inc., Chicago, Illinois). Assessments related to complete recovery, overall survival rate, disease-specific mortality rate, locoregional recurrence, and organ (larynx) preservation rate were presented by Kaplan-Meier curves and were analyzed by univariate log-rank (Bewick, Cheek, & Ball, 2004). P < 0.05 was considered significant.
4. Results
A total of 196 patients were eligible, 113 treated with TLM and 83 by RT. Of the 113 patients subjected to TLM, 17 had insufficient data (including the pathological report for margins), and 31 were lost to follow-up. In the radiotherapy group, 5 had insufficient data and 20 were lost to follow-up. In the end, 123 patients were included in the study.
4.1. Overall Subject Characteristic
In total 123 patients were examined, 65 were treated with TLM and 58 underwent RT. The mean age of patients was 59.85 in the TLM group, and 62.43 in the RT group. Pearson Chi-Square was used to compare the two groups, and the difference was not significant statistically (P = 0.581). Patient characteristics are listed in Table 1. The only feature that was significantly higher in the radiotherapy group was the prevalence of smoking. This finding was further investigated by comparison of smoking cessation rates in the two groups. In patients of TLM group, 41 patients (63.1%) quit smoking after treatment, and in the radiotherapy group, 46 patients (79.3%) quit smoking opium after treatment. The comparison of these data was statistically significant (P = 0.048).
| Variables | TLM Group (%) | Radiotherapy Group (%) | Statistical Significance |
|---|---|---|---|
| Mean age a | 59.85 | 62.43 | 0.581 |
| Gender (male) b | 89.2 | 82.8 | 0.299 |
| Diabetes a | 4.6 | 1.7 | 0.689 |
| Cardiac dis a | 20 | 25.9 | |
| Diabetes and cardiac dis a | 4.6 | 5.2 | |
| Lung dis a | 1.5 | 5.2 | |
| Immune deficiency a | 0 | 0 | |
| Other comorbidities a | 6.2 | 3.4 | |
| No comorbidities a | 63.1 | 58.6 | |
| Smoking a | 67.7 | 91.4 | 0.01 |
| Opium addiction a | 47.7 | 53.4 | 0.524 |
| Continuance of smoking after treatment a | 36.95 | 20.7 | 0.48 |
| Cigarette smoking and opium cessation after treatment a | 63.1 | 79.3 | |
| Occupational exposures a | 6.2 | 0.0 | 0.55 |
Abbreviation: TLM, transoral laser microsurgery.
a Pearson chi-square test was used.
bt test was used.
4.2. Stage and Tumor Location
Tumor location was another parameter that was compared between the two treatment groups. Among patients in the TLM group, 59 patients (90.8%) had glottic cancer and 6 patients (9.2%) had supraglottic cancer. In the radiotherapy group, 39 patients (67.2%) had glottic cancer and 19 patients (32.8%) had supraglottic cancer. The difference was statistically significant (P = 0.001).
The extent of cancer, represented by TNM, can affect the survival of a patient because more severe cases often have a worse prognosis. Among TLM patients, 43 patients (43.9%) had stage T1a glottic carcinoma, 7 patients (7.1%) had T1b glottic carcinoma, 9 patients (9.2%) had T2 glottic carcinoma, 4 patients (16.0%) had supraglottic T1, and 2 patients (8.0%) had supraglottic T2. In patients undergoing radiotherapy, 11 patients (11.2%) had glottic T1a stage, 6 patients (6.1%) had glottic T1b, 22 patients (22.4%) had glottic T2, 3 patients (12.0%) had supraglottic T1, and 16 patients (64.0%) had supraglottic T2.
When comparing the T-stage to the treatment groups, TLM and RT, through a Pearson chi-square analysis, a statistically significant relationship was observed. Therefore, it is mandatory to stratify the outcomes based on the T stage (see subgroup analysis).
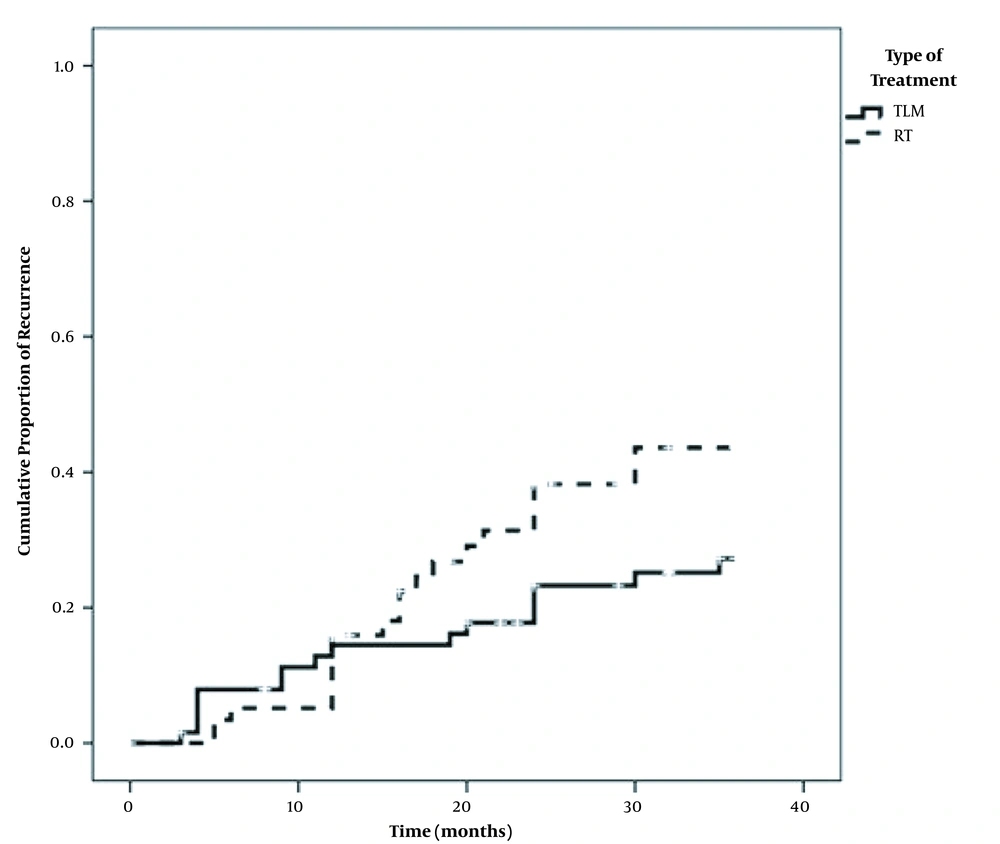
4.3. Recurrence Rate
The recurrence rate is one of the oncologic outcomes compared between the two treatment groups. Among the patients who underwent TLM, 16 patients developed laryngeal cancer recurrence during 36 months of follow-up, which accounts for 27.3% according to the analysis of the Kaplan-Meier diagram. Among patients in the radiotherapy group, 21 patients developed laryngeal cancer recurrence during 36 months of follow-up, which indicates a 43.6% probability of recurrence. The overall difference in the likelihood of recurrence between the two groups was not statistically significant (P = 0.114) (Figure 1).
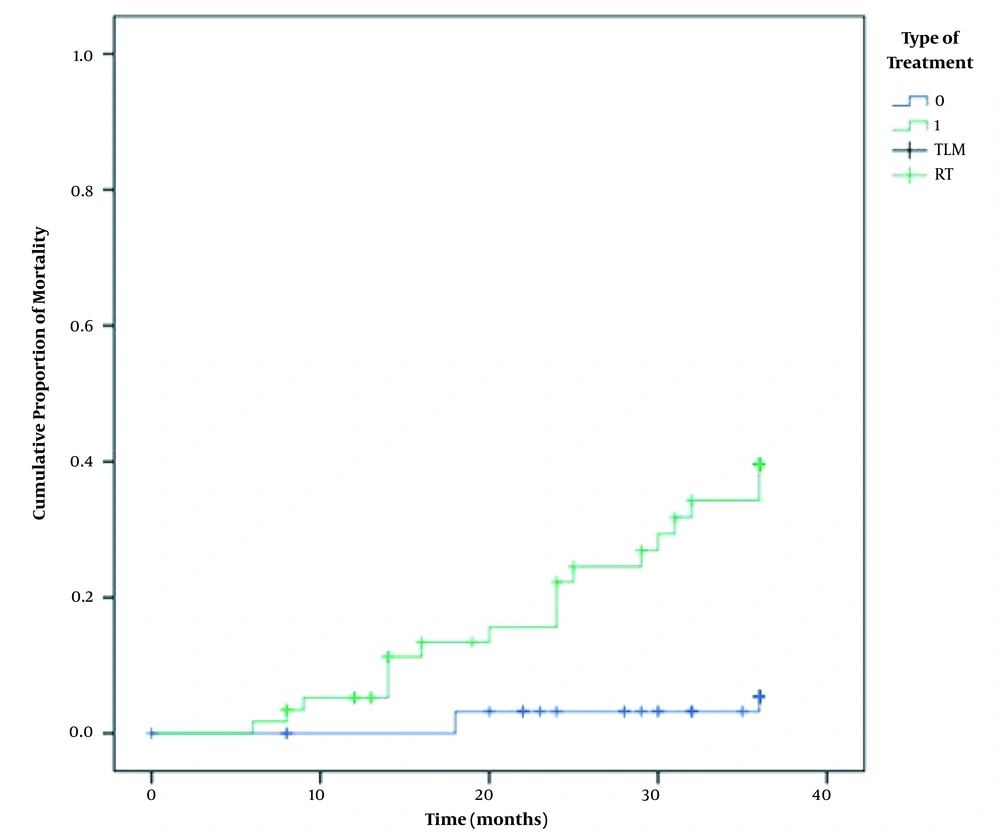
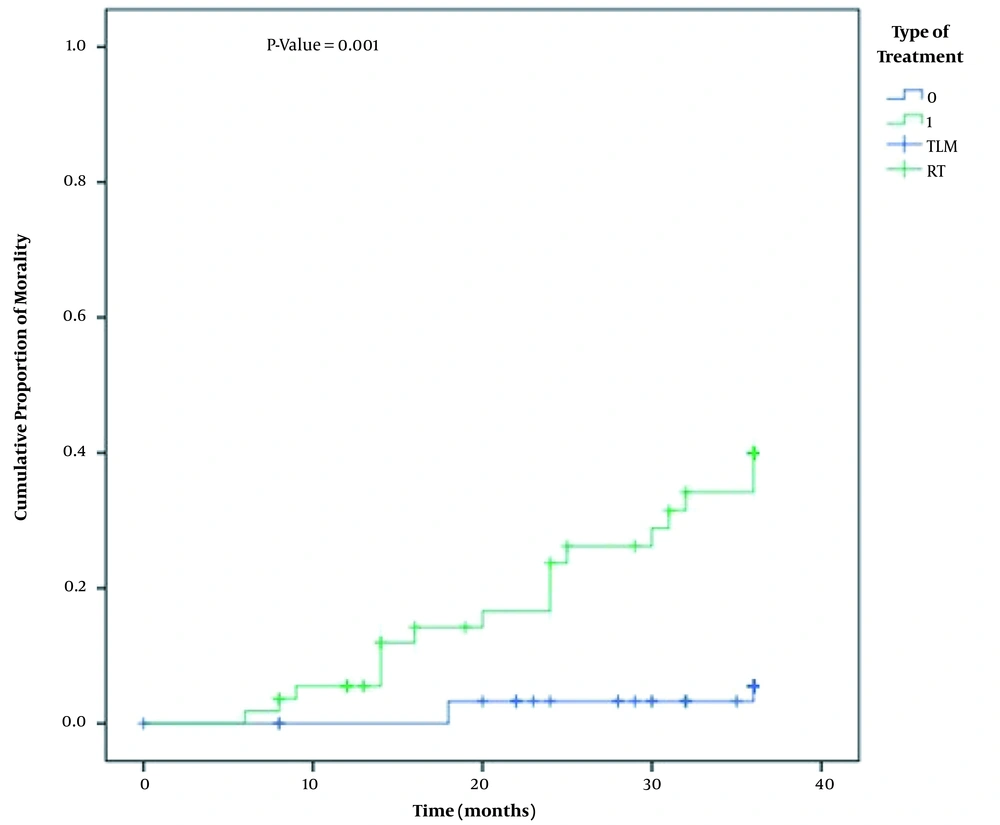
4.4. Mortality Rates and Overall Survival
During the 36-month follow-up of the laryngeal cancer patients enrolled in this study, death occurred in several patients in both groups. In the TLM group, out of 3 deaths, 2 (66.6%) were due to laryngeal cancer and 1 (33.3%) was not related to cancer. In the radiotherapy group, out of 18 patients who expired, 15 (83.3%) died due to laryngeal cancer and 3 patients (16.6%) died due to a cause other than cancer. Overall survival and overall mortality rate were evaluated and compared based on the analysis of the Kaplan-Meier diagram. The overall survival rate in the TLM group was 94.6% and the mortality rate in this category was 5.4%. The overall survival rate in the radiotherapy group was 60.4% and the mortality rate in this category was 39.6% (Figure 2). The difference in the overall mortality rate was statistically significant (P = 0.001). The disease-specific mortality rate in patients who underwent TLM was 5.5% and the disease-specific mortality rate in the radiotherapy group was 39.9%. The difference was statistically significant (P = 0.001) (Figure 3).
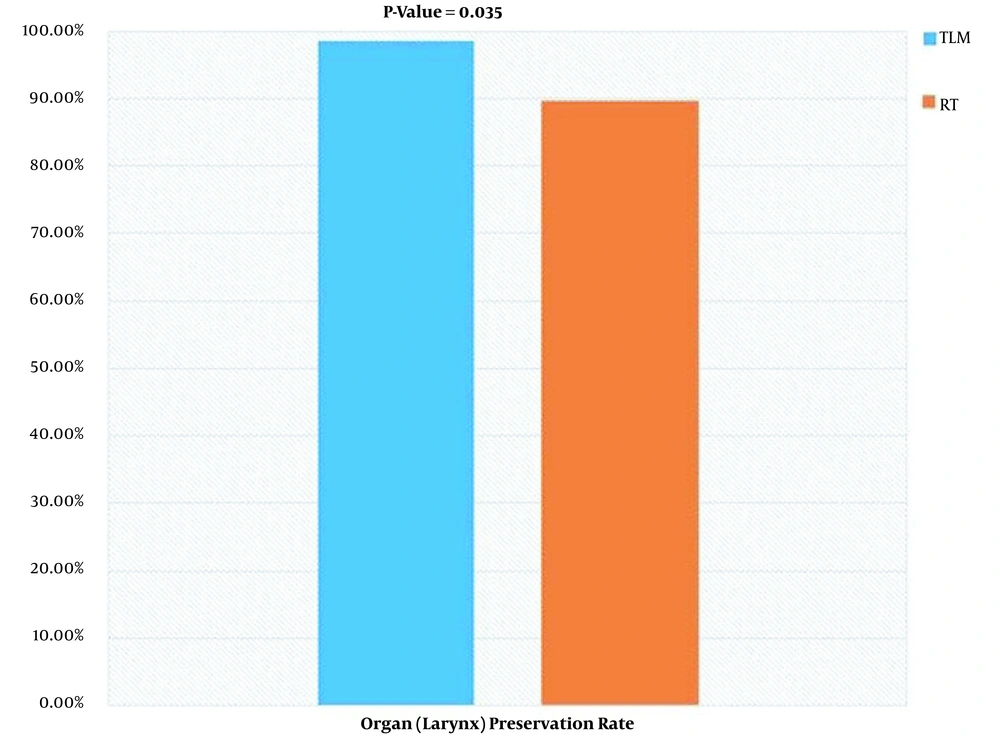
4.5. Organ (Larynx) Preservation Rate
Although both TLM and radiotherapy are treatment options to preserve the organ, occasionally, a recurrence of the disease in these patients will lead to total laryngectomy and organ loss. This outcome is also one of the main oncologic results determining the efficacy of treatment. A total of 7 patients underwent total laryngectomy in the 36-month follow-up. The larynx was preserved in 64 (98.5%) patients of the TLM group and 52 (89.7%) patients of the radiotherapy group. The superiority of TLM in terms of organ preservation was statistically significant (P = 0.035) (Figure 4).
4.6. Subgroup Analysis
According to the mentioned data related to stage and tumor location, the proportion of patients with higher stages in the radiotherapy group was higher. Therefore, it is mandatory to examine the effect of variables simultaneously on the oncological consequences of the treatment method. The COX Regression test was used for this purpose. Based on the results of this test, among the variables (type of treatment, tumor location, and stage of the disease), the only variable that significantly affected mortality was the type of treatment. The Odds Ratio of mortality in the radiotherapy group is 5.187 times that of the TLM group, in a supraglottic tumor is 1.649 times that of a glottic one, and in stage T2 of the disease 2.564 times that of the T1a patients (Table 2).
| Variables | HR | Confidence Interval 95% | P |
|---|---|---|---|
| Tumor location (suprglottic vs glottic) | 1.649 | 0.654 | 0.289 |
| Stage T1b vs T1a | 1.873 | 0.329 | 0.480 |
| Stage T2 vs T1a | 2.564 | 0.770 | 0.125 |
| Treatment (RT vs TLM) | 5.187 | 1.362 | 0.016 |
Abbreviations: TLM, transoral laser microsurgery; RT, radiotherapy.
5. Discussion
Since the introduction of Laser Endoscopic Surgery for the treatment of laryngeal cancer by Strong and Jako (9, 10), TLM has obtained a special place in laryngeal oncology and has become an effective method in the treatment of laryngeal tumors. Benefits such as magnification created by the microscope used in the TLM method reduce the resection, as the distance between normal tissue and the tumor is better recognized, and therefore the preservation of intact parts and the structures of the larynx in total, lead to a reduction in the use of permanent tracheostomy and nasogastric tube insertion (11-13). On the other hand, radiotherapy has been widely used in the treatment of early-stage laryngeal cancers and it is highly accepted among experts and clinicians as an organ preservation method (3). The major advantages of the surgical approach are avoidance of radiation and single treatment, but RT is believed to be better than surgical approaches in terms of voice quality outcomes, especially in more extended tumors (14). Adding to the intricacies of therapy selection are patient preferences, clinical characteristics, availability of the modalities across institutions, and insurance protocols (15). For instance, while surgery is more cost-effective than RT in western countries, the costs may be substantially higher than RT in the Middle East because of insurance coverage rules. As expected, current opinions of optimal therapy differ across disciplines and countries.
Though several studies have attempted to compare TLM and RT (with satisfactory results for both groups), due to a paucity of high-quality research and the lack of conclusive randomized prospective studies, standard care for early glottic cancer is still a matter of controversy (14, 15).
Mo et al. evaluated the results of TLM surgery and radiotherapy in the treatment of patients with glottal T1 cancer through systematic review and meta-analysis. They reviewed 11 studies from April 1990 to January 2012, demonstrating that the organ preservation rate in the TLM method is significantly better than radiotherapy (P < 0.00). The TLM method significantly increased overall survival (P = 0.04), but there was no significant difference in terms of local control between TLM and radiotherapy (P = 0.91). The authors concluded that utilizing TLM has better outcomes than radiotherapy (3). The organ preservation rate was significantly higher in the TLM group of our study as well. The lower disease-specific mortality rate was also a similar finding to the increased survival reported by Mo et al. (3).
In 2016, Warner et al. evaluated the oncological results of TLM and radiotherapy in the treatment of patients with stage T2 glottic laryngeal cancer in a systematic review study. After reviewing the results of 60 studies, they concluded that the 5-year local control rates in both TLM and radiotherapy methods were similar, 75.81% and 77.26%, respectively. They declared that both methods could be used as first-line treatment for glottic T2 stage cancers (16). In the present study, similar to what was observed by Warner et al., the local recurrence rate was not statistically different between the two groups.
In a retrospective cohort study in 2017, Ahmed et al. evaluated the results of radiotherapy and TLM in patients with glottal T1 cancer. There was no statistically significant difference in recurrence rate, or larynx preservation between the two groups (P = 0.77, P = 0.18, respectively). The authors concluded that the oncologic outcomes of both methods in the treatment of patients with T1 laryngeal cancer are similar and there is no preference for either method over the other (17). In our study, as in the study above, all patients were followed for the same period (for 36 months) and there was no significant difference in terms of demographic and medical characteristics between patients in the two groups. Contrary to what is found in that study, our results were significantly better in our TLM group. One of the influential factors for this result could be the higher number of more extensive tumors (T2) in patients of the radiotherapy group in both glottic and supraglottic cases in our study.
De Santis et al., compared radiation therapy and TLM for early glottic cancer patients in a retrospective cohort study. Contrary to our study, they reported that there was no difference in the 5-year disease-free survival and total laryngectomy-free survival between the RT and TLM treatment groups. Both groups showed similar 5-year survival before and after stratifying by confounding variables age and T stage, mentioning the fact that only 2 patients whose cancer was categorized as T2 were treated with TLM, making this a non-meaningful comparison (7).
More recent studies demonstrate results in favor of TLM the same as the present study; Ma et al., conducted the first multi-modality voice analysis to compare long-term voice outcomes following radiation and laser microsurgery in early glottic cancer. One hundred and two patients were analyzed, using a subjective index, a voice and speech software, and blinded speech-language pathologists. They reported that TLM results in better long-term voice outcomes than RT in objective voice analyses (contrary to the common beliefs), but not in self-perception (18).
In a systematic review and meta-analysis of T1 glottic cancer outcomes in 2019, Vaculik et al. included 16 studies, the majority being retrospective cohorts with two prospective cohort studies. The meta-analysis favored treatment with TLM for T1 glottic carcinoma patients in terms of overall survival, disease-specific survival, and laryngeal preservation. There was no difference in local control between TLM and RT in T1 glottic cancer (15). These results are the same as the findings of the present study.
Patient preference is one of the influential factors in decision-making for treatment. In a study published in 2017, treatment preferences of 175 patients with early (T1-T2) glottic carcinoma were reported after counseling. The majority of the patients preferred TLM for reasons including optimization of future options and shorter treatment (19). The weakness of the study was that the majority of the patients were counseled by an ENT surgeon.
Because of the high cure rate in early laryngeal cancers, the prognostic impact of initial treatment in salvaged recurrences is an important factor to consider. In 2018, Locatello et al. reported that the RT-failed early glottic cancers showed worse outcomes in terms of survival, complications, and locoregional recurrences compared to TLM-failed cases (20).
In 2020, a study with a similar structure to the present report in China evaluated the oncologic results in 164 patients. Similarly, they reported that both TLM and radiotherapy obtained good local control rates, but treatment with RT had a worse laryngeal preservation rate (21).
Considering that TLM has been introduced to the treatment of patients with early stages of laryngeal cancer in Mashhad since 2010, the number of eligible patients was 65, though the strength was the lack of significant differences in demographic and medical characteristics of patients.
5.1. Limitations of the Study and Suggestions for Future Works
As mentioned above, one of the influential factors for significantly better outcomes in the TLM group of the present study could be the higher number of more extensive tumors (T2) in patients of the radiotherapy group in both glottic and supraglottic cases in our study. Another potential bias to the current study results is the effects of treatment switching in patients who experienced progression on TLM and received RT, which could be addressed and minimized by increasing the sample size and utilizing other statistical methods. Smoking, as well as its continuation after diagnosis and treatment of the disease, are also independent factors affecting the survival of patients (22, 23). One of the confounding factors in the present study can be the difference in this feature between the two groups. Some previous studies have demonstrated the negative impact of supraglottic location on outcome and survival (24). As the radiotherapy group had significantly more supraglottic tumors, this is another confounding factor worth investigating in further studies. Considering the concerns about long-term side effects of radiation on adjacent organs (25), it is important to further investigate whether TLM could be the treatment of choice or not.
5.2. Conclusions
As early laryngeal cancers have high cure rates and treatment outcomes influence the patients' voice preservation and quality of life, it is mandatory to choose the perfect option. Although previous data were not conclusive in comparison between TLM and RT, more recent studies demonstrate better oncologic outcomes and larynx preservation rates with TLM. The present retrospective cohort study demonstrated that although the overall comparison of the likelihood of recurrence was not statistically different, both disease-specific mortality and larynx preservation rate were significantly better in the TLM group. As there are confounding factors influencing this conclusion, multi-institutional prospective studies are necessary to make more established conclusions.