1. Background
Pediatric cancer comprises 0.5% of all cancers worldwide and is the leading cause of death in children younger than 14 years old (1), with an incidence rate of 50 to 200 cases per one million population (2). However, recent improvements in treatment protocols have considerably increased the survival rate of children diagnosed with cancer (3).
Studies have indicated that approximately one out of every 285 children diagnosed with cancer is admitted to the pediatric intensive care unit (PICU) in the United States annually (4). Although the mortality rate of children admitted to the intensive care unit (ICU) because of childhood cancer is much higher than admitted non-cancerous children (5), over the past decades there have been significant advancements in the status of the former group (6). To be more precise, their overall survival rate increased to 80% and their mortality rate significantly decreased (7). Nevertheless, despite recent therapeutic advances in the treatment of children with cancer, the side effects of the treatment methods had led to the hospitalization of children 38% of them need to be admitted to the ICU for the first 3 years of their treatment (7, 8).
It is also reported that these children account for approximately 4.2% of all ICU hospitalizations and 11.4% of all ICU deaths (8).
The ICU ward plays a key role in improving the performance of treatment plans and increasing the life expectancy of hospitalized children. Therefore, it is considered an integral part of the treatment protocol. Despite the importance of hospitalization children with cancer in the ICU (9) only a few studies have been conducted in this field around the world, especially in developing countries such as Iran and other neighboring countries (10).
Mahak Pediatric Cancer Treatment and Research Center (MPCTRC) is a multidisciplinary referral center that plays a crucial role in the research, diagnosis, management, and care of pediatric patients with cancer younger than 14 years old. Children with malignancy from Iran and other countries are offered free support and treatment by the Mahak Hospital, a non-governmental organization (NGO).
2. Objectives
In this study, we aimed at evaluating the influence of hospitalization in the ICU on the treatment and survival of pediatric cancer in the Mahak Hospital.
3. Methods
3.1. Study Design
This retrospective study was conducted on 674 children diagnosed with cancer who were admitted to the ICU of Mahak Hospital amongst a total number of 2693 hospitalized patients from March 2014 to September 2019.
3.2. Data Collection
All data was collected from patients' clinical documents including demographic information [name, gender, date of birth, and familial history of cancer] and clinical data [type of cancer, date of diagnosis, date of hospitalization, date of treatment, date of death (if applicable), status of patients at the time of ICU discharge, adverse drug reactions (ADR) (drug allergies, grade ADR and time of ADR), secondary cancer, relapse and metastasis, treatment protocols, tracheal intubation and, extubation, number of admissions to ICU, etc.
3.3. Inclusion and Exclusion Criteria
Because of the fact that according to WHO, childhood cancer is defined when a pediatric patient younger than 14 years old is diagnosed with cancer therefore, we included all the children who were under 15 years old at the time of diagnosis with any type of cancer who admitted to the ICU from March 2014 to September 2019 were included in this study. Patients with non-cancerous diseases such as anemia and thalassemia were excluded from this study.
3.4. Survival and Prognosis
To better understanding the effect of ICU admission on patients' lives, we evaluated overall survival (OS) rates with the Kaplan-Meier method. The Total-OS (TOS) was based on the time of diagnosis to the last follow-up of the patient and the ICU-OS calculated from the time of ICU admission to the last follow-up.
3.5. Statistical Analysis
All the collected data were entered in SPSS software version 22. Descriptive analysis was done using Mann-Whitney, Spearman correlation coefficient, Kaplan-Meier Log Rank. P-value less than 0.05 was considered as statistically significant.
4. Results
4.1. Patient's Demographic and Clinical Characteristics
Totally, 674 children diagnosed with cancer were admitted to the ICU amongst a total number of 2693 hospitalized patients from March 2014 to September 2019. Among which 48.96% (n = 330) were female and 51.03% (n = 344) were male, (male to female ratio was 1/1.04). Patients' mean age was 2.54 ± 0.93 years, ranging from 5 days to 14 years. The majority of children were in the 1 to 4 years-old age group (43.62%, n = 293), and children younger than one-year-old were the fewest ones (11.12%, n = 75). The mean age of patients in their first ICU admission was 2.8 ± 0.97 years, ranging from 5 months to 19 years old. More information about patients' demographic characteristics are shown in Table 1.
| Female | Male | Total | |
|---|---|---|---|
| Age group at the time of diagnosis | |||
| < 1 | 43 (13.03) | 32 (9.30) | 75 (11.12) |
| 1 - 4 | 138 (41.81) | 156 (45.34) | 294 (43.62) |
| 5 - 9 | 84 (25.45) | 89 (25.87) | 173 (25.66) |
| 10 - 14 | 65 (19.69) | 67 (19.47) | 132 (19.58) |
| Mean age (y) at the time of diagnosis | 2.52 ± 0.91 | 2.56 ± 0.94 | 2.54 ± 0.93 |
| Age group at the time of ICU admission | |||
| < 1 | 17 (5.15) | 13 (3.77) | 30 (4.45) |
| 1 - 4 | 138 (41.81) | 134 (38.95) | 272 (40.5) |
| 5 - 9 | 90 (27.27) | 99 (28.77) | 189 (28.04) |
| 10 - 14 | 72 (21.81) | 82 (23.83) | 154 (22.84) |
| > 15 | 13 (3.93) | 16 (4.65) | 29 (4.30) |
| Mean age (y) at the time of ICU admission | 2.77 ± 0.97 | 2.86 ± 0.97 | 2.8 ± 0.97 |
| Type of diagnosis - solid tumors | 248 (36.79) | 264 (39.16) | 512 (75.96) |
| CNC tumors | 112 (45.16) | 112 (42.42) | 224 (33.23) |
| Neuroblastoma | 30 (12.09) | 63 (23.86) | 93 (13.79) |
| Sarcoma | 46 (18.54) | 40 (15.15) | 86 (12.75) |
| Renal tumors | 31 (12.50) | 23 (8.71) | 54 (8.011) |
| Retinoblastoma | 10 (4.03) | 9 (3.40) | 19 (2.81) |
| Hepatic tumors | 11 (4.43) | 7 (2.65) | 18 (2.67) |
| Germ cell tumor | 5 (2.16) | 8 (3.03) | 13 (1.92) |
| Langerhans cell histiocytosis | 3 (1.20) | 2 (0.75) | 5 (0.74) |
| Type of diagnosis - non-solid tumors | 75 (11.2) | 87 (12.90) | 162 (24) |
| Leukemia | 58 (77.33) | 70 (80.45) | 128 (18.99) |
| Lymphoma | 17 (22.66) | 17 (19.54) | 34 (5.44) |
| Status of patient at the time of ICU discharge | |||
| Alive | 203 (30.12) | 200 (29.67) | 403 (59.79) |
| Dead | 127 (18.84) | 144 (21.36) | 271 (40.20) |
| Status of patient at the time of last follow-up | |||
| Alive | 161 (48.78) | 150 (43.60) | 311 (46.14) |
| Dead | 169 (51.21) | 194 (56.39) | 363 (54.74) |
| Number of ICU admission | |||
| Once | 231 (70.0) | 250 (72.67) | 481 (71.36) |
| Twice | 56 (16.96) | 71 (20.63) | 127 (18.84) |
| More than three times | 43 (3.03) | 23 (6.68) | 66 (9.79) |
Demographic and Clinical Characteristics of Pediatrics Admitted to the ICU Based on Sex of Patient (N = 674) a
The commonest malignancies amongst children were central nervous system tumors (33.23%, n = 224) and leukemia (18.99%, n = 128). Additionally, Langerhans cell histiocytosis (0.74%, n = 5) and germ cell tumors (1.92%, n = 13) were the least frequent type of cancer among the children . Information about other types of cancer are shown in Table 1.
Duration of hospitalization to the ICU ranged from one day to 45 days, with a mean time of 7.24 ± .044 days.
4.2. Patient's Status, Follow-up, and Survival
At the time of patients' last follow-up (September 2019), 76 (11.30%) children were off-treatment because of disease progression, 235 (34.90%) were during their treatment procedure and unfortunately, 363 (53.90%) patients died.
Regarding events in their treatment procedure from the time of disease diagnosis to the last follow-up, 20.62% (n = 139) and 5.34% (n = 36) of patients experienced disease relapse and cancer metastasis, respectively, and 5 patients were diagnosed with secondary cancer. Of these events, 36 (5.34%) cases of relapses, 8 (1.18%) cases of metastasis, and one case of secondary cancer caused ICU admission in patients. More information about events based on each gender are shown in Table 2.
| Female | Male | Total | |
|---|---|---|---|
| Events up to the last follow-up | |||
| Relapse | 77 (11.42) | 62 (9.20) | 139 (20.62) |
| Metastasis | 19 (2.82) | 17 (2.52) | 36 (5.34) |
| Secondary cancer | 3 (0.45) | 2 (0.30) | 5 (0.74) |
| Events causing ICU admission | |||
| Relapse | 18 (2.67) | 18 (2.67) | 36 (5.34) |
| Metastasis | 5 (0.47) | 3 (0.45) | 8 (1.18) |
| Secondary cancer | 1 (0.15) | 0 | 1 (0.15) |
Information About Disease Relapse, Metastasis, and Secondary Cancer Events Based on Sex of Patient (N = 674) a
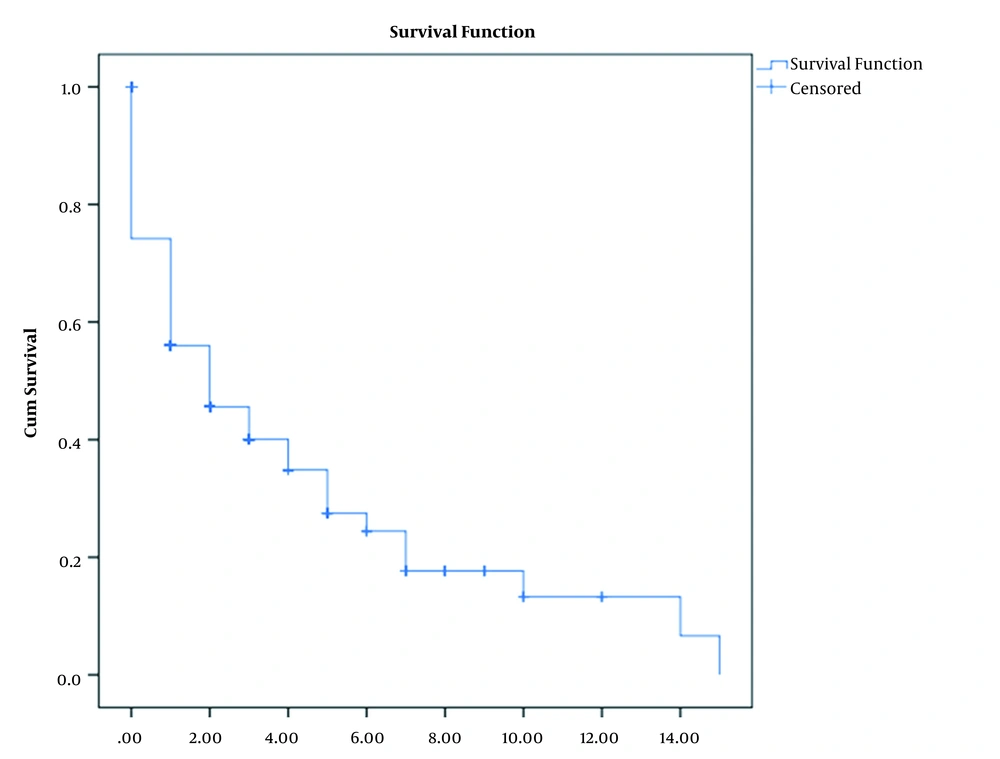
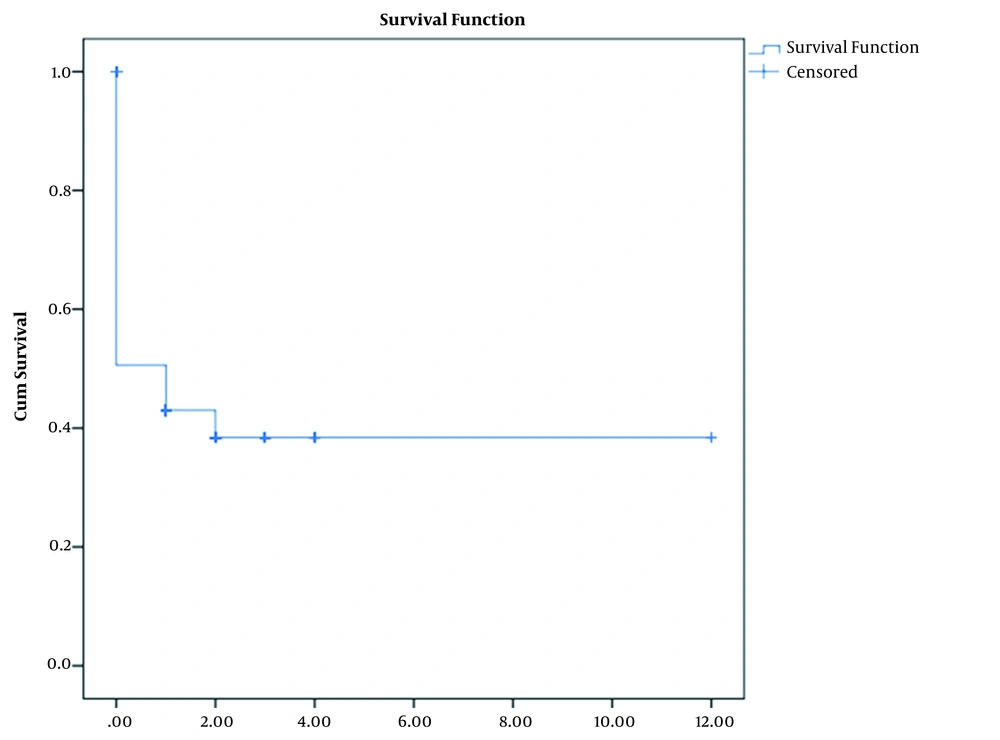
Amongst 363 dead patients, 271 (40.20%) patients expired at the ICU ward. The 3-year and 5-year overall survival (from the time of their cancer diagnosis) were 40.4 ± 2.4 and 29.50 ± 2.6, respectively (Figure 1). Besides, their 3-year and 5-year overall survival (from the time of the first admission to the ICU) was 29.6 ± 2.9. More information about patients' overall survival are shown in Table 3 and Figure 2.
| Variables | Overall Survival (OS) | ||
|---|---|---|---|
| 1-year | 3-year | 5-year | |
| TOS (from the time of diagnosis to the last follow-up) | 70.9 ± 1.8 | 40.4 ± 2.4 | 29.5 ± 2.6 |
| OS-1 based on type of cancer | |||
| Solid tumors | 78.0 ± 3.4 | 42.6 ± 5.1 | 27.1 ± 5.5 |
| Non-solid tumors | 75.5 ± 2.0 | 44.0 ± 2.7 | 32.6 ± 3.1 |
| OS-1 based on sex of patient | |||
| Female | 70.1 ± 2.7 | 39.2 ± 3.5 | 29.7 ± 3.7 |
| Male | 71.6 ± 2.5 | 41.5 ± 3.2 | 29.5 ± 3.6 |
| OS-1 based on the number of ICU admission | |||
| Once | 75.1 ± 2.1 | 44.4 ± 2.9 | 33.0 ± 3.4 |
| Twice | 61.64.4 | 38.3 ± 4.9 | 27.7 ± 5.1 |
| More than three times | 64.3 ± 6.1 | 21.5 ± 5.6 | 13.9 ± 5.1 |
| ICU-OS (from the time of ICU admission to the last follow-up) | 41.3 ± 2.2 | 29.6 ± 2.9 | 29.6 ± 2.9 |
| OS-2 based on type of cancer | |||
| Solid tumors | 42.7 ± 4.9 | 28.3 ± 6.9 | 28.3 ± 6.9 |
| Non-solid tumors | 43.9 ± 2.6 | 32.4 ± 3.5 | 32.4 ± 3.5 |
| OS-2 based on sex of patient | |||
| Female | 40.3 ± 3.0 | 31.2 ± 3.4 | 31.2 ± 3.4 |
| Male | 42.5 ± 3.3 | 28.7 ± 4.4 | 28.7 ± 4.4 |
| OS-2 based on the number of ICU admission | |||
| Once | 48.6 ± 2.6 | 41.2 ± 3.8 | 41.2 ± 3.8 |
| Twice | 32.7 ± 4.5 | 26.2 ± 4.8 | 26.2 ± 4.8 |
| More than three times | 35.0 ± 6.2 | 6.6 ± 4.2 | 6.6 ± 4.2 |
Information About Patients' Survival and Outcome (N = 674) a
Among 674 patients admitted to the ICU, 285 (44.0%) patients were intubated, of whom 120 (17.83%) and 66 (9.81%) patients were diagnosed with CNS tumors and leukemia, respectively. Also, intubation was more frequent amongst male patients (52.63%, n = 150) than female ones (47.37%, n = 135).
In this study, 481 patients were admitted once and 127 patients were admitted twice to the ICU during their treatment procedure. Also, a total number of 66 patients were hospitalized at the ICU for more than 3 times. The maximum duration of hospitalization in the ICU was 45 days and the minimum duration of hospitalization was one day. The mean time of stay in ICU was (7.24 ± .044) days.
5. Discussion
The purpose of this study was to provide a complete report on the status of children admitted to the intensive care unit (ICU) at the Mahak Hospital. Due to the lack of research on the impact of ICU admission on children with cancer survival and outcome, especially in low- income countries such as Iran, this retrospective study could play an important role in evaluating these patients' quality of life.
Although patients were administrated to the ICU with different types of cancer, there was no significant relationship between the type of cancer and the number of ICU hospitalizations or duration of it.
In Iran, several studies have been conducted on palliative care of children with cancer who were admitted to the ICU. In addition, studies on the types of infections during the period of hospitalization in ICU have been conducted (11), but to the best of our knowledge, no similar study has been conducted on children with cancer admitted to the intensive care unit.
Leukemia seems to be the most common cancer amongst pediatric patients, accounting for approximately 25% of all childhood cancers (11) followed by CNS tumors which form 17% of it (11) which were also, the most frequent type of cancer amongst patients of the present study. However, the frequency of CNS tumors was higher than leukemia, because children with CNS tumors needed more admitted to the ICU than other cancers.
According to the world health organization (WHO), Leukemia and CNS tumors are also more frequent among children in the 1 to 4-years-old age group (12), which is similar to our findings. Since Leukemia and CNS tumors are the most common type of cancers, the frequency of children in this age group is consequently higher than other age groups.
The mortality rate in the oncology ICU is higher than other ICU ranges (7).
The mortality rate in our study was 40.20% which is lower in the range of mortality from other studies (7, 13). The reason why the death rate in our study is lower than a study conducted in another low-income country (Pakistan) is that in our center, in contrast to that study, there are pediatric hematologist-oncologists who use the latest treatment protocols to cure children in the ICU (10). Nevertheless, the mortality rate in some reports from high- income countries is lower than the findings of this study due to the advances in the treatment procedures, ICU infection control, and other improvements in curing children diagnosed with cancer (1, 7, 14, 15)
The aim of our study was to evaluate the survival rate of children with cancer who were admitted to the ICU. Unfortunately, the overall survival of children in our study was lower (29.5% ± 2.6) compared to those conducted in developed countries (1, 16).
There are various reasons for the reduced survival rate, of which the most important one could be postponed referral of children to the Mahak Hospital, so most of them were in the late stages of their disease and efforts to survive them could not be effective enough. Recent studies in high-income countries have shown overall survival rates of up to 80% in pediatric cancer patients admitted to the ICU (17). Also, the overall survival rate for solid tumors (27.1% ± 5.5) was less than non-solid tumors (32.6% ± 3.1), which is similar to other studies and could be because of the fact that non-solid tumors have a better prognosis than solid ones (1, 18).
5.1. Conclusions
Despite the utilization of appropriate treatment protocols in order to cure children, the overall survival rate of children in this report was lower compared to other studies. The main reasons for that were the death of children during treatment and their late referral in the last stages of cancer. Considering that oncology ICU plays a more vital role in pediatric patients due to their disease condition, the overall survival in this type of ICU is usually lower than others, with higher rates of mortality. Finally, we suggest that a similar but multicenter study be conducted in order to assess survival and outcome of ICU admission amongst pediatric patients which could be more reliable.