1. Introduction
Mature cystic teratomas are benign germ cell tumors found predominately in the gonads and rarely in extra-gonadal areas (1). Intrapulmonary mature cystic teratomas are extremely rare and the first case was reported by Mohr in 1839 (2). Intrapulmonary mature cystic teratomas arise from totipotent cells of 1 or more of the 3 germ layers, which can differentiate into any type of tissue (3). These lesions usually involve the upper lobes of the left lung and usually present with nonspecific symptoms such as chest pain, persistent cough, and hemoptysis (4). There are no specific clinical or radiological findings for diagnosis, and anatomopathological examination is the definitive diagnostic method (5). To the best of our knowledge, no case has yet been reported from Kabul, Afghanistan. We describe here the first case of intrapulmonary mature cystic teratoma reported from Kabul, Afghanistan, to draw the attention of clinicians to this pathology.
2. Case Presentation
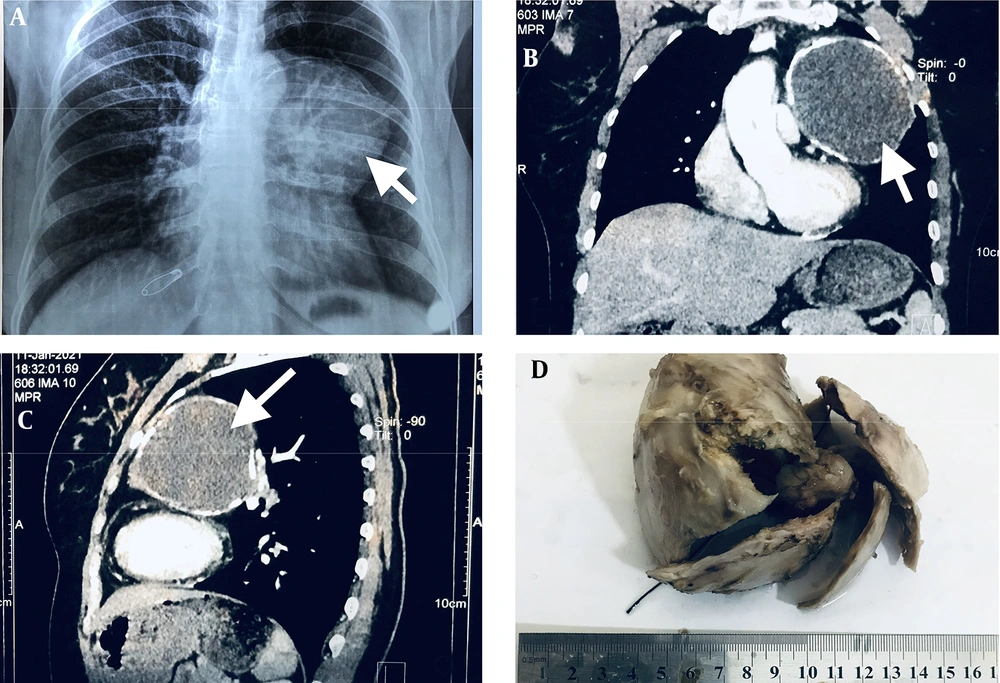
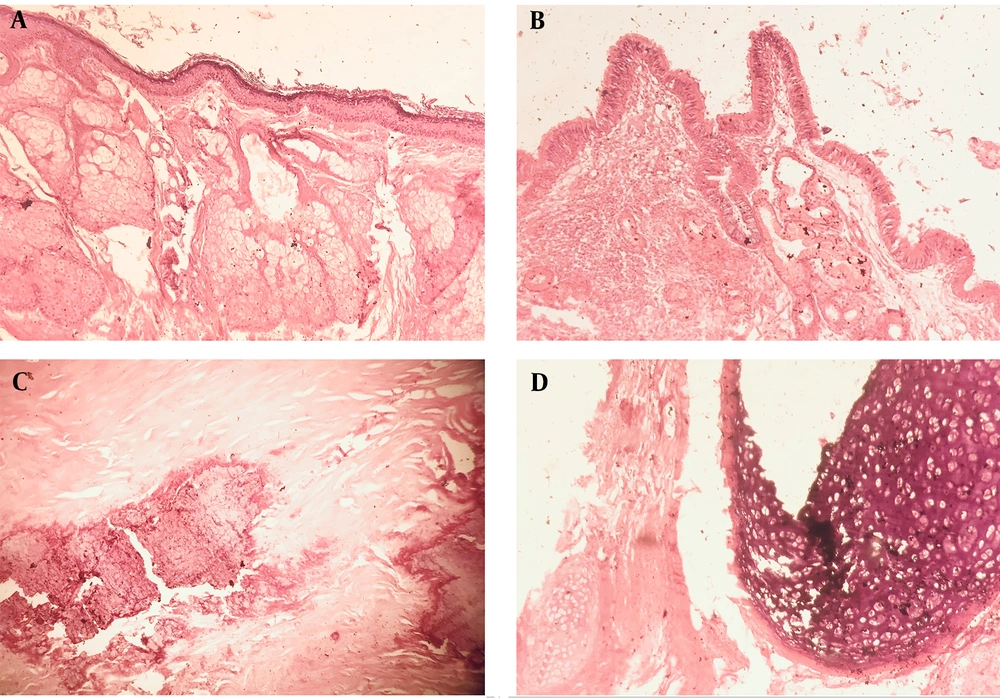
A 28-year-old Afghan woman presented to her local hospital complaining of a 6-month history of intermittent episodes of dry cough and hemoptysis. Her medical history was unremarkable. Clinical examination revealed a well-preserved young woman with stable vital signs. Auscultation of the chest revealed coarse crackles in the left upper lobe. The rest of the clinical examination was within normal limits. Chest X-ray showed a well-demarcated large opacity in the left upper lobe of the lung (Figure 1A). Computed tomography (CT) of the chest showed a well-demarcated cystic lesion measuring 9.5 × 8.0 × 7.0 cm, occupying the anterior segment of the left upper lobe (Figure 1B and C). The lesion had a homogeneous density and contained soft tissues, fat, and calcifications at the periphery. No mediastinal lymphadenopathy, pleural effusion, or thickening was observed. Routine hematologic testing and abdominal ultrasonography were unremarkable. The clinicians suggested a diagnosis of lung abscess and recommended that the patient take broad-spectrum antibiotics; they also recommended lifestyle changes of no smoking and drinking more fluids. After 6 weeks of treatment, there was no positive change in the patient's condition and the lesion had not disappeared on the chest X-ray. Therefore, surgical intervention was suggested to remove the lesion. Vital signs were within normal limits and the patient underwent surgery under general anesthesia. A posterolateral thoracotomy was performed. Examination of the pleural cavity revealed a grayish intrapulmonary cystic mass (9.0 × 7.5 × 6.0 cm) in the left upper lobe filled with cheesy material, and a cystectomy was performed. The specimen was sent to the Pathology Department of Kabul University of Medical Sciences for further examination. The cystic lesion had a size of 9.0 × 7.5 × 6.0 cm. The sections of the lesion showed a unilocular cystic lesion filled with waxy material (Figure 1D). A granular sensation was felt when cutting the cyst wall. Microscopic examination revealed a diversity of cell lines (Figure 2), consisting of squamous epithelium with underlying sweat and sebaceous glands (Figure 2A), pseudostratified ciliated columnar epithelium with underlying seromucous glands (Figure 2B), areas of calcification (Figure 2C), and cartilaginous tissue (Figure 2D). The final diagnosis of intrapulmonary mature cystic teratoma was made by histopathologic examination.
Chest X-ray shows a well-demarcated large opacity in the upper lobe of the left lung (A). Computed tomography (CT) of the chest shows a well-demarcated lesion in the anterior segment of the left upper lobe with peripheral calcification (B, C). Surgical specimen representing encapsulated unilocular cystic lesion and waxy material already removed (D).
3. Discussion
Mature cystic teratomas grow slowly and are usually benign. Intrapulmonary mature cystic teratomas are very rare neoplasms. To date, fewer than 100 cases have been described in the medical literature, with the first report dating back to 1839 (2, 6). Most cases are localized in the left upper lobe (7), as in the reported case; they usually affect patients in their first and second decades of life and occur equally in men and women. Symptoms of intrapulmonary mature cystic teratomas vary depending on the location, size of the tumor, and histological components. In this case, the patient complained of dry cough and hemoptysis, the most commonly reported symptoms. Other symptoms reported in the literature include trichophytic, pneumonia, fever, bronchiectasis, abscesses, and infection (8). The size of the neoplasm is not related to malignancy (7, 8). Reports of various studies have shown that laboratory tests are generally unremarkable (9, 10), which is concordant with our case. Radiographic findings in most cases show cystic lesions, often with focal calcification (11), but in some cases, chest radiography may be of no diagnostic value, particularly when tissues such as bone and teeth are absent. Chest CT is considered a standard diagnostic procedure because it provides information about the exact location, extent, and nature of the lesion; however, it can also provide non-specific findings (9). Studies have shown that a lobulated cystic lesion with peripheral translucency is distinctive for the diagnosis of teratoma on CT, as in our case, though having such specific features as peripheral calcification or translucency; our clinicians missed the differential diagnosis of teratoma, which is due to the lack of information and rarity of the lesion. The commonly mentioned preoperative differential diagnoses are lung abscess and hydatid cyst (8). In our case, the preoperative chest X-ray and CT scan resulted in the misdiagnosis of a lung abscess, after which the patient was treated with a broad-spectrum antibiotic. The recommended treatment is complete resection of the tumor, after which the patient is considered completely cured (6, 12). Patients who have not undergone surgery may experience excessive hemoptysis, tumor enlargement, airway compression, malignant transformation, and ultimately death (4, 10). In the reported case, the patient was without complications and did not require further therapeutic measures as reported in the literature. Postoperative histopathologic examination gave the exact diagnosis, where squamous epithelium with plentiful keratin, connective tissue, parts of fat tissue, calcifications, for example, teeth or bone, drifting hair and endometrial tissue were noticed (11, 13). Similar features were also noted in this case.
3.1. Conclusions
Intrapulmonary mature cystic teratoma is a rare neoplasm and surgery is considered the optimal treatment. It is usually misdiagnosed preoperatively due to nonspecific clinical symptoms, and indistinguishable radiographic findings, and should keep in the differential diagnosis of all cystic lesions. The exact diagnosis is made by postoperative anatomopathological examination.