1. Introduction
Spinal cord intramedullary tumors are rare and account for 20% of adults and 35% of pediatric spinal tumors. Astrocytomas and ependymomas are the most common histological types of intramedullary tumors (1). As the most common intramedullary spinal cord neoplasm in adults, spinal cord intramedullary ependymomas (IE) originate from ependymal cells that line the ventricular system and spinal canal. They account for approximately 3 - 6% of central nervous system tumors and 60% of intramedullary tumors (2). The majority of spinal cord ependymomas (25 - 42% of the cases) occur in the cervical region, and most of them are non-capsulated, benign, have little infiltrative potential, and have a slow rate of growth (3). Before diagnosis, they cause prolonged symptoms, with an average of two years. Symptoms are related to the tumor's location and can present with pain, motor weakness of extremities, hypoesthesia, gait disturbance, sphincter, or sexual dysfunction (4). Considering the non-specific nature of its presentation, it is imperative to conduct imaging modalities as early as possible. The use of imaging also aids in the determination of tumor size, compression of structures, and other important aspects apart from diagnosis (5).
IEs are classified into three types. Grade I, tumors include myxopapillary and subependymoma, which do not infiltrate the peripheral tissue, and surgical excision is sufficient to be cured. Grade II, tumors have papillary, clear cell, and tanycytic cells that tend to recur after resection and can transform into malignant types more frequently than grade I tumors. Grade III tumors are anaplastic ependymomas that infiltrate adjacent tissue, and surgical resection does not cure them (4).
The gold standard treatment choice for IE tumors is gross-total surgical resection (6). Postoperative radiotherapy for residual tumors may be needed as surgical resection leads to complete resection because of tumor location. Still, the role of this adjuvant therapy remains unclear and is related to the extent of tumor resection. Radiotherapy decreases failure rate, enhances neurologic function, and Increases survival rate (7). Radiation therapy should be applied to those with anaplastic-type or residual mass after the operation (8).
2. Case Presentation
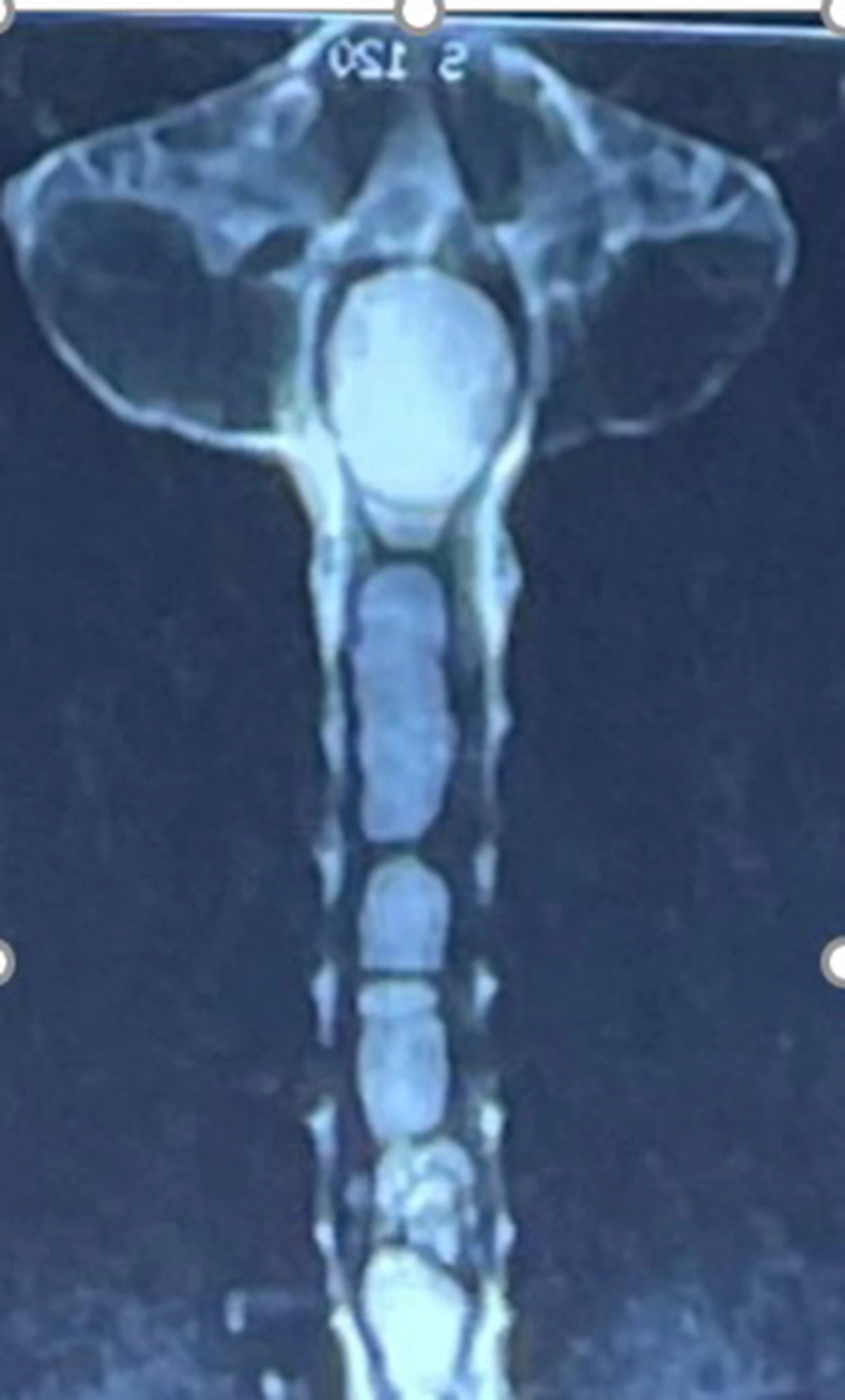
A 42-year-old man presented to our institution with the chief complaint of neck pain with radiation to both shoulders, paraesthesia of upper extremities, gait disturbance, and dysphagia. The symptoms were initiated four years ago and, in the evaluations, IE was diagnosed. Still, the patient refused the surgical treatment due to the location, tumor extension, and surgery complications (Figure 1). In the months before presenting, the patient started to have difficulty swallowing. The symptoms are considered tumoral pressure in the fourth ventricle.
2.1. Surgical Method
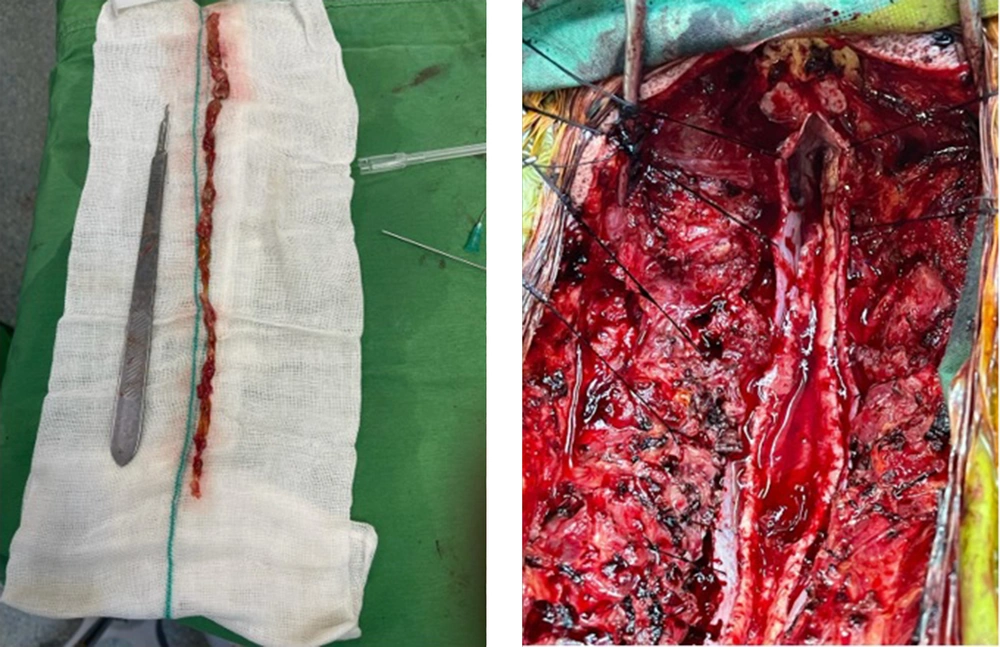
After general anesthesia in the prone position, the patient underwent laminectomy from T4 to C1 and partial resection of the occipital bone. The dura was incised carefully, and under the microscope, a careful midline myelotomy was done by separating posterior columns (Figure 2). The typical reddish-Gray tumor was located from the fourth thoracic vertebra to the fourth ventricle. The tumor gently separated from the spinal cord and was extracted entirely (Figure 3). No instrumentation was done. Dura was closed with running- locked sutures, and fascia and skin were tightly closed over two drains. Figure 4 demonstrates the pathology of the tumor.
Immediately After the surgery, the patient's symptoms resolved except for right-hand paraesthesia. The physiotherapy began after two weeks after surgery for the right hand. Informed consent was taken from the patient.
3. Discussion
Intramedullary spinal cord ependymomas (IE) are non-capsulated, benign, and slow-growing tumors. The cervical region is the most common intramedullary tumor and the most frequent site of IE despite its lesser spinal cord tissue. It usually occurs in middle-aged adults with identical sex distribution. IEs present with a variety of symptoms, and the most common of them is pain. Usually, patients experience a prolonged period before the diagnosis occurs. Clinical presentations are related to the site of the tumor and include pain, motor weakness, sensory problems, gait disturbance, sphincter, or sexual dysfunction (9).
The treatment of IEs is surgical resection and is recommended to be performed as soon as the diagnosis is made, regardless of its extension (9). Surgical resection is usually sufficient, and no subsequent intervention is needed. The tumor recurrence is rare since the prognosis after complete resection is favorable (10). The surgical resection was previously conducted in two stages suggested by Cushing (11) and Horrax and Henderson (12) which de Divitiis et al. (13) and Zhang et al. (14) demonstrated that single-stage laminectomy is preferred over the old two-stage operation.
Peker et al. demonstrated that a ratio of the tumor width to the largest cord width at the tumor site could play a role as an indicator of neurological outcome after surgery. When it is more than 0.80, the prognosis is poor. They also showed that the length of the tumor could predict the risk of postoperative dysesthesia. Therefore, the risk is higher in long IEs (15). The most substantial factor predicting the surgery's functional outcome was the preoperative neurological condition (16). McCormick scores less than 3 (Table 1) and extension of tumor less than five levels are assumed as the most critical factor for an excellent postoperative functional outcome (17).
| Grade | Clinical Definition |
|---|---|
| 0 | No deficit |
| 1 | Mild motor or sensory deficit, functional independent |
| 2 | Moderate deficit, limitation of function, independent without external aid |
| 3 | Severe motor or sensory deficit, limited function, dependent on external aid |
| 4 | Severe deficit, paraplegia or quadriplegia |
It is recommended that after the surgery, patients should be monitored with physical examination and MRI at regular intervals for at least ten years (18).
In this case, we presented a massive intramedullary ependymoma of the spinal cord, with four years of progressive upper extremities paraesthesia, gait disturbance, and dysphagia. IEs usually present with progressive upper extremity paraesthesia, gait disturbance, and dysphagia caused by compression of the spinal cord.
Usually, a tumor in the cervical region extends for eight segments. Still, in our patient, the tumor extends from the fourth ventricle to the fourth thoracic vertebra, a rare presentation. We recommend that patients undergo surgery as soon as the diagnosis is made because, as is evident in this case, the tumor can progress and cause permanent symptoms. Our patient was fortunate to be treated entirely without any subsequent complications and symptoms.
Massive spinal ependymoma is a rare, benign, slow-growing tumor, and patients develop symptoms years before diagnosis. Due to its non-specific presentations and the possibility of progression of the symptoms, we recommend surgery as soon as the diagnosis is confirmed.