1. Context
Chemotherapy is a complex process and is highly prone to errors (1). These types of errors are considered the second most common cause of fatal medication errors (2). Some of the reasons that can cause serious and irretrievable risks to the patient's health during the chemotherapy process are as follows: (A) The use of cytotoxic drugs that have a narrow therapeutic index, (B) the need for drug dose adjustment requiring several parameters such as weight, age, and body surface area (3, 4), (C) the necessity of adjusting the correct frequency for chemotherapy (5), (D) patients with cancer are more sensitive and at more serious risks due to the effects of cancer on physiological status, patient's vital organs, and immune system (6). Due to the complexity and high risk of the chemotherapy process, these errors can occur at any phase of the chemotherapy process, including prescribing (all incidents and errors that occur to the patient during the decision-making and prescribing process), dispensing, and transcribing, including all errors and issues related to product labeling, packaging, distribution, and composition of drugs; monitoring phase (all the events associated with the monitoring of clinical or laboratory data that show the patient's response to the prescribed medication) and the administration phase (all the errors that occur when the drug is given to the patient). According to studies, the highest rate of medication errors is assigned to the prescription process (2, 7, 8).
Different strategies have been proposed to prevent or reduce chemotherapy medication errors. These include continuous training of healthcare providers, development of advanced drug surveillance systems, development and improvement of error reporting systems, the standardization of the preparation, labeling, and distribution process, use of pre-printed standard forms, development of computerized provider order entry systems (CPOE), and clinical decision support systems (CDSSs) (9-16). The term CDSS is used for a wide range of computer tools used to assist physicians in decisions making with the ultimate aim of improving patient care and safety (17, 18). Nowadays, CPOE systems are enabled with CDSS systems to improve the functionality of these systems to ensure optimization of, and reduction in, drug-related errors through alerts creation (19-23). The integration of the CPOE systems with CDSSs provides capabilities such as automatic elimination of interpretation and transcription errors improves the availability of dosage information and medication plans, enables automatic calculation of drug doses, generates alerts, and provides the possibility of checking errors. With these features, a CPOE system can effectively and safely assist the healthcare team in providing high-quality care (3, 18, 24, 25). The CPOE systems have the capability of supporting physicians in prescribing medications, requesting laboratory tests, or asking for consultations. These systems can reduce or prevent medication errors and improve patient safety (17, 18). The CPOE systems have specific features such as automating the medication prescription as they can allow standard, complete, and legible prescriptions (19-21).
Several studies have been conducted to evaluate the impact of CPOE systems on chemotherapy medication errors in cancer care units. However, to the best of our knowledge, there has been limited research with a focus on the impact of CPOE on the incidence of chemotherapy medication errors, the severity of errors, and adverse drug events (ADEs) in cancer care units.
Published systematic studies have attempted to investigate the impact of CPOE in other medical specialties. For example, Prgomet et al. conducted a systematic review about the impact of CPOE on medication errors, length of stay, and mortality in intensive care units (17). Van Rosse et al. systematically reviewed the impact of CPOE on medication errors and ADEs in pediatric and intensive care units (26). Another study by Georgiou et al. discussed the effects of the CPOE system on medication errors in the emergency department (27). In addition, there have been other systematic reviews that have analyzed the impact of CPOE on medication safety and ADE in other hospital units (19, 28-34). Previous systematic reviews have shown that the CPOE system significantly increases the safety of the medication process by preventing or reducing the number of medication errors and ADEs. However, these systems are not error-free. Errors can occur for 5 various reasons, such as increased system workload, lack of positive feeling of end-users to use the system, constant need for updates, implementation problems, and user errors while using CPOE.
2. Objectives
The aim of the current study is to systematically review the impact of CPOE systems on the incidence of chemotherapy medication errors, the severity of errors, and ADEs.
3. Data Sources
The literature search was conducted, using 5 databases of PubMed, EMBASE, Scopus, Web of Science, and ScienceDirect between 2000 and 2020. We also checked the grey literature, but no relevant publication was found concerning the inclusion criteria. The search strategy was developed by using a combination of keywords and Medical Subject Headings (MeSH) related to CPOE, medication errors, chemotherapy, and cancer care unit. We used these groups of keywords in the following 2-step process: (1) Keywords and MeSH terms in every three groups of A, B, and C were combined by the operator “OR”, (2) groups A, B, and C were, then, combined, using “AND” to search studies about CPOE system and medication errors in cancer care units. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) protocol was used as guidance for reporting studies in this systematic review (35). Table 1 shows the keywords and the search strategy used in searching databases for relevant articles.
| Search Strategy | |
|---|---|
| A | “Medical Order Entry System” OR “Computerized Provider Order Entry System” OR “Computerized prescriber order entry” OR “Computerized physician order entry” OR “Electronic physician order entry” OR “Electronic order entry” OR “Computerized Order Entry” OR “Electronic Prescribing” OR “CPOE” OR “Clinical Decision Support Systems”, OR “CDSS” OR “DSS” |
| B | “Medication error” OR “Error reporting” OR “Error reduction” OR “Patient safety” OR “Safety” |
| C | “Chemotherapy” OR “Cancer Care Unit” OR “Oncology department” OR “Oncology Service Hospital” OR “Neoplasm” OR “Chemotherapy services” |
4. Study Selection
All available titles and abstracts of articles were checked by 3 authors (MA, RR, AH) to identify the studies that need further evaluation according to pre-determined inclusion and exclusion criteria. After removing duplicate papers, all non-English papers, review studies, and conference abstracts were excluded, and full-text papers (if available) were included if they met 3 main criteria: (1) they investigated the CPOE system, (2) they were carried out in the oncology department, which provided chemotherapy services to patients with cancer on an outpatient or inpatient basis, and (3) they reported medication errors in cancer care.
5. Data Extraction
We defined medication errors, as the errors in any step of the medication process including prescribing, transcribing, dispensing, and administration of a drug, which could harm the patient (28). Concerning the severity of errors, the National Coordinating Council for Medication Error Reporting and Prevention System (NCC MERP) developed an index that classifies errors based on the severity of the outcome (Appendix A in the Supplementary File) (36). Additionally, ADEs are drug-related injuries to patients (37).
The included papers and data were extracted by one of the authors (MA) and then approved by two other authors (AH and RR). To extract the specific details of each study, a data extraction form was used based on the objectives of the study. This form included items such as author, year of publication, country of study, type of study, objectives of the study, and main findings (Table 2). All eligible articles were qualitatively evaluated with a tool provided by Downs and Black (38).
| Author | Date of Publication | Country | Type of Study | Main Objectives | Main Findings and Results (Impact of CPOE) |
|---|---|---|---|---|---|
| Huertas Fernandez et al. (39) | 2006 | Spain | Case / control study design | Investigate the incidence of medication errors in the CPOE system in comparison with the paper-based method | Significant reduction of medication errors after using the CPOE system. The average incidence of drug errors in prescribing chemotherapy in the CPOE system was zero (range 1 - 0) and for manual paper-based prescriptions 5 (range 12 - 1) (P < 0.001). |
| Harshberger et al. (18) | 2011 | USA | Retrospective comparison in practices with CPOE and handwritten orders | Describe prescription completeness and safety events per CPOE and paper-based ordering method | The use of CPOE has led to the identification and improvement of significant sources of medication errors. The completion of CPOE versions and manual paper-based systems have been reported as 93% and 63%, respectively. |
| Martin et al. (40) | 2015 | United States | Pre/post | Establish CPOE for chemotherapy ordering and monitoring CPOE-related safety events | In the first year after using the CPOE system, drug errors increased (90 vs. 86). In the second year, the total number of drug errors decreased by roughly 20%. |
| Aita et al. (3) | 2013 | Italy | Prospective observational study of developed CPOE | Assess the frequency, type, and actual severity of medication errors per CPOE used system | The incidence of errors is reported to be 8%. The CPOE system needs to be properly designed before the performance. |
| Chung et al. (41) | 2018 | USA | Comparison in practices with CPOE andpaper-based orders | Establish CPOE for chemotherapy ordering and monitor CPOE-related safety events | 75% of medication errors, as well as major errors, were reduced after the CPOE system. (60 errors among 60 prescriptions of chemotherapy before CPOE were reduced to 10 errors among 40 prescriptions of chemotherapy using CPOE, P < 0.05) |
| Meisenberg et al. (42) | 2014 | USA | Retrospective comparison in practices with CPOE and paper-based orders | Measure the incidence and type of chemotherapy errors in 3 different approaches to chemotherapy prescribing | Chemotherapy prescriptions of the CPOE system have 100% accuracy and 10% to 44% of errors occur in the traditional-paper prescription method. |
| Voeffray et al. (43) | 2014 | Switzerland | Pre/post | Investigate the impact of CPOE on errors in prescribing chemotherapy drugs | Before the CPOE system, 141 errors were recorded out of 940 chemotherapy prescriptions (15%). After CPOE, only 6 errors (1%) were recorded in 527 prescriptions. |
| Aziz et al. (24) | 2015 | Pakistan | A prospective, controlled cross-sectional comparative study | Investigate the hypothesis that the CPOE system reduces the incidence and severity of chemotherapy protocol errors. | The number of medication errors in the CPOE system (N = 10) was reduced compared to the paper prescription method (N = 134). |
| Collins and Elsaid (44) | 2010 | USA | Pre/postanalysis | Reduce medication errors in prescribing oral chemotherapy using CPOE | Medication errors were significantly reduced in all phases. (P < 0.023) |
| Kim et al. (45) | 2006 | USA | Pre/postanalysis | To implement and assess the impact of CPOE on reducing Order errors in pediatric chemotherapy | After Cpoe, less inappropriate dose (0.26%, 95% CI, 0.11 to 0.61) incorrect dose calculations (RR, 0.09, 95% CI 0.03 to 0.34) and Missed doses (RR; 32%, 95% CI 0.14 to 0.77) and incomplete nursing checklists (RR 0.51 95% CI, 0.33 to 0.80). |
| Nerich et al. (46) | 2009 | France | Observational study of developed CPOE | Evaluate the occurrence of prescribing medication errors in the cancer care process | The incidence of prescribing errors is 1.5% in the CPOE system compared to other studies (from 2.7 to 12.3% in other studies) |
| Small et al. (47) | 2008 | United Kingdom | Prospective comparison in practices with CPOE and paper-based orders | Compare chemotherapy prescribing errors using CPOE and spreadsheet in the cancer care unit | In 602 orders of SPREADSHEET, Medication error was equal to 20.4%, and out of 1339 CPOE orders, medication was equal to 11.8%. |
| Chen and Lehmann (5) | 2011 | USA | Observational study of developed CPOE | Establish a CPOE system to increase patient safety and electronic chemotherapy ordering | After the application of CPOE, the incidence of chemotherapy has been reduced (67%). The incidence of errors in TRANSCRIPTION =100% reduced. DISPENSING = 44% reduced. ADMINISTRATION = reduced by 33%. |
| Lichtner et al. (8) | 2019 | United kingdom | Observational study of developed CPOE | Prospect medication safety issues by using an electronic medication management system (CPOE). | Out of 610 medication errors, the most errors occurred in the prescription phase (35%) and the administration phase (about 27%). In other drug phases, 5% error was reported in the dispensing stage and 5% in the monitoring stage, respectively. |
This quality assessment tool was composed of 26 items that examined various dimensions of studies, including external validation, internal validation, and bias check with a scoring system (38). It was used independently by two authors (MA and RR) and any disagreement between the authors was resolved through discussion.
6. Results
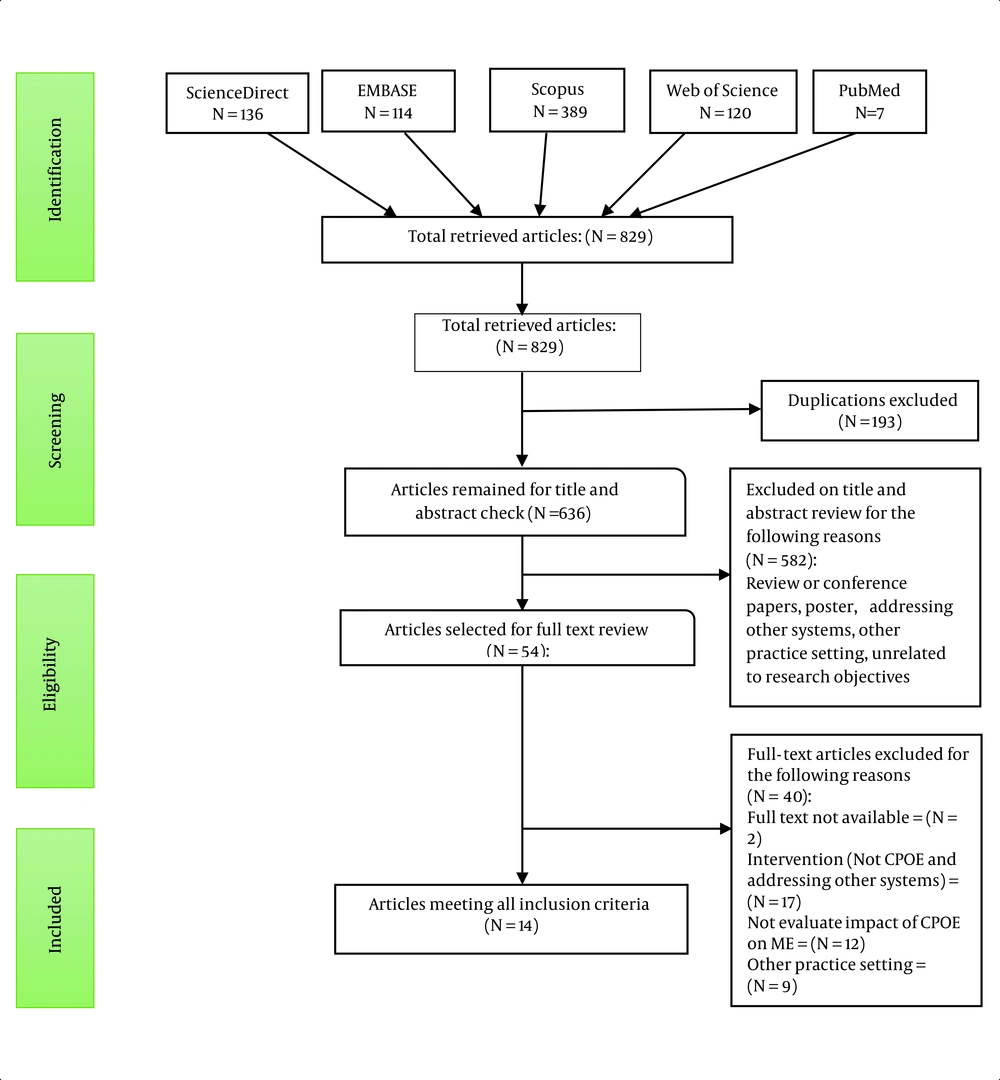
A total of 829 studies were identified by the search; 193 duplicates and 582 unrelated papers were removed. The remaining 54 publications were reviewed, of which 40 studies did not meet the eligibility criteria. Among the excluded papers, 17 studies focused on non-CPOE systems, 12 studies did not report the effect of CPOE on medication errors, the full text of 2 studies was not available and studies were conducted in a different study setting (n = 9). A total of 14 papers published from January 2000 to November 2020 were eligible and included in the study (Figure 1).
6.1. Study Characteristics
The current systematic review examined 14 articles, including 3 studies with the pretest-posttest design method (43-45), 1 case-control study (n = 1) (39), and 9 observational, comparative, and analytical studies (Table 2) (3, 5, 8, 18, 40-42, 46, 47). All 14 studies reported the impact of using the CPOE system on medication errors and medication safety issues. Seven out of 14 studies were conducted in the United States (3, 18, 39-42), 2 studies were performed in the United Kingdom (8, 44) and 1 study in either of the 5 following countries: France, Italy, Switzerland, Spain, and Pakistan. Ten studies (71%) reported the impact of CPOE on chemotherapy medication errors in comparison with the traditional paper-based ordering method (5, 18, 24, 39-44, 47). In 4 studies (29%), researchers developed a CPOE for the oncology department and then assessed user experiences, safety challenges, as well as the effects of the system on medication errors (3, 5, 8, 43, 45).
According to the objectives of the study, our findings were categorized into 4 groups:
6.2. Definitions of Medication Prescription Error in Studies
In these studies, chemotherapy prescription errors were defined as "errors due to incomplete prescription (prescription with missing information or lack of a specific detail) or incorrect prescription (incorrect data or any discrepancy between the prescribed drug and the patient or treatment protocols), and errors related to illegible handwriting and abbreviations" (24, 41). However, the details of specific elements in the definition of medication errors were different (8, 24, 39, 42-44). Definitions of medication prescription errors are available in Appendix A in the Supplementary File.
6.3. Impact of CPOE on Medication Errors Based on the Phase of the Medication Process
Nine studies examined the impact of the CPOE system on medication errors exclusively in the prescription phase, and 5 studies assessed the effects of using CPOE on all phases of the medication process. Table 3 shows the pooled results. In most studies, the CPOE system led to a significant reduction in chemotherapy prescription errors compared with other chemotherapy prescription methods. In a study by Meisenberg et al., prescribing drugs with the CPOE system resulted in a 100% precision in dose, creatinine clearance calculations, demographic information, and signature (42). In other studies, chemotherapy prescription errors were reduced by about 42%, 74%, and 75%, respectively, compared with paper manual prescriptions (24, 41, 47). In a study by Voeffray et al., the average chemotherapy prescription error was reduced 22 times after using the CPOE system (43). However, the authors noted that CPOE did not eliminate all prescription errors, while new types of errors might occur. Small et al. reported that chemotherapy prescribing with the CPOE system was associated with errors such as wrong cycle number or phase and wrong data entered (47). Aita et al. (3) also pointed out the incidence of error after the implementation of the CPOE system as 8%.
| Errors by Phase | Harshberger et al. (18) | Martin et al. (40) | Aita et al. (3) | Chung et al. (41) | Meisenberg et al. (42) | Voeffray et al. (43) | Aziz et al. (24) | Collins and Elsaid (44) | Kim et al. (45) | Nerich et al. (46) | Small et al. (47) | Huertas Fernandez et al. (39) | Lichtner et al. (8) | Chen and Lehmann (5) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prescription | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | ↓ | * | ↓ |
| Transcription | ↓ | * | * | ↓ | ||||||||||
| Dispensing | ↓ | * | * | ↓ | ||||||||||
| Administration | ↓ | * | ↓ | * | ↓ | |||||||||
| Monitoring | ↓ | * | * |
a Symbols: ↓ Significant reduction; * Just reported medication errors per phases
Five studies examined the impact of the CPOE system on medication errors in all the different phases of the chemotherapy process, namely prescription, transcription, dispensing, administration, and monitoring. In 4 studies, each phase of the chemotherapy process improved after the implementation of the CPOE system (5, 8, 44, 45); and only 1 study conducted by Martin et al. reported an increase in errors in the first year of CPOE implementation (90 vs. 86). The reasons for the increase in errors were reported to be the lack of familiarity with the system and improper use of the system. However, the second year of using the CPOE system resulted in a 20% reduction in medication errors compared with the paper-based prescribing approach, administration errors from 30 to 25, dispensing errors from 12 to 10, monitoring errors from 16 to 14, prescribing errors from 10 to 7, and transcribing errors from 18 to 11 (40). In another study by Chen and Lehmann, after implementing the CPOE system, the incidence of chemotherapy medication errors decreased by 67% in the prescribing phase, 100% in the transcription phase, 42% in the dispensing phase, and 33% in the administration phase (5). Having implemented CPOE, Kim et al. reported less chemotherapy prescriptions with inappropriate dose (0.26%, 95% CI, 0.11 to 0.61), incorrect dose calculations (RR, 0.09, 95% CI 0.03 to 0.34), missed doses (RR; 32%, 95% CI 0.14 to 0.77), and incomplete nursing checklists (RR 0.51 95% CI, 0.33 to 0.80) (45). In another study, Lichtner et al. showed that among 610 medication errors, the most errors occurred in the prescription phase (35%) and the administration phase (about 27%) after using the CPOE system. In addition, 5% of errors were reported in the dispensing phase and 5% in the monitoring phase. In this study, the most common errors in the prescription phase pertained to incorrect dosage, prescriptions for the wrong patient, or incorrect formulation of dispensed medications (8).
6.4. Comparing the CPOE System with the Paper-based Ordering Method
Ten studies compared the effects of the CPOE system on chemotherapy medication errors compared with the traditional paper-based ordering method (Table 3). According to Table 4, even with the deployment of the CPOE systems, still there might be medication errors; however, in 90% of studies, the medication errors with CPOE were significantly reduced compared to the conventional prescribing method.
| Author | Paper Base | CPOE |
|---|---|---|
| Huertas Fernandez et al. (39) | The average of medication errors was 5 (range: 1 - 12) (P < 0.001) | The average of medication errors was 0 (range 1 - 0) |
| Harshberger et al. (18) | 67% of paper prescriptions were complete. | Significant reduction of medication errors after using the CPOE system. 93% of the CPOE prescriptions were complete. |
| Meisenberg et al. (42) | The incidence of medication error for paper-based ordering: 30.6% | The incidence of medication error in the CPOE system (2.2%) |
| Small et al. (47) | The incidence of prescribing errors in 602 orders 20.4%. | The incidence of prescribing errors of 1339 orders (11.8%). |
| Voeffray et al. (43) | Out of 940 prescriptions, 141 errors were recorded. | Seventy-five medication errors were recorded for 1505 ordered chemotherapy (5%) |
| Aziz et al. (24) | Out of 5514 prescriptions, the number of medication errors (N = 134) | The incidence of prescribing errors of 1339 orders (N = 10). |
| Chung et al. (41) | Number of prescriptions analyzed: 60; Number of medication errors: 60 | Number of prescriptions analyzed: 40; Number of medication errors: 10 |
| Chen and Lehmann (5) | One year before implementation 132 drug-related events reported | In the first year after implementation, 80 drug-related events were reported. |
| Collins and Elsaid (44) | Number of prescriptions analyzed: 412; Number of medication error: 39 | Number of prescriptions analyzed: 126; Number of medication error: 4 |
| Martin et al. (40) | Chemotherapy-related medication events have been reported in 86 cases. | Increase of errors in the first year of CPOE (N = 90). In the second year of CPOE: The total number of reported errors has decreased by approximately 20%. |
6.5. Impact of CPOE on Severity of Errors and Medication-related Adverse Events
Five studies assessed the impact of the CPOE systems on the severity of error and ADEs (3, 16, 23, 26, 48). Table 4 shows the pooled results. In 80% of studies, the CPOE system reduced the severity of errors and ADEs in the chemotherapy process (3, 16, 23, 48). But, in a study by Small et al. (47) different results were reported compared with other studies. In this study, the incidence of severe and life-threatening errors in the CPOE system increased compared with the paper-based ordering method, and most of the errors in the CPOE system were severe errors. Small et al. reported that the results of the paper-based ordering method were reversed. Serious and life-threatening errors occurred at a lower rate, and most errors were minor (26). Table 5 shows the severity of errors and ADEs in CPOE and paper-based systems.
| Study | The Severity of the Error and Adverse Drugs Event | |
|---|---|---|
| NO CPOE | CPOE | |
| Aita et al. (3) | Not reported | 72% of error=minor; 25% of error= moderate; 3% produce major or catastrophic injuries |
| Meisenberg et al. (42) | 4.2 % of errors lead to serious damage | 0.1 % of errors lead to serious damage |
| Voeffray et al. (43) | 27 (19%) of errors = major; 114 (81%) of errors= minor | Error rate = 1%; all of error = minor |
| Aziz et al. (24) | 35 % of error = serious; 1 error was fatal; 63% of error = significant | Eight were significant. none of the errors was Fatal. 2 errors were serious. |
| Small et al. (47) | Minor error rate: 36.6 %; Significant error : 32.25%; Serious error : 25.2 %; Life threatening error: 5.7 % | Minor error rate: 16.5%; Significant error: 35.4 %; Serious error: 41.8%; Life threatening error: 6.3% |
7. Discussion
To our knowledge, this systematic review is the first study that presents a synthesis of the literature on the impact of the CPOE system on chemotherapy medication errors, the severity of errors, and the incidence of ADEs in cancer care settings, respectively. The findings indicated that the use of CPOE can significantly reduce medication errors in all chemotherapy phases by up to 75%, the severity of errors by 97 to 100%, and ADEs by 80%. We identified a significant reduction in the chemotherapy medication errors, the severity of the error, and the incidence of the ADEs after CPOE system implementation. In addition, we found several issues reported in some studies after using CPOE systems. According to these studies, the CPOE system does not prevent all medication errors and even may cause new errors (42, 46). Meisenberg et al. identified 6 types of CPOE-related errors, 2 of which were capable of causing serious harm to e patients. One of the errors was related to unintended dose-escalation resulting from copying forward a previous dose that had been reduced for toxicity, and the other was the failure to sign one of the 3 chemotherapy drugs in a protocol on the CPOE user interface (42). Nerich et al. (46) also reported that 62.7% of errors in CPOE prescriptions could cause significant or severe harm to patients. A reason for risks associated with the use of CPOE could be designing issues, which could be partly resulted from limited user participation in the development of systems and the user’s lack of skills for appropriate use of the CPOE system. There have been suggestions for eliminating issues with the CPOEs. Chung et al. (41), for example, suggested that for successful implementation of the CPOE system, it is critical to identify the key stakeholders and involve them from the early stages of development of the system. The use of drop-down menus for data entry, the capability of alert generators, and the training of end-users are among the solutions suggested for preventing CPOE-related medication errors reported by Lichtner et al. (8, 41, 42).
Regarding the chemotherapy process phases, 9 of 14 studies reported the impact of the CPOE system on medication errors exclusively in the prescribing phase, and 5 studies assessed the effects of using CPOE on all phases of the chemotherapy process. Before the implementation of the CPOE system, all reviewed studies reported that most errors in the chemotherapy process occur during the prescribing phase (3, 39, 44-46). The findings revealed a significant reduction in medication error during the prescribing phase following the implementation of a CPOE system, except for one study (3). Aita et al., reported an increase in the rate of medication errors during the prescribing phase by 20%, which is higher than other published reports from cancer care settings. The reason for the high reduction in prescribing errors following implementation of a CPOE system could be assigned to some capabilities of CPOE such as automatic calculation of drug dose, the removal of manual data entry, using drop-down meus, as well as alert generation at prescribing stage (24, 41-43, 47). Data from 5 other studies showed that transition from a traditional paper-based prescription system to a CPOE-based system could eliminate or highly reduce the errors related to transcription, dispensing, and administration phases through the integration of CPOE systems with systems such as automatic dispensing cabinets, structuring and standardizing the chemotherapy process, and solving the illegibility issues (5, 8, 40, 44, 45).
Another important aspect of the medication errors was the severity of medication errors and their ADEs. Although it is difficult to accurately assess the impact of the CPOE system on the severity of errors and possible ADEs due to the lack of relevant data, our study showed that 5 studies (36 %) addressed the severity of errors and eliminated ADEs. Aita et al. indicated that only 3% of errors detected after CPOE implementation had the potential for catastrophic events (3). Furthermore, in Meisenberg et al.'s study, the incidence of errors that could seriously harm patients decreased from 4.2% in the paper-based system to 0.1% in a CPOE-based system (42). Voeffray et al. also reported significant effects in preventing major and influential errors (43) as only 1% of errors occurred after CPOE implementation, all of which were reported as minor ones. In another study, Afrash et al. pointed out that implementation of the CPOE system could improve patient safety through reduction or prevention of medication errors (49). Although in previous studies, the CPOE system led to a significant reduction in ADEs and severity of errors, Small et al. reported different results compared with other studies (47). In their study, more severe errors (66 errors for the CPOE system and 31 errors for the paper-based system) and more life-threatening errors (10 errors for the CPOE system and 7 errors for the paper-based ordering method) occurred after the implementation of the CPOE system. Small et al. mentioned that the increased severity of error and ADEs after using the CPOE system were associated with the gemcitabine carboplatin regimen for non-small cell lung cancer, where a new cycle was mistakenly prescribed. These studies suggest that the use of CPOE system could help reduce the severity of errors and ADEs, and as a result, improve patient safety by standardizing the chemotherapy process and improving its completeness.
7.1. Limitations and Strengths
A limitation of this study could be the issue of heterogeneity. Although we acted obsessively at the time of selecting studies and polling results, the review of studies demonstrated that it is difficult to accurately compare the error rates, ADEs, and severity of errors. The issue could be assigned to the terminology used for medication errors, different types of ADEs, the severity of errors, and the use of different CPOE systems in different settings. However, the heterogeneity experienced was not related to the methodological approach of the studies, and inclusion and exclusion criteria were rigorously checked and applied to eliminate the risk of bias.
We comprehensively searched the literature, and the criterion-based selection of publications that solely focused on chemotherapy medication errors, the severity of errors, and ADEs in chemotherapy services could be the strengths of the current study.
7.2. Conclusions
Cancer care settings involve unique complexities that make them vulnerable to chemotherapy medication errors and ADEs. The current systematic review suggests that the use of CPOE can minimize the occurrence of medication errors, the severity of errors, and ADEs; however, they still occur. Most errors are human-related or associated with the design and implementation of the systems. User involvement in the system development process and training of end-users, and the adoption of secure data entry methods could help prevent CPOE-related medication errors. A meta-analysis is highly recommended to provide a quantitative estimation of the effects of the CPOE systems and present statistically stronger findings.