1. Background
The annual incidence of thyroid cancer is increasing rapidly, making it one of the most common endocrine malignancies. The standardized age incidence of this cancer around the world in 2020 was estimated to be 10.1% in women and 3.1% in men (1). Also, the highest mortality rate due to thyroid cancer has occurred in Asia and the mortality rate of thyroid cancer in Iran was reported to be 0.58% per thousand people in 2020 (2). This cancer in Iran was the 5th most common cancer in women, 15th cancer in men, and 11th most common cancer in both genders in 2020 (1) and according to the Iranian Cancer Institute, thyroid cancer contains 1.8% of all cancers and 76.1% of endocrine cancers (3, 4).
Different individual and social factors can be involved in this increase, according to epidemiological studies, obesity, genotype, and exposure to ionizing radiation are among the potential risk factors for this cancer, and nutritional factors such as inadequate or excessive use of iodine, smoking, family history of thyroid cancer, TSH levels, lifestyle, weather conditions, alcohol use, and hormonal factors (especially in women) are also possible risk factors (5, 6).
Several studies have shown that diabetes, obesity, and metabolic syndrome are potential risk factors for cancer, and some studies have concluded that a possible increased risk of thyroid cancer is due to diabetes (7, 8). Studies have also shown that patients with insulin resistance have higher thyroid volume and risk of developing thyroid nodules. A study by Rezzonico et al. (9) found that the percentage of thyroid nodules in the insulin resistance group was significantly higher (61%) and the lowest (16.1%) in the insulin non-resistance group. Seo et al. also in a study showed that type 2 diabetes had a significant effect on thyroid cancer and increased the chance of developing thyroid cancer more than 5 times (10). In a study by Ayturk et al., a significant relationship was between thyroid and metabolic syndrome. The mean thyroid volume in the group of metabolic syndrome with a mean of 17.5 and standard deviation of 5.5 was significantly different from this volume in the control group with a mean of 12.2 and standard deviation of 4.2 (9, 11).
The prevalence of type 2 diabetes around the world has significantly increased in recent years and the age of onset of the disease is reducing. It is estimated that about 102 million people around the world or 5.1% of the adult population have diabetes. And this figure will increase to 6.3% by 2025 (12). The prevalence of this disease has varied from 1.2% to 14.6% in Asia, 4.6 to 40% in the Middle East, and 1.3% to 14.5% in Iran (13).
On the other hand, a study conducted in 2016 showed that the prevalence of thyroid cancer has increased in the second, third, and fourth decades, as well as in those older than 59 years, and the prevalence of this cancer in 2020 in Iran has been estimated to be 4 per 100,000 people (14).
The main causes of type 2 diabetes include insulin resistance due to defects in insulin delivery, changes in the expression of insulin-target proteins or genes, other metabolic defects, and interactions with other hormones (15). According to studies, it seems that insulin resistance takes precedence over disturbing secretion, and this phenomenon often occurs 10 to 20 years before the onset of symptoms of type 2 diabetes (16). Therefore, since evidence suggests that those with insulin resistance often have higher thyroid volume and risk of developing thyroid nodules, the possible relationship between type 2 diabetes and thyroid cancer has been shown in some previous studies (9, 17, 18).
2. Objectives
The objective of the present study was to investigate the global trend of thyroid cancer and its relationship with the prevalence of type 2 diabetes using the longitudinal model of random effects, to determine the risk of thyroid cancer due to diabetes.
3. Methods
The information in the present study is related to the prevalence of type 2 diabetes and the incidence of thyroid cancer which was extracted from the Global Burden of Disease (GBD) site during 1990-2019 in countries: Latin America, Australia, Caribbean, Central Asia, Central Europe, Central Latin America, Sub-Saharan Africa, East Asia, Southeast Asia, South Latin America, tropical Latin America, Western Europe, Sub-Saharan Africa, East Sub-Saharan Africa, South Asia, Oceania, North Africa, and the Middle East were the high-income parts of North America, Asia and the Pacific (19). In order to conduct this study, all the required information related to five continents and based on 204 different countries were extracted from the GBD site, which includes the incidence of thyroid cancer rate (per 100 thousand) during 1990 - 2019 and the prevalence of type 2 diabetes rate (per 100 thousand). All values of the studied indicators were calculated according to the world population, which is estimated by GBD and standardized in terms of age.
3.1. Statistical Analysis
The main objective of a longitudinal study is to determine the change in the response variable over time and the factors affecting the changes (20, 21). On the other hand, given that in longitudinal data, the assumption of independence of observations is violated, so for data analysis, it is necessary to use methods that can consider this correlation (22, 23).
In the random effect model for longitudinal data, it is assumed that there is a kind of normal heterogeneity among the subjects in the study population this heterogeneity between the subjects can be considered by considering the random effect in the model. In this case, it is possible to make individual predictions for the random effect model (21, 24, 25). For this purpose and to investigate the relationship between the prevalence of type 2 diabetes and the incidence of thyroid cancer, a random effect model was used. In this study, in order to accurately estimate the coefficients, a random effect model was used which randomly considered both the intercept and the slope. Here, the random effect of intercept was the initial thyroid cancer unique to each country and the random effect of the slope was the trend of unique changes in cancer incidence attributed to the prevalence of diabetes in each country.
The model used in the present study is as follows:
Where
In the present study, in order to determine the relationship between the incidence of thyroid cancer and the prevalence of type 2 diabetes using the random effects model, “nlme” package in R software was used.
This study was approved with the reference number of IR.SSU.SPH.REC.1399.090 by the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4. Results
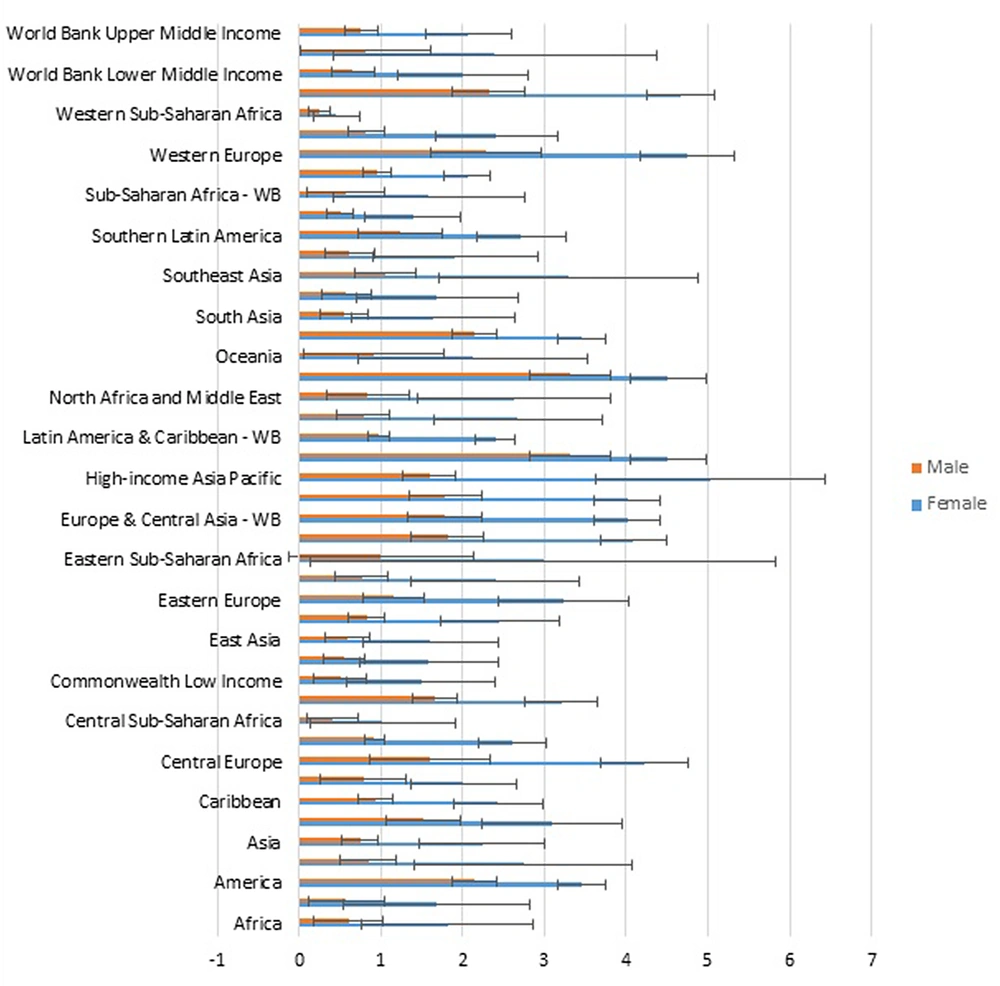
The incidence of thyroid cancer in 1990 was 1.90 per hundred thousand, while 2.79 in 2019. In 1990, the rate was 1.14 for men and 2.66 for women. This is while in 2019, this rate was equal to 1.83 hundred thousand for men and 3.74 for women.
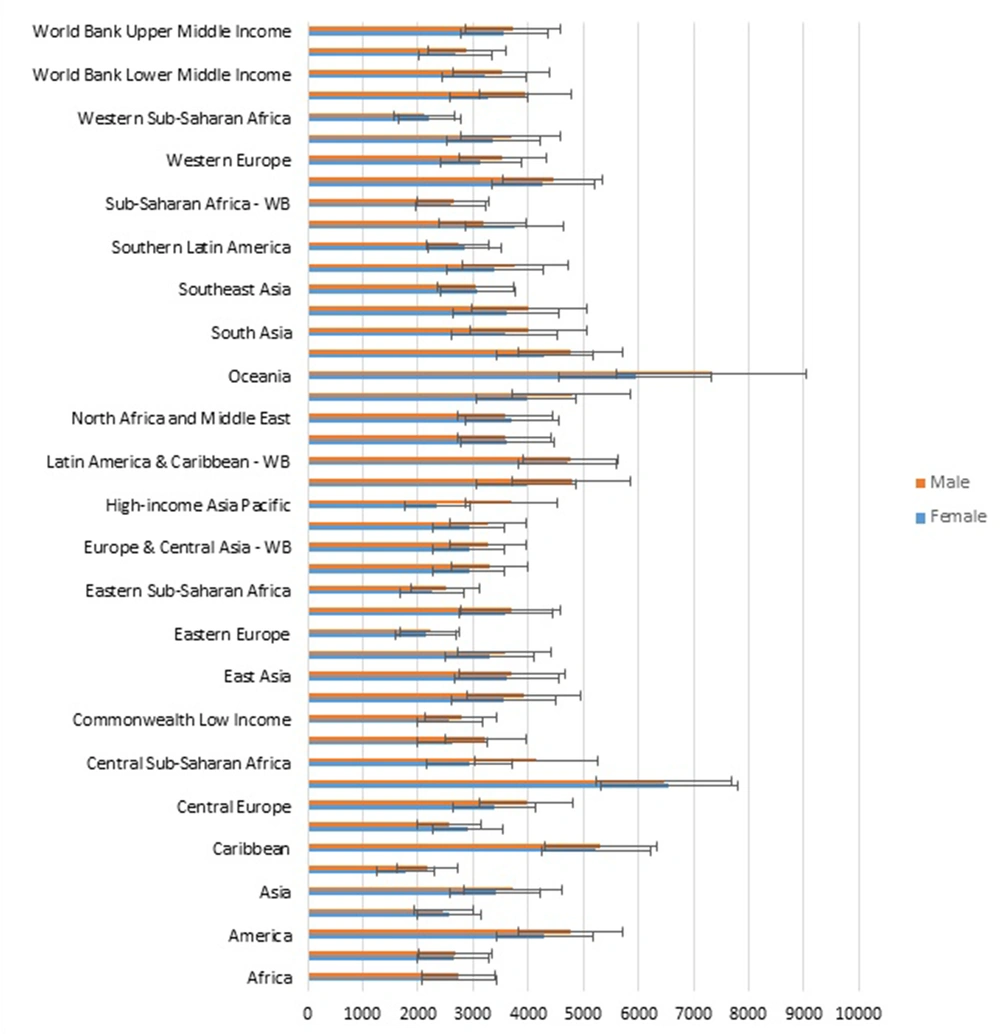
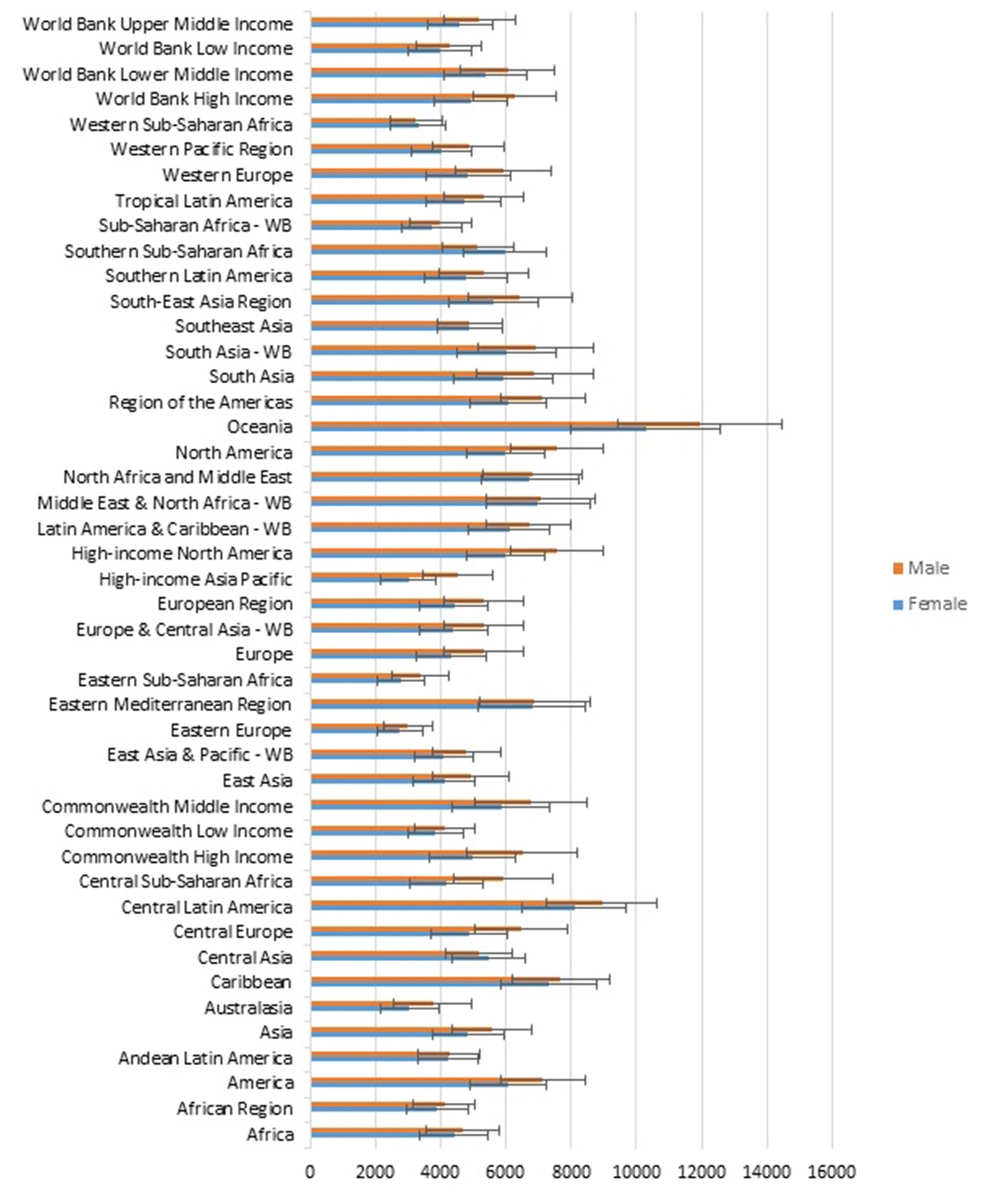
The prevalence of type 2 diabetes in 1990 was 3516.89 per hundred thousand, while 5420.68 in 2019. In 1990, the rate was 3661.29 for men and 3372.43 for women. This is while in 2019, this was equal to 5768.75 for men and 5072.60 for women.
The highest prevalence of type 2 diabetes in women in 1990 was in Oceania (7332.67) and Central Latin America (6452.09). The highest prevalence of type 2 diabetes in men was in Oceania (5940.64) and Central Latin America (6555.42) (Figure 1A).
The highest incidence of thyroid cancer in women in 1990 was in the high-income Asia Pacific and Western Europe (3.31%), while the highest incidence of thyroid cancer in men in 1990 was in high-income North America (5.03) and North America (4.75) (Figure 2A).
The highest incidence of thyroid cancer in 2019 was in the high-income Asia Pacific (7.21) and Eastern Europe (6.14), while the highest incidence of thyroid cancer in men 2019 was in high-income North America (4.99) and North America (4.9) (Figure 2B).
The highest prevalence of type 2 diabetes in women in 2019 was in Oceania (8101.6) and Central Latin America (10278.67). The highest prevalence of type 2 diabetes in men was in Oceania (8948) and Central Latin America (11934.53) (Figure 1B).
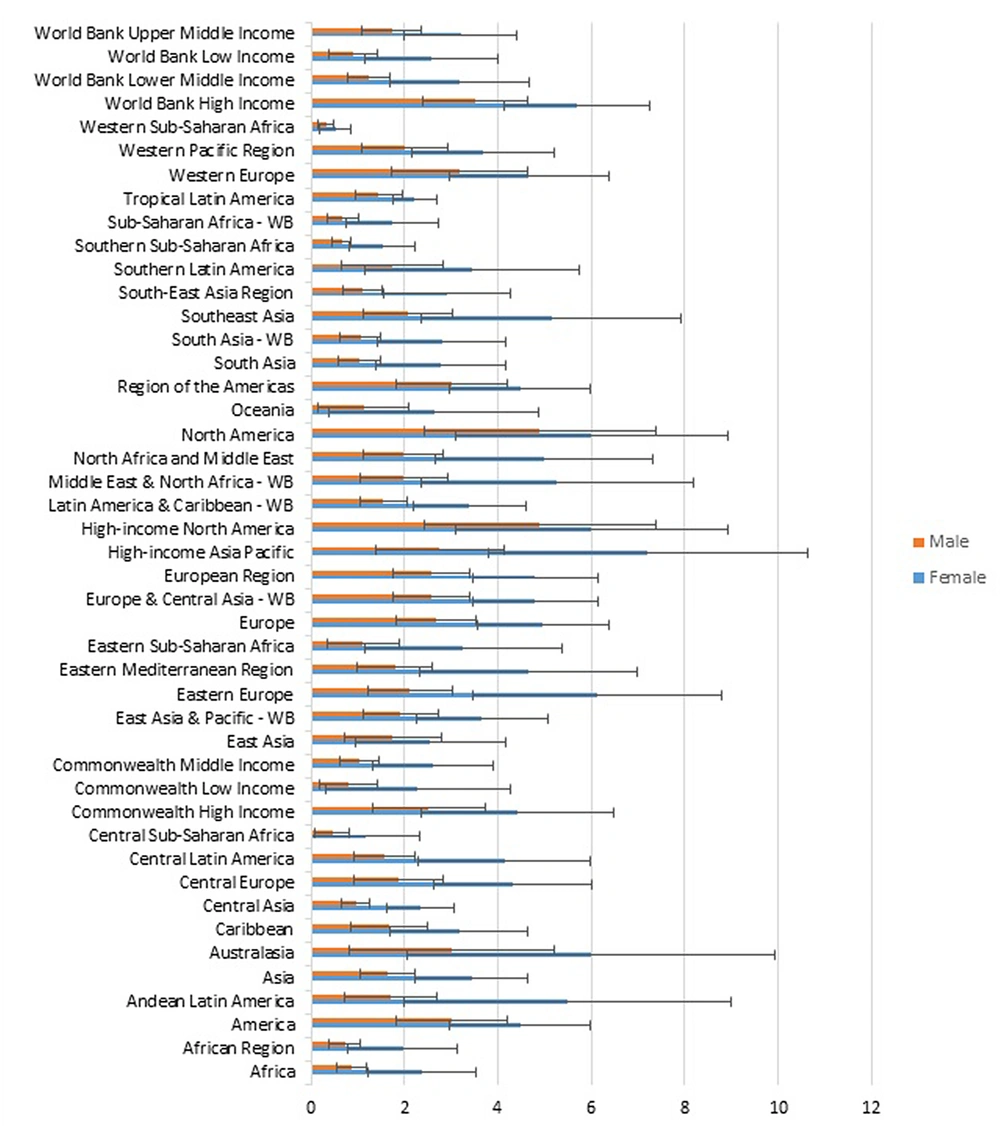
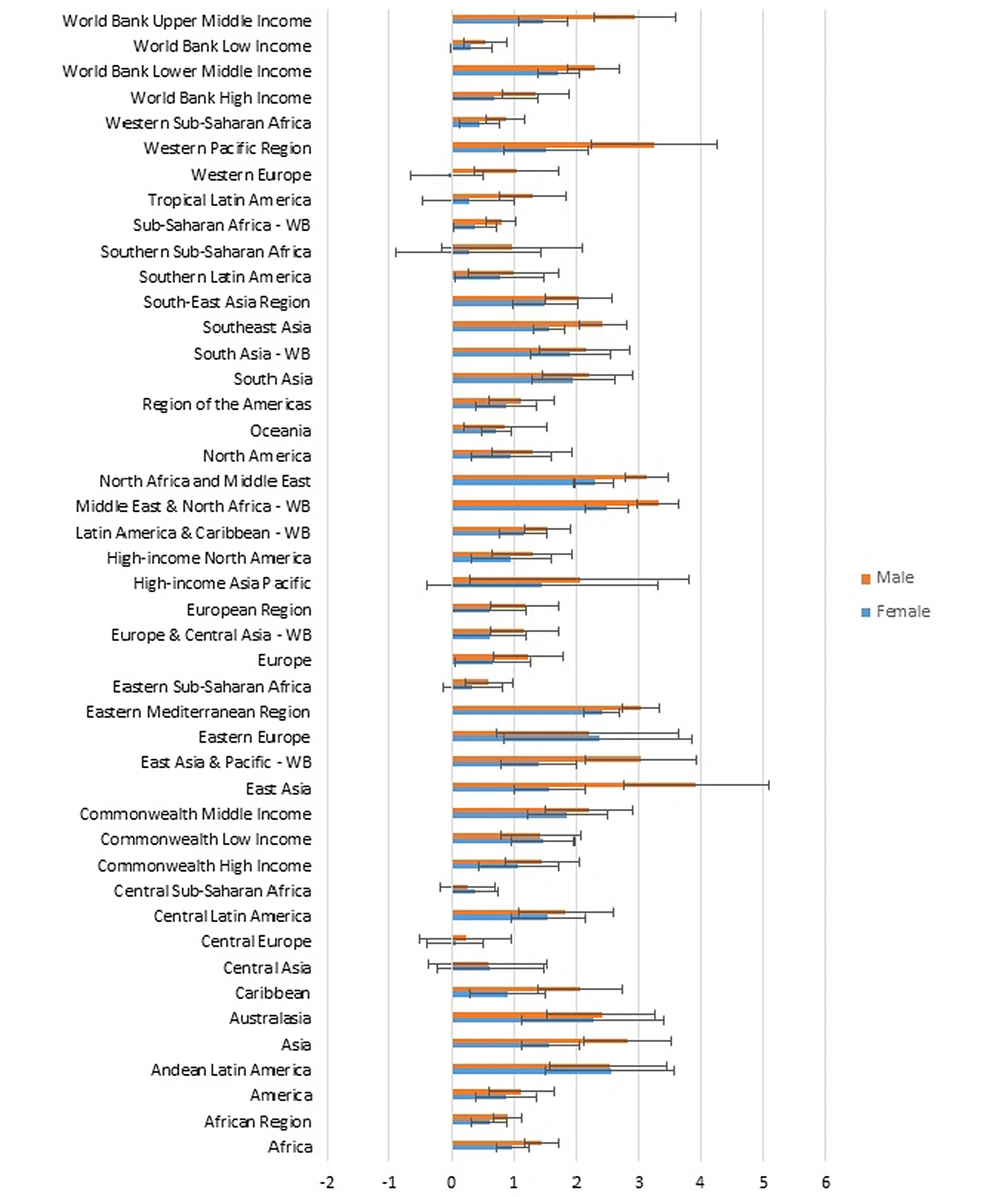
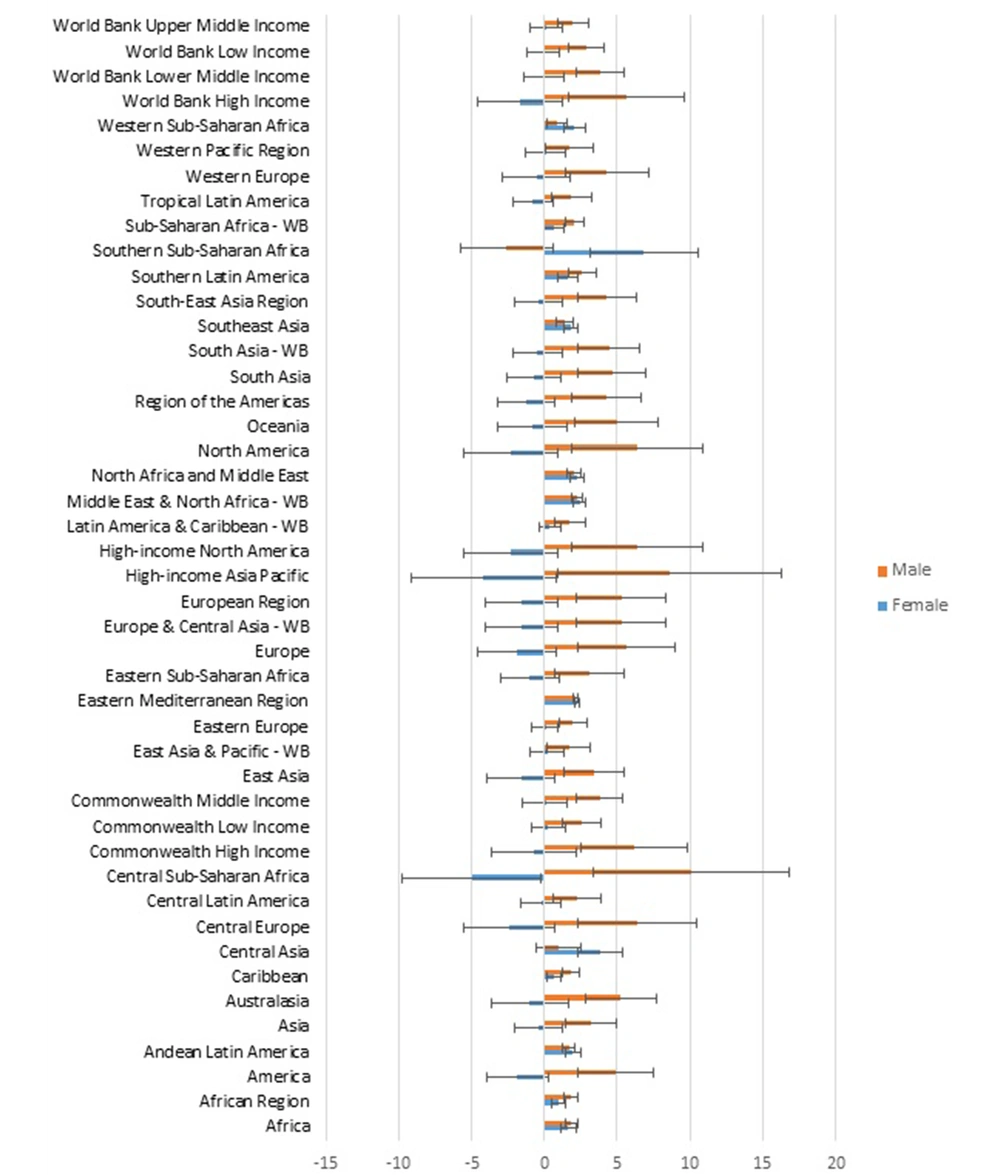
In general, East Asia (3.913) and the Middle East and North Africa (WB) (3.32) had the highest percentage of changes in the incidence of male thyroid cancer during 1990 - 2019. The highest percentage of these changes in women was related to Andean Latin America (2.544) and the Middle East and North Africa - WB (2.48) (Figure 3A).
In general, during 1990 - 2019, Central Sub-Saharan Africa (10.134) and high-income Asia Pacific (8.61) had the highest percentage changes in the incidence of type 2 diabetes in men. The highest percentage of these changes in women was related to Southern Sub-Saharan Africa (6.85) and Central Sub-Saharan Africa (4.99) (Figure 3B).
The results of the present study showed that the prevalence of type 2 diabetes had a significant effect on the incidence of thyroid cancer. Here, the relative risk is 0.00024 (95% CI 0.00023 - 0.00025). In other words, per unit increase in the incidence of type 2 diabetes, the risk of thyroid cancer increased by 0.00024. Therefore, 24 out of every 100,000 cases of thyroid cancer can be attributed to the prevalence of diabetes (Figures 4-6). This significance was also investigated separately in men and women and it was found that in both genders the prevalence of type 2 diabetes had a significant effect on the incidence of thyroid cancer, so that the risk in men was equal to 0.00018 (95% CI 0.00017 - 0.00019) and in women was equal to 0.00033 (95% CI 0.00031 - 0.00035) (Table 1).
| Parameter | Estimate | SE | %95 CI for Estimate | P-Value | |
|---|---|---|---|---|---|
| Male | |||||
| Intercept | 0.56 | 0.09 | (0.38 - 0.74) | < 0.001 | 0.82 |
| Type 2 diabetes | 0.00018 | 0.000004 | (0.00017 - 0.00019) | < 0.001 | 0.17 |
| -0.064 | |||||
| 0.10 | 0.0001 | (0.09 - 0.11) | |||
| Female | |||||
| Intercept | 1.67 | 0.14 | (1.38 - 1.96) | < 0.001 | 2.13 |
| Type 2 diabetes | 0.00033 | 0.00001 | (0.00031 - 0.00035) | < 0.001 | 0.99 |
| -0.042 | |||||
| 0.48 | 0.0001 | (0.45 - 0.49) | |||
| Total | |||||
| Intercept | 1.17 | 0.11 | (0.95 - 1.38) | < 0.001 | 1.17 |
| Type 2 diabetes | 0.00024 | 0.000006 | (0.00023 - 0.00025) | < 0.001 | 0.40 |
| -0.016 | |||||
| 0.22 | 0.0001 | (0.20 - 0.23) |
Parameters Estimation of Longitudinal Random Effects Regression Model to Investigate Thyroid Cancer Incidence and Its Relationship with the Prevalence of Type 2 Diabetes a
5. Discussion
The present study was an ecological study to investigate the relationship between thyroid cancer and the risk factor for type 2 diabetes. In this study, this relationship was investigated once in general and once by gender. For this purpose, the relative risk index obtained from the longitudinal random effects regression model was used. In our study, it was found that type 2 diabetes was significantly associated with thyroid cancer so that this relationship was statistically significant in both women and men. This significance was consistent with a study by Khoshsirat et al., they concluded that this was more significant in women (OR = 4.42, 95% CI: 2.04 - 9.57) (26). The results of our study are also consistent with the study results of Seo et al.. They concluded that type 2 diabetes had a significant effect on thyroid cancer (OR = 5.21, 95% CI: 1.58 - 17.15) (10). However, it should be noted that there are studies in which no significant relationship was between type 2 diabetes and thyroid cancer (27). What is certain is that the incidence of non-contagious diseases such as cancer and diabetes can vary around the world due to different ethnicities, environmental factors, and lifestyles. Therefore, it seems that the study results can be a good model for Asian countries, especially in West Asia or the Middle East.
On the other hand, it should be noted that many different factors can affect thyroid cancer. One of these factors is type 2 diabetes, which has been shown in several studies, including the present study, to be associated with thyroid cancer in both genders. In other words, according to the relative risk calculated in the present study, it can be said that the incidence of thyroid cancer in 24 out of every 100,000 people can be attributed to diabetes. On the other hand, in most studies where the relationship between thyroid cancer and type 2 diabetes was significant, this was more significant in women (28). In the present study, due to the higher relative risk in women than men, it can be claimed that type 2 diabetes has a greater effect on thyroid cancer in women than men.
It seems that insulin resistance takes precedence over impaired secretion, and this phenomenon often occurs 10 - 20 years before the onset of symptoms of type 2 diabetes (16). Patients with insulin resistance require more thyroid volume to form thyroid nodules. A study by Rezzonico et al. showed the highest thyroid nodules in the insulin-resistant group (61%) and the lowest (16.1%) in the insulin non-resistance group. The difference was also statistically significant (P < 0.001) (9). Therefore, it can be argued that high circulating insulin levels lead to increased thyroid proliferation. In other words, the thyroid gland is another victim of insulin resistance syndrome. In a study by Ayturk et al., a significant relationship was between thyroid and metabolic syndrome. The mean of thyroid in the group of metabolic syndrome with a mean of 17.5 and a standard deviation of 5.5 was significantly different from the mean in the control group with a mean of 12.2 and a standard deviation of 4.2 (11). In this article, it was concluded that metabolic syndrome significantly increased thyroid volume and the prevalence of nodules. In this study, it was found that insulin resistance is a risk factor for thyroid nodules (P = 0.005). In general, all these results are consistent with the results of the present study.
5.1. Conclusions
Our study showed that thyroid cancer can be associated with type 2 diabetes. In other words, type 2 diabetes can be a risk factor for thyroid cancer, so this effect can be considered in both men and women. On the other hand, considering the relative risk, it can be concluded that in addition to type 2 diabetes, there are other risk factors that have a significant effect on thyroid cancer. Therefore, type 2 diabetes can be considered a modified risk factor in the screening of cancer patients with diabetes, especially women.