1. Background
Sarcomas as the malignancies of the soft tissue are responsible for 1% of the head and neck malignancies (1, 2). Parotid gland tumors consist of a majority of 3/4 of all salivary gland tumors, while the less frequently affected sites are the submandibular, sublingual, and ancillary glands (3, 4). However, 80% of parotid gland tumors are benign; the malignant cases are crucial and life-threatening (5). For this matter, epidemiological studies in each geographical region are necessary to determine the course and management strategies for the physicians and improvement in patients’ final prognosis (6). Disease-free survival in other studies of malignant sarcoma cases in salivary glands, especially at 10 and 15 years is nearly 50% (7). This rate has improved since 1977, but still, some concerns are seen about the mortality rate in patients (8).
Surgery after precise imaging modalities is the mainstay of treatment for salivary gland sarcomas; but, the presence of adjacent vessels and nerves are important issues that should be cautioned at operation time (9, 10). Also, complementary methods should be considered in high-grade malignancies. Long-term follow-up is essential due to the high occurrence rate of distant metastases, notably to the lungs, which complicates the disease course and increases the rate of mortality (11, 12).
2. Objectives
Regarding the importance of this issue, the epidemiological characteristics of cases with salivary sarcoma among Iranian patients were assessed in this study.
3. Methods
3.1. Patients and Data Collection
This study is an epidemiological retrospective analysis that utilized data from the Iran National Cancer Registry (INCR) dataset. The dataset was used to extract information on cancer patients, who were diagnosed with a salivary glands sarcoma morphology between 2009 and 2014. The INCR dataset is a comprehensive source of information that includes data from death certificates, pathological reports, hospital reports, clinical reports, and follow-up visits across all provinces in Iran and was compiled under the supervision of the Iranian National Ministry of Health (13-15).
The information that was provided comprised the patients' given name, surname, age, sex, date of birth, diagnostic method, province of domicile, and year of diagnosis, along with the primary location, and pathologic morphology. In case additional data on clinical or pathological diagnostic reports were available, they were considered; otherwise, Death Certificate only (DCO) was accepted as the main source.
It is important to acknowledge that the individuals incorporated in the study were those who satisfied the morphological standards for salivary gland sarcoma as per the classifications suggested by the International Agency for Research on Cancer (IARC-2013) (16).
This study was performed following the approval of Ethics Committee of Shahid Beheshti University of Medical Sciences with the approval code of IR.SBMU.CRC.REC.1398.010.
3.2. Quality Control and Data Validation
The assessment and qualification of the reliability and accuracy of the data were previously conducted in our center and reported in multiple publications (13, 14).
A quality control assessment was conducted by aligning the tumor with variables such as year of birth, gender, the salivary gland of origin, tumor pathologic findings with morphology, and age with date or province of diagnosis. The assessment of duplicated cases was conducted, utilizing patients' age, first name, family name, gender, and national identification number. After removing duplicate cases, 70 consecutive cases with salivary sarcoma in Iran, from 2009 to 2014, were presented, including both parotid (n = 53) and major salivary glands (n = 17). The major salivary glands included the submandibular gland, and sublingual gland, which due to infrequent incidences were reported collectively. We included data from 22 provinces including Tehran, Isfahan, East Azarbaijan, Fars, Kermanshah, Khuzestan, West Azarbaijan, Kerman, Mazandaran, Ilam, Alborz, Gilan, Markazi, Hormozgan, Hamedan, Chaharmahal and Bakhtiari, Razavi Khorasan, Semnan, South Khorasan, Yazd, Golestan, and Sistan and Baluchestan. Due to the rare occurrence of salivary sarcomas in general and to facilitate comprehension of our data, we classified patients into 3 primary age subcategories: 0 - 14 years (children and adolescents), 15 - 64 years (working adults), and >65 years (older adults); this particular age bracket has been employed in numerous resources as a means of reporting low incidence rates. The crude incidence of each sarcoma subtype including the gender, age category, year, and province of diagnosis has been presented in Table 1.
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parotid | ||||||||||||||
| Tehran | 3 | 1 | 2 | 3 | 3 | 2 | 14 | |||||||
| Fars | 0 | 0 | 1 | 3 | 1 | 0 | 5 | |||||||
| Isfahan | 1 | 2 | 0 | 2 | 0 | 0 | 5 | |||||||
| East Azarbaijan | 2 | 0 | 2 | 1 | 0 | 0 | 5 | |||||||
| Kermanshah | 1 | 0 | 1 | 0 | 1 | 1 | 4 | |||||||
| Alborz | 0 | 1 | 1 | 0 | 0 | 0 | 2 | |||||||
| Gilan | 0 | 0 | 0 | 1 | 1 | 0 | 2 | |||||||
| Khuzestan | 0 | 0 | 1 | 0 | 1 | 0 | 2 | |||||||
| Markazi | 1 | 0 | 1 | 0 | 0 | 0 | 2 | |||||||
| West Azarbaijan | 0 | 2 | 0 | 0 | 0 | 0 | 2 | |||||||
| Kerman | 0 | 0 | 0 | 1 | 0 | 0 | 1 | |||||||
| Ilam | 0 | 0 | 1 | 0 | 0 | 0 | 1 | |||||||
| Hamedan | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |||||||
| Chaharmahal and Bakhtiari | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |||||||
| Razavi Khorasan | 1 | 0 | 0 | 0 | 0 | 0 | 1 | |||||||
| Semnan | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |||||||
| South Khorasan | 0 | 0 | 0 | 1 | 0 | 0 | 1 | |||||||
| Yazd | 1 | 0 | 0 | 0 | 0 | 0 | 1 | |||||||
| Golestan | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |||||||
| Sistan and Baluchestan | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |||||||
| Total | 10 | 6 | 10 | 12 | 10 | 5 | 53 | |||||||
| Other Salivary Glands | ||||||||||||||
| Tehran | 2 | 0 | 0 | 2 | 0 | 0 | 4 | |||||||
| Isfahan | 0 | 1 | 0 | 2 | 0 | 1 | 4 | |||||||
| East Azarbaijan | 0 | 0 | 0 | 1 | 0 | 1 | 2 | |||||||
| Mazandaran | 0 | 0 | 1 | 0 | 0 | 1 | 2 | |||||||
| Khuzestan | 1 | 0 | 0 | 0 | 0 | 0 | 1 | |||||||
| West Azarbaijan | 0 | 1 | 0 | 0 | 0 | 0 | 1 | |||||||
| Kerman | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |||||||
| Ilam | 0 | 0 | 1 | 0 | 0 | 0 | 1 | |||||||
| Hormozgan | 0 | 0 | 1 | 0 | 0 | 0 | 1 | |||||||
| Total | 3 | 2 | 3 | 5 | 1 | 3 | 17 | |||||||
Total Data for Year and Residence Provinces of All Tumors
3.3. Statistical Analysis
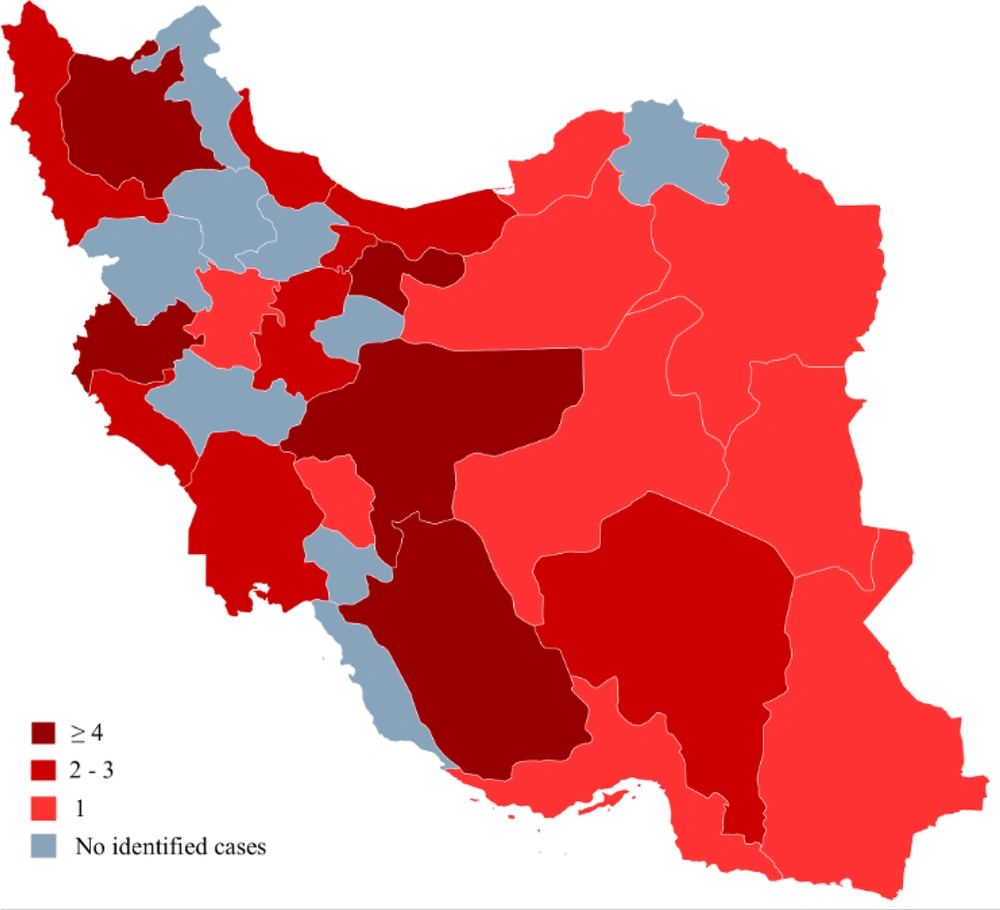
The software utilized for conducting data analysis and data visualization was Excel version 2016. We generated a provincial incidence heat map to provide a better grasp of regional incidences (Figure 1). The study did not conduct a comparative evaluation. Only epidemiological data are presented. To enhance presentation, categorical variables are utilized to represent numerical data, such as age. We calculated a cumulative age-adjusted incidence rate (CAIR) for salivary gland sarcomas over 6 years, utilizing data from the population census conducted by the Statistical Centre of Iran during the mid-point of the study duration (2011).
4. Results
4.1. Parotid
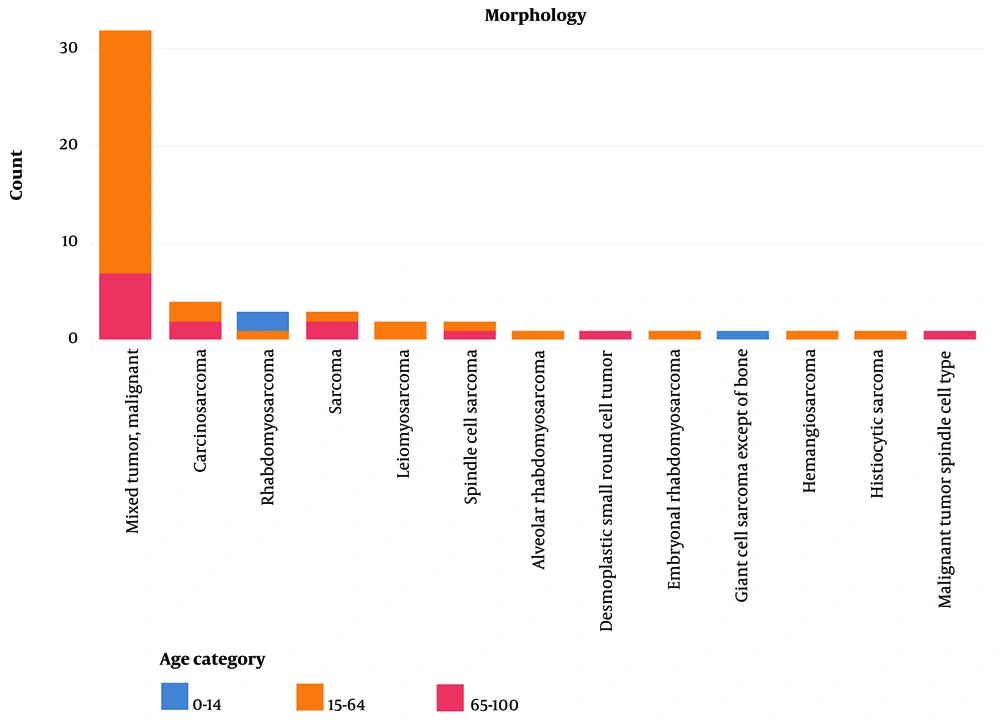
A total of 53 parotid sarcoma cases were reported from 2009 to 2014. The predominant pathological subtype was malignant mixed tumor, accounting for over 60% of cases (Figure 2), while carcinosarcoma and rhabdomyosarcoma were less frequently observed. The age range of 15 to 64 years accounted for 67% of sarcomas with this particular origin. The ratio of females to males was 0.76. The yearly occurrence rate exhibited a decreasing trend, except in the years 2011 and 2012. As shown in Table 1 , 12 cases were from Tehran.
4.2. Other Major Salivary Glands
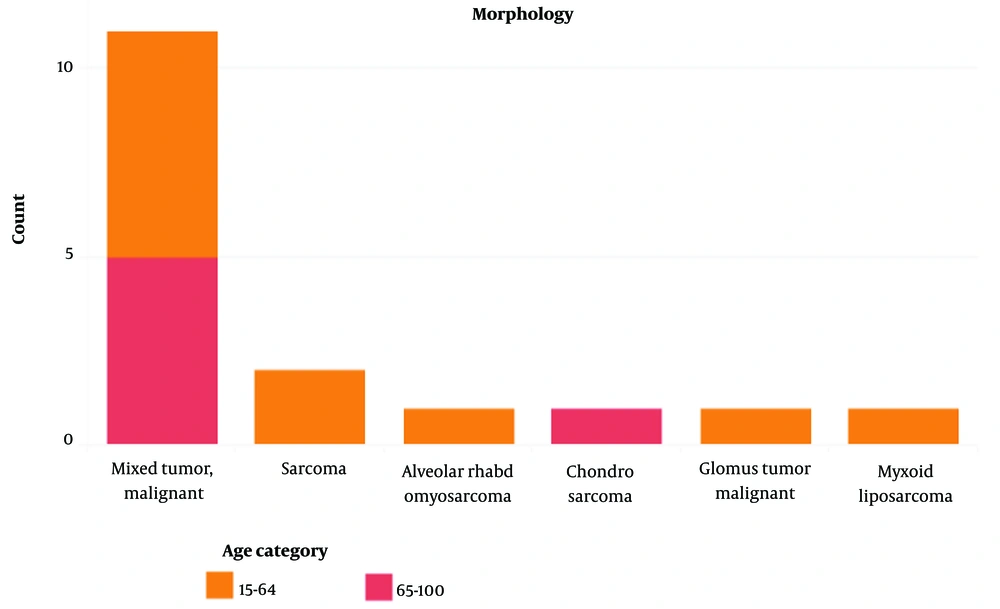
A total of 17 cases of other salivary gland (such as sarcomas) were reported. The highest incidence rate was reported in 2012 but no significant pattern was observed in the other years. Malignant mixed tumor was the most common subtype encompassing 64% of all cases (Figure 3). In the same way as parotid sarcomas, the majority of cases were in the age range of 15 to 64 years. The female-to-male ratio was 0.7. As shown in Table 1 , 4 cases were from Tehran. Table 2 illustrates the CAIR per 1 million individuals across various age groups for both the parotid gland and other salivary glands.
| 0 - 14 Years | 15 - 64 Years | 65 - 100 Years | CAIR (0 - 14 Years) | CAIR (14 - 64 Years ) | CAIR (>64 Years) | |
|---|---|---|---|---|---|---|
| Parotid | 3 | 36 | 14 | 0.016004854 | 0.05796 | 0.339074 |
| Other salivary glands | 0 | 11 | 6 | 0 | 0.01771 | 0.145317 |
| Total | 3 | 47 | 20 | 0.016004854 | 0.07567 | 0.484391 |
Cumulative 2009 – 2011 Age-Adjusted Incidence Rates (CAIR) Per 1 Million People, Based on Mid-duration (2011) Population
5. Discussion
Salivary gland sarcomas of primary origin are infrequent, with a prevalence ranging from 0.3% to 1.5% of salivary gland tumors. These sarcomas account for 1.5 to 2.3% of malignant salivary neoplasms (17, 18). The majority of occurrences are observed in the parotid gland, although a significant proportion of instances are evident in the other major salivary glands, specifically the submandibular glands (18, 19). The findings of this investigation indicate that malignant mixed tumors were the prevailing form of malignancies affecting the salivary glands overall. Salivary sarcomas, whether located in the parotid gland or other salivary glands exhibited a higher incidence rate among the male population. However, the study did not find any significant gender predominance. The age range of the majority of our reported cases was between 15 and 64 years; although, our age-adjusted incidence rate suggests a greater prevalence of salivary gland tumors in the elderly population (aged 64 years and above), which can be attributed to their relatively smaller demographic representation and generally higher incidence of malignancies with advancing age, a recurring trend commonly observed in the majority of malignant tumors. Moreover, no discernible geographical pattern was observed. The incidence of primary leiomyosarcoma malignancies in the head and neck region is infrequent, accounting for less than 10% of all leiomyosarcomas. Typically, this type of malignancy is observed in individuals of middle age (20, 21). A slight male predominance was seen, but there was no significant sex difference across the tumors.
The prognosis could be predicted by the grade, size, and site of the salivary tumors as well as the surgery success rate, nevertheles, the prognosis is usually poor for major salivary glands (22, 23).
Based on the morphological aspects in the histopathological evaluation of salivary tumors, the poorly differentiated adenocarcinoma, myoepithelioma, leiomyosarcoma, rhabdomyosarcoma, fibrosarcoma, hemangiosarcoma, histiocytic sarcoma, and undifferentiated sarcoma are considered for the differential diagnosis (24). In our study, the majority of cases in both parotid and non-parotid tumors were seen as malignant mixed types. With advancements in molecular techniques providing more powerful tools, now it is possible to recognize detailed signs of differentiation toward some specific lineages in salivary tumors and classify a large number of the tumors more properly.
The study by Al Sarraj et al. conducted in the United Arab Emirates showed that among 83 malignant salivary gland tumors, higher frequency was observed in males compared to females, which was also concordant with our findings (25). Also, the peak occurrence in their study was in the fifth decade of life. Moreover, in our study, the rate was rising with age. In their study, Mucoepidermoid carcinoma was the most common type of tumor (35%) following adenoid cystic carcinoma (18.1%) and acinar cell carcinoma (10.8%). They declaimed similar pattern of tumor distribution was seen in patients from Middle Eastern countries. Another study by Noel et al. in the Caribbean region among 85 cases showed that malignant neoplasms made up the minority with only 7 cases whereby mucoepidermoid carcinoma was the most common malignant neoplasm found followed by squamous cell carcinoma (26).
Lack of association between gender and subtype of salivary tumors was noticed in previous studies, whereas the slight male predominance in our study was observed. According to this result, it can be postulated that this finding would be attributable to the higher rate of hubble-bubble use among Iranian subjects. Other undetermined factors should also be assessed by further studies to investigate the etiologies of this concept. The previously mentioned hubble-bubble use may also be responsible for the predominance of age range of 15 to 64 years in our study.
Totally, according to the obtained results in this study, it may be concluded that salivary sarcoma in the Iranian population is mostly mixed malignant tumor subtype and identical patterns were observed in both parotid and other major salivary glands of the same age and sex category. In addition, slight male predominance was perceived. Nonetheless, further studies with longitudinal follow-up are required to achieve more definite results, particularly about the prognosis and outcomes in patients with salivary sarcoma and its contributing factors.
5.1. Limitations
The main limitation of this study was the comparatively infrequent occurrence of salivary gland sarcomas, which complicated the process of reporting and evaluating such diagnoses. Despite our diligent efforts to procure data from a nationwide database and our success in acquiring information from 22 provinces, certain cases may have been overlooked as a result of incomplete data registration in cities with limited pathology confirmation resources. The authors acknowledge the importance of enhancing the quality of INCR data and have explored various approaches that are expected to yield improvements in data quality in the coming years.