1. Background
Idiopathic Granulomatous Mastitis (IGM), also known as idiopathic lobular granulomatosis mastitis, is a rare and uncommon inflammatory disease of the breast with an unknown cause (1, 2). It is usually unilateral, but it can be bilateral or subsequently developed in another breast (2). The disease usually occurs in young women of reproductive age (usually during the first 5 years after pregnancy) and the third and fourth decades of life (3). However, it has been reported in Nulliparous women and men (4). Various studies have reported that IGM accounts for 24% of all inflammatory breast disorders, with an annual incidence of 2.4: 100,000 in women (5).
The most common manifestation of IGM is a palpable mass in one or both breasts, measuring 1 to 5 cm and even more. It may be accompanied by tendonitis, erythema, sinus duct formation with drainage, or edema in the breast, which could clinically mimic a bacterial abscess or breast cancer (6, 7). Although IGM is a benign disease, it can clinically and radiologically mimic the symptoms of breast cancer (7, 8). Clinically, IGM may present as a peripheral inflammatory mass of the breast (3).
Sinus formation, Nipple retraction, peau d'orange-like changes, and axillary adenopathy can also occur (9). On the other hand, patients with IGM may have recurrent abscesses over weeks to months; so, these findings may be confused with breast cancer or malignancy (9, 10). For this reason, diagnosing and treating the disease has become a challenge.
Many factors including autoimmune disorders, hormonal disorders, trauma or local immune response, local stimulants, various organisms, viruses, hyperprolactinemia, diabetes mellitus, alpha-1-antitrypsin deficiency, tobacco use, urinary tract ectasia, and use of contraceptive pills are mentioned in the etiology of this disease (1, 6). Also, pregnancy, lactation, and hyperprolactinemia with galactorrhea are other possible causes (6).
Differential diagnoses of IGM include diseases such as tuberculosis, histoplasmosis, or rarely sarcoidosis, and reactions due to foreign bodies that may cause granulomatous mastitis (11, 12). These causes must be determined by biopsy or microbiological examination (11).
With this description, the diagnosis of IGM is often delayed because the clinical symptoms are different and usually vary from case to case (13). Since other diseases mimic IGM imaging and clinical symptoms, diagnosing becomes a challenge (7). The best way to diagnose is through observation and clinical examination.
The initial and choice imaging examination is ultrasound, which usually shows a solid mass, often accompanied by abscesses-like formation (7, 14). The definitive diagnosis of IGM is made by tissue diagnosis through core biopsy (14, 15). In cases of clinical suspicion of diagnoses such as infections, for follow-up and accurate diagnosis, culture and gram and fast acid staining should be prepared from the biopsy (13).
Biopsy evaluation results typically show granulomatous formations, which are centered on lobules (15). Neutrophils are commonly seen, and even micro-abscesses of neutrophils and eosinophils may be seen. Acidophil necrosis and atypical cells should not be seen in the specimen, and no organisms should be present (16).
The treatment management of these patients can be challenging. Many treatments and algorithms have been described, including close follow-up, antibiotic therapy, surgical removal, systemic steroids, immune system suppressants, and mastectomy (17).
Studies conducted in Iran to investigate the incidence and factors associated with IGM are rare. For example, in a study over 5 years in 3 medical centers, only 112 people were evaluated (18). While in our study, more patients were evaluated over a longer time (10 years).
In the meantime, the choice of primary treatment among the articles is different and controversial, and the treatment depends on the size of the lesion, the severity of the symptoms, and the patient's overall health, as well as the surgeon's experience and the patient's treatment preference (19). However, there is no standard treatment, and recurrence rates have been reported between 20% and 50% (20). However, various studies have shown that the disease is self-limiting and that half of the cases are cured within 24 months (20, 21).
All abscesses should be treated with skin aspiration (22). After abscess aspiration, prevention with broad-spectrum antibiotics is recommended during the diagnostic evaluation period (23, 24). Nonsteroidal anti-inflammatory drugs (NSAIDs) also help relieve the inflammatory pain of these IGM masses, which have been very successful in controlling pain (3, 25). Another treatment is systemic oral steroids, which many patients and physicians are reluctant to use due to high-dose steroids. Also, the use of topical steroids has been shown to have fewer side effects than systemic oral food and is safe and effective (26).
Therefore, due to the unknown pathogenesis of IGM and the lack of unity in the treatment of this disease, drugs with significant side effects and invasive methods such as unnecessary mastectomies are used (27). In this study, patients were treated with the primary treatment, which was drainage and analgesic drugs, and some cases with the systemic sign of superimposed infections received antibiotics in addition to the primary treatment. Also, some cases received corticosteroids with these treatments.
2. Objectives
Due to the rare and limited number of studies in Iran, this study was designed and conducted to evaluate patients' clinical characteristics and treatment management with IGM. In this way, valuable data about this disease can be obtained about patients' causes, clinical features, and treatment outcomes.
3. Methods
In this cross-sectional and retrospective descriptive-analytic study, the necessary permits and the ethical code of medical research were obtained to access patients' data (ethic code Nu: IR.SBMU.CRC.REC.1399.021).
The sampling method was a census. All existing patients' data in the pathology departments of the Cancer Research Centers of SBMU with the diagnosis of IGM in the last 10 years (from 2010 to 2019) were evaluated. In the study, there were 293 patients in this period. Patients’ data were disaggregated based on the referring center.
The pathology report of these patients was printed, and their results were recorded on a checklist. Document number, age, sex, location of the disease, and telephone number of patients were extracted from their files.
Patients were contacted by telephone to visit clinically or collect additional information about variables that were not registered in the documents, such as early symptoms at diagnosis, the number of children, history of breastfeeding to children, history of the underlying disease and autoimmune diseases, type of treatment performed for the patient, and recurrence.
3.1. Data Analysis
After collecting and classifying the data, they were entered into SPSS software version 24 and analyzed. Tables and graphs were used to describe the qualitative data. The relationship between qualitative variables was performed, using the chi-square test. All analyzes were bilateral, and the significance level was determined at P < 0.05.
4. Results
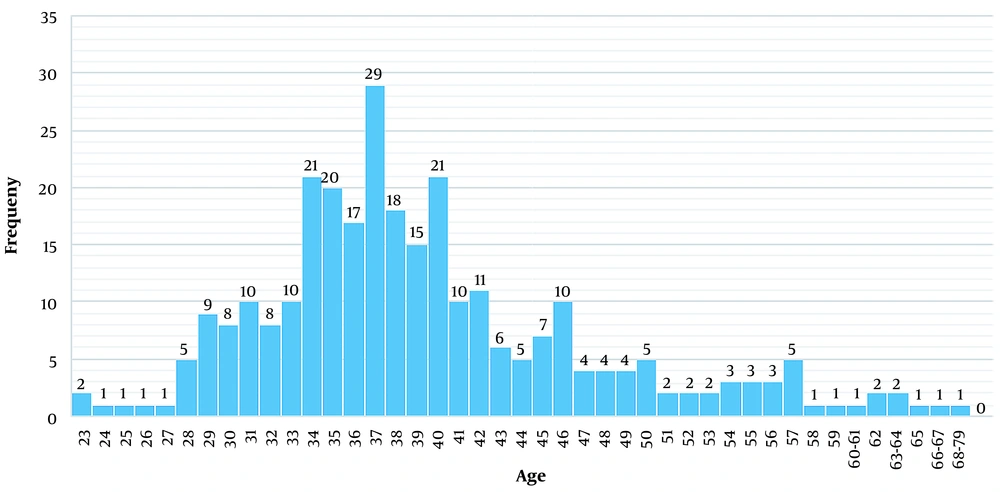
In this study, 303 patients with a diagnosis of IGM were evaluated, 9 of whom were excluded due to incomplete medical documents and lack of follow-up, and, finally, 293 patients were evaluated. It should be noted that there were 2 cases of male patients and 1 case of death among all patients (The cause of death was not related to IGM). Only 1 case of breast cancer had a confirmed pathology among patients. The mean age of patients was 39.21 (ST = 8.29) years, the minimum age of patients was 23 years, and the maximum age of patients was 79 years (Figure 1).
Among the studied patients who had a history of pregnancy, the highest number of deliveries was 2 times (n = 107, 38.1%), followed by 1 delivery (31%) and 3 deliveries (18.1%). Among women who had a history of pregnancy, 66 (23.5%, total = 281) had a history of abortion. In this study, women without a history of pregnancy and single women had no history of abortion.
The average duration of breastfeeding in women with a history of breastfeeding was 36.44 (SD = 23.43) months; 111 cases (40.4%) had less than 24 months, and 164 cases (59.6%) had more than 24 months of breastfeeding history (Table 1).
| Variables | Frequency (%) |
|---|---|
| Age category, y | |
| 20 - 30 | 28 (9.6) |
| 30 - 45 | 208 (71.0) |
| > 45 | 57 (19.5) |
| Gestation (yes) | 281 (95.9) |
| Number of pregnancies | |
| Once | 87 (31.0) |
| More than once | 194 (69.0) |
| Breastfeeding history | |
| Yes | 275 (93.9) |
| No | 18 (6.1) |
| Breastfeeding, mo | |
| < 24 | 111 (40.4) |
| > 24 | 164 (59.6) |
| Underlying disease (yes) | 20 (6.8) |
Twenty cases (6.8%) had an underlying disease, among which the most common underlying disease was diabetes (7 cases, 2.4%), followed by collagen vascular disease (4 cases, 1.4%) and hypothyroidism (1.4%), and TB (3 cases, 1%), respectively. A case of multiple sclerosis has also been reported among patients (Table 1).
Breast involvement in patients in 236 cases (80.5%) was unilateral and bilateral in 57 cases (19.5%). In 50 cases (17.1%), the involvement was Pere-Areola, and in the remaining cases (82.9%), there was involvement in other areas (Table 2).
| Variables | Frequency (%) |
|---|---|
| Breast involvement side | |
| Unilateral | 236 (80.5) |
| Bilateral | 57 (19.5) |
| Affected areas of the breast | |
| Pere-areola | 50 (17.1) |
| Other | 243 (82.9) |
| Systemic symptoms (yes) | 99 (33.8) |
| Type of treatment | |
| Conservative therapy | 178 (60.8) |
| Antibiotic therapy + analgesia + drainage | 66 (22.5) |
| Antibiotic therapy + analgesia + drainage + corticosteroid | 41 (14.0) |
| Other (immunosuppression or surgery) | 8 (2.7) |
| Duration of disease, mo | |
| < 12 | 156 (53.2) |
| > 12 | 137 (46.8) |
| Recurrence after one year of treatment (yes) | 29 (9.9) |
| Complications (scar or breast skin color change) (yes) | 70 (23.9) |
| Last patient status (final outcome) | |
| Cure | 232 (79.5) |
| The patient is under treatment | 43 (14.7) |
| Recurrence-IGM | 17 (5.8) |
Ninety-nine cases (33.8%) of patients had systemic symptoms (fever, general weakness, fatigue, myalgia, etc.) and local symptoms. The most common type of treatment was conservative therapy (analgesia + drainage) (178 cases, 60.8%), which was the primary treatment in our study; 66 patients (22.5%) received antibiotic therapy + analgesia + drainage, and 41 (14%) cases received corticosteroid in addition to antibiotic therapy + analgesia + drainage treatment. Eight cases (2.7%) had received only immunosuppressive treatment or only surgery (These treatments were performed in other centers) (Table 2).
The mean duration of the disease in the studied patients was 18.47 (ST = 18.87) months; so, the minimum duration of the disease was 15 days, and the maximum time was 120 months. In 137 cases (46.8%), the duration of the disease was more than 12 months. Patients were evaluated 1 year after treatment, and 29 cases (9.9%) had recurrence after 1 year (Table 2).
Seventy cases (23.9%) had complications (scar and breast skin color change). The outcome and the latest condition of the patients were evaluated; 232 cases (79.5%) were completely cured with the performed treatments, 17 cases (5.8%) had a recurrence of symptoms, and 14.7% of the patients were still receiving treatment. One case of death was excluded from the evaluation of the outcome (Table 2).
The relationship between different variables with recurrence after 1 year after treatment, complications, and outcome (patient's prior status) was examined; the results are shown in Tables 3 to 5.
| Variables | Recurrence After 1 Year of Treatment | P-Value | |
|---|---|---|---|
| Yes | No | ||
| Age, y | 0.873 | ||
| 20 - 30 | 2 (7.1) | 26 (92.9) | |
| 30 - 45 | 21 (10.1) | 187 (89.9) | |
| > 45 | 6 (10.5) | 51 (89.5) | |
| Breastfeeding | 0.321 | ||
| No | 3 (16.7) | 15 (83.3) | |
| Yes | 26 (9.5) | 249 (90.5) | |
| Gestation | 0.423 | ||
| No | 2 (16.7) | 10 (83.3) | |
| Yes | 27 (9.6) | 254 (90.4) | |
| Number of pregnancies | 0.741 | ||
| Once | 9 (9.1) | 90 (90.9) | |
| More than once | 20 (10.3) | 174 (89.7) | |
| Duration of disease, mo | 0.004 b | ||
| < 12 | 8 (5.1) | 148 (94.9) | |
| > 12 | 21 (15.3) | 116 (84.7) | |
| Breast involvement side | 0.502 | ||
| Unilateral | 22 (9.3) | 214 (90.7) | |
| Bilateral | 7 (12.3) | 50 (87.7) | |
| Underlying disease | 0.987 | ||
| No | 27 (9.9) | 246 (90.1) | |
| Yes | 2 (10.0) | 18 (90.0) | |
| Type of treatment | 0.032 b | ||
| Conservative therapy | 16 (9.0) | 162 (91.0) | |
| Antibiotic therapy + analgesia + drainage | 4 (6.1) | 62 (93.9) | |
| Antibiotic therapy + analgesia + drainage + corticosteroid | 9 (22.0) | 32 (78.0) | |
| Other (immunosuppression or surgery) | 0 (0.0) | 8 (100.0) | |
a Values are expressed as No. (%).
b The P-value is less than 0.05 and means the statistically significant relationship.
| Variables | Complications (Scar or Breast Skin Color Change) | P-Value | |
|---|---|---|---|
| Yes | No | ||
| Age, y | 0.663 | ||
| 20 - 30 | 7 (25) | 21 (75) | |
| 30 - 45 | 52 (25) | 156 (75) | |
| > 45 | 11 (19.3) | 46 (80.7) | |
| Gestation | 0.030 b | ||
| No | 6 (50.0) | 6 (50.0) | |
| Yes | 64 (22.8) | 217 (77.2) | |
| Breastfeeding | 0.332 | ||
| No | 6 (33.3) | 12 (66.7) | |
| Yes | 64 (23.3) | 211 (76.7) | |
| Breastfeeding, mo | 0.225 | ||
| < 24 | 30 (27.0) | 81 (73.0) | |
| > 24 | 34 (20.7) | 130 (79.3) | |
| Duration of disease, mo | 0.005 b | ||
| < 12 | 27 (17.3) | 129 (82.7) | |
| > 12 | 43 (31.4) | 94 (68.6) | |
| Underlying disease | 0.507 | ||
| No | 64 (23.4) | 209 (76.6) | |
| Yes | 6 (30.0) | 14 (70.0) | |
a Values are expressed as No. (%).
b the P-value is less than 0.05 and means the statistically significant relationship.
| Variables | Last Patient Status (Outcome) | P-Value | ||
|---|---|---|---|---|
| Recurrence-IGM | The Patient is Under Treatment | Cure | ||
| Age, y | 0.179 | |||
| 20 - 30 | 2 (7.1) | 3 (10.7) | 23 (82.1) | |
| 30 - 45 | 12 (5.8) | 37 (17.9) | 158 (76.3) | |
| > 45 | 3 (5.3) | 3 (5.3) | 51 (89.5) | |
| Breastfeeding, mo | 0.414 | |||
| < 24 | 8 (7.2) | 17 (15.3) | 86 (77.5) | |
| > 24 | 6 (3.7) | 24 (14.7) | 133 (81.6) | |
| Gestation | 0.244 | |||
| No | 2 (16.7) | 2 (16.7) | 8 (66.7) | |
| Yes | 15 (5.4) | 41 (14.6) | 224 (80.0) | |
| Number of pregnancies | 0.095 | |||
| Once | 10 (10.1) | 17 (17.2) | 72 (72.7) | |
| More than once | 7 (3.6) | 26 (13.5) | 160 (82.9) | |
| Breast involvement side | 0.109 | |||
| Unilateral | 11 (4.7) | 38 (16.1) | 187 (79.2) | |
| Bilateral | 6 (10.7) | 5 (8.9) | 45 (80.4) | |
| Affected areas of the breast | 0.083 | |||
| Pere-areola | 5 (10.0) | 11 (22.0) | 34 (68.0) | |
| Other | 12 (5.0) | 32 (13.2) | 198 (81.8) | |
| Underlying disease | 0.524 | |||
| No | 15 (5.5) | 39 (14.3) | 218 (80.1) | |
| Yes | 2 (10.0) | 4 (20.0) | 14 (70.0) | |
a Values are expressed as No. (%).
Recurrence after 1 year in patients who had a longer duration of disease (more than 12 months) was higher than in those who had a shorter period (less than 12 months) (15.3% vs. 5.1%, P = 0.004). Also, the highest recurrence rate was in the group receiving corticosteroids compared to the group receiving the usual treatment and usual treatment plus antibiotics. This relationship was statistically significant (22.0% vs. 9 % and 6.1%, respectively, P = 0.032) (Table 3).
Complications (scar or breast skin color change) were significantly higher in patients without a pregnancy history than in patients who had pregnancy (50.0% vs. 22.8%, P = 0.030). Also, these complications were significantly higher in patients who had a longer duration of illness (more than 12 months) than in shorter periods of illness (less than 12 months) (31.4% vs. 17.3%, P = 0.005) (Table 4).
It should be noted that there was no relationship between the last patient and the variables listed (Table 5).
5. Discussion
IGM is a disease with unknown pathogenesis and unclear treatment. Most clinicians use different methods to treat this disease, from drug therapy to surgery, corticosteroid therapy, or even immunosuppression, which can have different consequences (1, 4, 28). In Iran, clear information about the characteristics of this disease is not available among the people involved, and the number of studies conducted on this disease is lacking.
In many cases, due to the imitation of the symptoms of breast cancer by this disease, wrong treatments and diagnoses are performed, which will have a bad financial and psychological burden on the patient and the health system.
Therefore, we decided to conduct a study to evaluate the clinical features and management of treatments performed on patients with IGM diagnosis, which has been retrospectively over 10 years. This is one of the strengths and unique points of this study. This study included a study of 293 patients, and the high statistical population of this study is also of great importance.
In the present study, the highest frequency of patients was 30 to 45 years, and the average age of patients was about 39 years old. Breast involvement in most cases (80.5%) was unilateral, and only 17% of the involvement was Pere-Areola. The most common type of treatment was conservative therapy (analgesia + drainage) (60.8%), which was the main treatment in our study; 22.5% received antibiotic therapy + analgesia + drainage, and 14 % of cases received corticosteroid in addition to this treatment. Based on these 2 common treatments, 9.9% had recurrence after 1 year. Finally, the overall recurrence rate was 5.8%, and 79.5% were completely cured. Complications of the disease were seen in 23.9% of patients.
In this study, 6.8% had the underlying disease, and the presence of the underlying disease was not related to patients' recurrence, complications, and outcome. The rate of 1-year recurrence in patients with no history of pregnancy and breastfeeding and a longer duration of the disease was higher. On the other hand, the complications of this disease were higher in patients with no history of pregnancy and a longer duration of the disease.
Studies have been conducted in this regard; for example, in the study of Azizi et al. (16) in 2019, the recurrence rate was 24.8, and breast skin lesions were more likely to recur, which was much higher than in our study. In another study by Patmano et al. (5), in 2019, patients were treated surgically with/without corticosteroids, which had a lower recurrence in the surgical group (6.7%) than in the steroid group (20%) during follow-up. However, no significant difference was observed between the groups.
Also, in our study, the highest recurrence rate was in the group receiving corticosteroids compared to the group receiving the usual treatment, and it was statistically significant. However, in a study by Mahmodlou et al. (29), it was concluded that steroid therapy as a treatment method (such as prednisolone) along with reducing inflammation is an effective and practical choice in the treatment of IGM, which indicates a discrepancy in the results of the studies. However, based on our study, corticosteroid therapy seems associated with more recurrence. In 2015, Yabanoglu et al. (30) concluded that surgical treatment was more effective than conservative treatment with less recurrence; however, the recurrence rate was 11.7% among all patients. In the study of Kadivar et al. (18), only 9% of patients experienced a recurrence of symptoms during different treatment protocols used in Iran. In this study, the etiological role of pregnancy and breastfeeding history is also emphasized.
Finally, it can be concluded that the exact treatment of this disease is still unclear and requires further studies in this field. The difference between the present studies and our study may be due to differences in sample size, differences in the type of study design, and different treatments.
5.1. Conclusions
The results of our study and its comparison with the results of other studies still emphasize the uncertainty of the etiology of IGM disease and its treatment. However, to some extent, our study has shown that conservative treatment (drainage with analgesic drugs) is one of the best treatment options. Also, corticosteroid therapy is associated with a higher recurrence rate, but more studies are needed.