1. Background
In the present century, non-communicable diseases are the main leading cause of death in most countries, among them, cancer is a main cause of death and the most important obstacle to increasing life expectancy worldwide. According to the World Health Organization (WHO) estimation, in more than half of the world, cancer is the first or the second cause of death in people aged younger than 70 years (1). The epidemiological pattern of cancer in developing countries is increasing (2).
Depending on the climatic conditions in different geographical regions, different diseases are spread in that area. Skin cancer is one of the most common cancers in different regions (3). According to previous studies, one out of every five people has a chance of developing one type of skin cancer (4). It is more common in developed countries such as Australia, New Zealand, and the United States. But the mortality of this disease is higher in developing countries (5, 6). Most skin cancers are the result of modern human migration and the mismatch between skin pigmentation and geography or lifestyle (7-9). Although the trend of cancer rate is declining, different types of skin cancer have an increasing growth (10, 11).
In Iran, a developing country with diverse climates and different ethnic groups (12), cancer is the third cause of mortality (13). The lifestyle of the people in the country depends on some factors such as living area and ethnic group. These lead to differing cancer incidence rates in various areas (14, 15).
Skin cancer has been increasing in Iran (5). According to the national report of the cancer registry of Iran, non-melanoma skin cancer has been the third most common cancer in the country based on age-standardized rates. This cancer was the second most common cancer among men and the third most common cancer among women (16).
The relative risk of skin cancer varies in different climates and depends on geographical regions (17, 18). The difference in the incidence of this disease is due to the geographical features of the regions which influence the type of clothing, nutrition, and activities of the people (19, 20). The increased incidence of skin cancer may be influenced by a combination of various factors including aging, long-term outdoor activities, genetics, and exposure to ultraviolet radiation due to prolonged exposure to sunlight (21-24).
Some studies have been conducted on the association of skin cancer incidence with latitude (25-27). Rivas et al. evaluated the relationship between skin cancer and latitude in different regions of Chile. The results of this study showed that the incidence of skin cancer was significantly related to latitude (28).
The study conducted by van der Leun et al.’s showed that non-melanoma skin cancer is positively related to the average daily maximum temperature and ultraviolet radiation. They suggested assessing the temperature effect on skin cancer in various regions (29). Ultraviolet radiation is affected by temperature, rainfall, and other climatic factors (30).
Iran is a relatively large country with an area of 1,648,195 km2 located in the southwest of Asia. According to the 2016 census, Iran's population is 79926270. It is the 17th in terms of area and the 18th in population in the world (19). It is located between 25° to 40° N latitudes and 44° to 63.5° E longitudes. The two main Zagros and Alborz mountains with altitudes up to 5610 (m) divide the country into different climates. It runs north to the Caspian Sea and south to the Oman Sea and the Persian Gulf (31). Climate condition varies in Iran. Central and sub-eastern regions of Iran from arid regions and some of the western parts of the country experience semi-arid climates (32). Therefore, there is a high-climatic diversity in Iran.
Based on our knowledge, there is no comprehensive study on the effect of climatic and geographic parameters such as temperature, wind, humidity, latitude, and altitude on the incidence of skin cancer using mixed model effect models.
2. Objectives
The aim of this study was to investigate the impact of latitude, altitude, wind speed, humidity, and maximum air temperature on age-standardized incidence rates (ASR) of skin cancer in different provinces of Iran.
3. Methods
The present study is ecological. In order to assess the effects of the meteorological parameters and geographical factors on skin cancer incidence in Iran, we used panel data from all provinces as subjects over a six-year period of time. In this study, the average of the maximum air temperature, relative humidity, and wind speed of all provinces were calculated by the Islamic Republic of Iran Meteorological Organization (IRIMO) for a 29-year period. The ASR of skin cancer for all provinces was obtained from reports of the national cancer registry of the Iranian Ministry of Health and Medical Education. Based on these reports, ASR of skin cancer was available from 2004 to 2008 and 2015.
The incidence of skin cancer is affected by many factors. In the present study, for each province, the averages of meteorological parameters for 29 years were considered as covariates. In addition, gender and geographical parameters of latitude and altitude were used as other covariates. The annual ASR of skin cancer was the response variable. In this study basal cell carcinoma, squamous cell carcinoma, malignant melanoma, and basosquamous carcinoma were considered skin cancer.
To evaluate the impact of meteorological and environmental factors on the incidence of skin cancer, the mixed effects polynomial regression model was applied to the data. Also, different structures of the covariance matrix of error were evaluated for the applied model. The best structure of the covariance matrix was chosen based on the lowest Bayesian information criteria (BIC). Data analysis was performed in the environment of R freely software version 3.5.2 using the “nlme” package.
4. Results
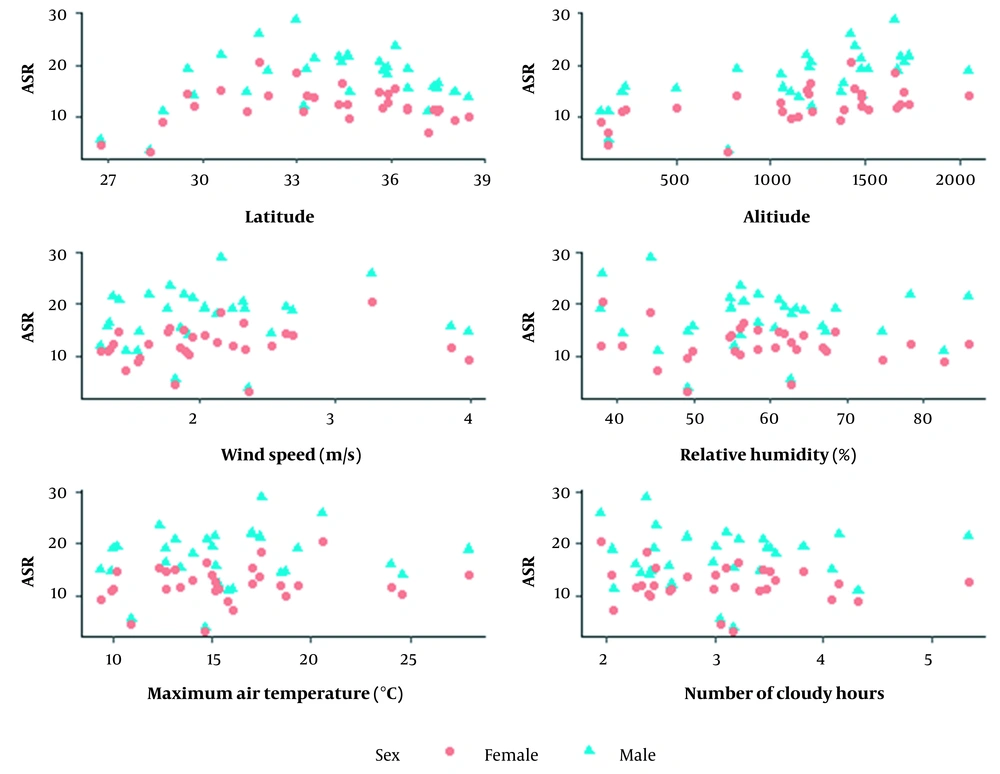
Figure 1 represents the relationship between ASR of skin cancer, and climatic and geographic variables. The figure shows that some geographical and climatic factors have an impact on the ASR of skin cancer. It shows a non-linear association between latitude and skin cancer incidence.
We applied a mixed-effects polynomial regression model with an unstructured covariance matrix of error. This model was chosen based on the BIC. Based on the results, the linear part of the ASR trend of skin cancer was negatively significant (P < 0.001). Also, the quadratic part of the ASR trend was positively significant (P < 0.001). However, the positive sign of the quadratic term reveals the deceleration in the rate of skin cancer incidence. The cubic term of time was positively significant (P < 0.001). This suggests upward trend reverses with increasing time. ASR of skin cancer for males was more than the females (P < 0.001). The positive linear effect of latitude was significant (P = 0.002), but there was a negative quadratic effect of latitude on skin cancer incidence (P = 0.002). This means, although skin cancer incidence increased with rising latitude there was a deceleration in the growth rate of skin cancer incidence by increasing the latitude. Furthermore, there was a positive significant association between skin cancer incidence and altitude (P = 0.045). The wind speed, number of cloudy hours, air temperature, and relative humidity were not associated with skin cancer incidence (P > 0.005) (Table 1).
| Coefficient | SE | P-Value | |
|---|---|---|---|
| Intercept | -285.397 | 87.311 | 0.001 |
| Time (y) | -2.841 | 0.973 | 0.004 |
| Quadratic form of time | 0.926 | 0.211 | < 0.001 |
| Cubic form of time | -0.058 | 0.012 | < 0.001 |
| Gender (male) | 5.147 | 0.320 | < 0.001 |
| Latitude | 17.582 | 5.104 | 0.002 |
| Quadratic form of latitude | -0.268 | 0.078 | 0.002 |
| Altitude (m) | 0.005 | 0.002 | 0.045 |
| Number of cloudy hours | 0.210 | 1.856 | 0.911 |
| Average of relative humidity | 0.137 | 0.100 | 0.187 |
| Average of wind speed (m/s) | -0.286 | 1.034 | 0.785 |
| Average of maximum temperature (°C) | 0.025 | 0.305 | 0.937 |
The Impact of Meteorological and Environmental Factors on Skin Cancer Incidence
5. Discussion
In the present study, we determined the effects of gender, climatic parameters, and geographical factors on skin cancer incidence. Findings showed that there was a decreasing linear trend of skin cancer in Iran. Based on the results, the incidence rate of skin cancer for males was more than the females. This difference seems quite natural. Because the protective measures and clothing differ for men and women. Also, men are more exposed to the risk factors of skin cancer because of the type of job they do. In addition, men take fewer protective measures against the sun's harmful rays. This finding is consistent with the global burden of cancer study (GLOBOCAN 2018) estimates of cancer incidence and mortality produced by the International Agency for Research on Cancer. Based on this report, the ASR of non-melanoma skin cancer for men was greater than of females from different regions of the world (33).
There are controversies about the association between latitude and skin cancer incidence. Based on the Madan et al. study, there was an inverse association between latitude and the incidence of skin cancer (34). Wakeford indicated that a reduction of latitude is associated with increasing an incidence of skin cancer in white people of the same race (27). Whereas, in 2017, Rivas et al. found that there was a strong positive correlation between latitude and melanoma skin cancer mortality and a negative association between skin cancer incidence and latitude (26). Furthermore, based on our results, a positive association was found between latitude and ASR of skin cancer. This result was obtained based on adjusting the effect of latitude in the presence of other variables. Also, this finding is in line with studies in Iran in which some provinces that are located in the south of Iran have had lower skin cancer incidence than the other provinces (17, 35). Furthermore, arid and semi-arid regions of central Iran include Dasht-e Kavir and Lot plain (36). Some studies in Iran have also reported a high incidence of skin cancer in the central part of the country (37). It may be due to the existence of desert regions or high farming jobs. Cahoon et al. and Yadav and Banerjee found that ultraviolet radiation levels vary based on environmental and meteorological factors (38, 39). There was a direct relationship between ultraviolet radiation levels and low relative humidity, lack of rainfall, low wind speed, days of higher ultraviolet radiation, and near-equatorial latitudes (38).
We found a positive effect of altitude on skin cancer incidence. It may be due to the positive association of ultraviolet radiation dose with altitude (28). Unprotected prolonged exposure to sunlight is one of the important risk factors for skin cancer due to the sun's ultraviolet radiation. That is the result of the thinning of the ozone layer. In addition to inappropriate diets, genetic characteristics of people are known as individual factors affecting on skin cancer (7, 15, 24, 40, 41). The ultraviolet radiation of sunlight that passes through the atmosphere is absorbed by ozone and water vapor. Environmental factors such as sun height, latitude, cloud cover, altitude, and ground reflection effect ultraviolet radiation. Higher altitude, proximity to the equator, higher sun height (occurs at solar noon), ozone depletion, and presence of reflectors such as snow increase the amount of ultraviolet radiation. Ultraviolet radiation is high in the sky without cloud (42).
In the present study, we obtained the adjusted effects of the employed covariates. Since disability, mortality, and treatment cost of skin cancer is notable (3, 43), prevention planning is essential for health managers. Furthermore, finding the impact of important climatic factors on skin cancer will help health policy makers to develop specific care plans for different regions.
5.1. Conclusions
According to the results of this study, the incidence of skin cancer in the central regions of Iran is more than in the south and the north. As altitude increases, skin cancer incidence increases. Furthermore, the incidence of skin cancer for males was more than the females. In the aim of the preventive intervention, one most important determinant is individual behavior which should be attention. Therefore, health policymakers in their planning should consider geographical factors as influencing factors for skin cancer. Moreover, more training programs for the male target group for prevention and protection measures are needed.