1. Background
Bladder cancer is one of the most common cancers worldwide, especially in men that and in spite of all treatments, the mortality rate has remained high (1). According to the Global Burden of Disease report, there were 524,000 new bladder cancer cases and 229,000 bladder cancer deaths worldwide in 2019. The age-standard incidence rates (ASIRs) of bladder cancer were reported 1.4 - 31.9 per 100,000 population in different parts of the world. Monaco had the highest ASIRs in the world (31.9 per 100 000) followed by Lebanon (30.2 per 100,000) and San Marino (25.3 per 100,000) (2).
In Iran, bladder cancer is considered the most frequent urologic cancer in men and women (3). Different studies have evaluated the incidence rate of bladder cancer in Iran; ASIRs of bladder cancer varied from 2.1 to 17.7 per 100,000 in men (4, 5) and 0.4 to 4.1 per 100,000 in women (6, 7) in different provinces and different years. A recent systematic review and meta-analysis showed that the ASIRs of male and female bladder cancer are 10.92 and 2.80 per 100,000, respectively in Iran (8).
Incidence and mortality rates of bladder cancer vary globally and this may be due to genetic differences, population age, and exposure to risk factors i.e. smoking habits. The main histologic subtype of bladder cancer is urothelial carcinoma which includes more than 90% of all bladder cancers (9). Regardless of disease stage, bladder cancer is associated with high morbidity. Bladder cancer is non-muscle invasive in 70% to 80% of patients; however, the likelihood of recurrence is high in non-muscle invasive diseases and almost all patients require regular and life-long follow-up which imposes a remarkable financial burden on healthcare systems (10).
A thorough understanding of bladder cancer epidemiology is of great value for policymakers and assists in the prevention and early detection of the disease, especially in regions with high incidence or mortality rates. Epidemiological studies also may provide important information for studies that assess risk factors for cancer.
2. Objectives
In the present study, we aimed at reporting national and subnational incidence trends of bladder cancer in Iran between 2003 and 2015.
3. Methods
This descriptive-analytical study carried out on national and subnational data of pathology-confirmed cases of recorded bladder cancer that were by the Iranian National Cancer Registry of the Iran Ministry of Health and Medical Education has been developed systemically since 2000 using software-based data from all pathology centers with coverage of 100% of country provinces (11, 12). Since 2014, it has been developed by collecting clinical, paraclinical, and mortality data nationwide (13). In the Iranian cancer registry system, cancer types are coded according to the International Classification of Diseases for Oncology, third edition (ICD-O-3) (14), and the topography of cancers is determined based on the International Classification of Diseases, 10th edition (ICD-10) (15). In this system, bladder cancer is detectable by C67, the malignant neoplasm of the bladder (15). Statistics of new bladder cancer cases by each year and in each province were provided by recorded data from the National Cancer Management Secretariat of the Ministry of Health and Medical Education (16). In this study, the results were calculated and reported for the entire country and provinces based on the number of cases and ASIRs per 100,000 people per annum (in 18 age groups) for both sexes and by year and province. In this regard, the country’s population by men and women, as well as the population of the provinces, were obtained from the portal of the Iran Statistics Center. This center performs and reports the Iran population census every 5 years (17). Due to the unavailability of any population estimation in the interval between periods, the population of the nearest year was used for calculating Incidence rates.
Incidence rates were calculated directly and based on the standard population of the World Health Organization (WHO) using STATA software version 12. To simplify assessments of age-specific epidemiological rates through populations with diverse age structures, it is beneficial to determine short statistics which take away the effects of variation in age composition. For keeping the comparability of the incidence rates in different societies, WHO has introduced a new standard population as a basis to facilitate epidemiological research worldwide (18).
Due to the severe lack of data recording during the years 2010 to 2013, the available data did not have the necessary citation capability, so we decided to compensate for this shortcoming by performing a time series analysis for this period in support of a more precise presentation of national incidence trends.
For identifying a proper primary model sc and pac graphs were used. The comparison was done using the Likelihood ratio test (Lrtest). The autoregressive integrated moving average (ARIMA) model was used as the most common category of models for forecasting time series events (19). ARIMA (pdq) consists of components of autoregressive (p), the difference (d), and moving average (q) and in the case of having a seasonal pattern for a disease, are used as SARIMA (p d q) (P D Q) s. in this condition P, D, and Q components are same as the aforementioned model and s is the time corresponding to a data in the previous year.
4. Results
The number of incident bladder cancer cases in Iran was 39352 between 2003 and 2015 including 7044 (17.9%) women and 32308 (82.1%) men. The age-standardized incidence rate of bladder cancer in 2015 was 13.57 in men and 2.86 in women.
The numbers of incident cases, annual crude incidence rate, and ASIR for both sexes from 2003 to 2015 are demonstrated in Table 1. The age-specific incidence rate among men had a rising trend from 8.35 per 100,000 in 2003 to 13.57 in 2015. The incidence trend of bladder cancer in women also increased over the study period. The lowest women-adjusted incidence rate was 2.12 per 100,000 in 2003 and the highest was 3.78 per 100,000 in 2008.
| Year and Gender | Number of Cases | Crude Incidence Rate | ASIR |
|---|---|---|---|
| 2003 | |||
| Male | 2263 | 6.63 | 8.35 |
| Female | 482 | 1.49 | 2.12 |
| 2004 | |||
| Male | 2722 | 7.84 | 9.90 |
| Female | 579 | 1.76 | 2.49 |
| 2005 | |||
| Male | 3248 | 8.99 | 11.30 |
| Female | 689 | 2.01 | 2.86 |
| 2006 | |||
| Male | 3347 | 9.30 | 11.66 |
| Female | 705 | 2.06 | 2.99 |
| 2007 | |||
| Male | 3617 | 10.05 | 13.03 |
| Female | 781 | 2.29 | 3.32 |
| 2008 | |||
| Male | 3957 | 10.99 | 14.42 |
| Female | 883 | 2.58 | 3.78 |
| 2009 | |||
| Male | 3764 | 9.57 | 12.59 |
| Female | 837 | 2.44 | 3.28 |
| 2010 a | |||
| Male | 3780 | 9.97 | 12.89 |
| Female | 859 | 2.30 | 2.70 |
| 2011 a | |||
| Male | 3565 | 9.40 | 11.81 |
| Female | 768 | 2.06 | 2.71 |
| 2012 a | |||
| Male | 3606 | 9.40 | 12.01 |
| Female | 689 | 1.82 | 2.14 |
| 2013 a | |||
| Male | 3604 | 9.29 | 11.76 |
| Female | 645 | 1,69 | 2.17 |
| 2014 | |||
| Male | 4776 | 12.37 | 14.30 |
| Female | 1041 | 2.47 | 2.97 |
| 2015 | |||
| Male | 4615 | 11.82 | 13.57 |
| Female | 1047 | 2.72 | 2.86 |
Abbreviations: ASIR, age-standardized incidence rate.
a Results are provided by time series model
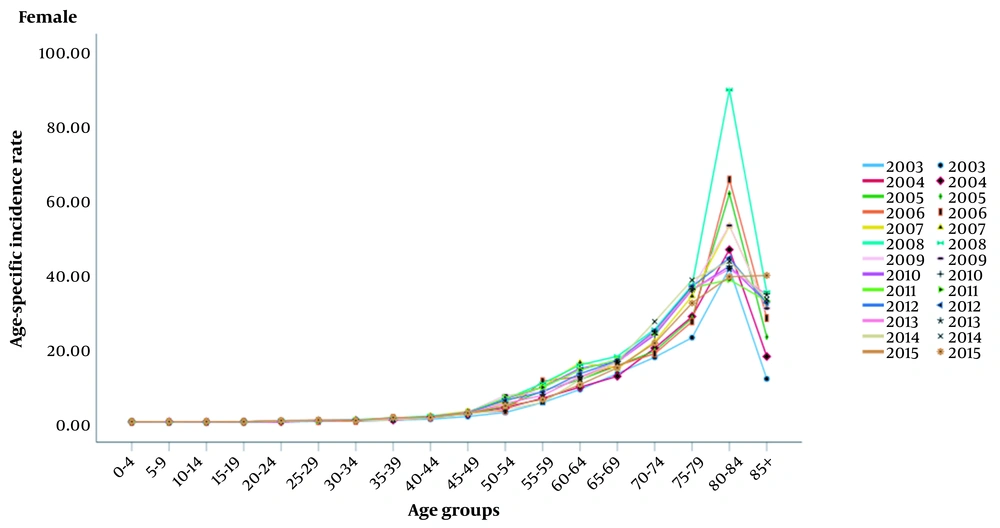
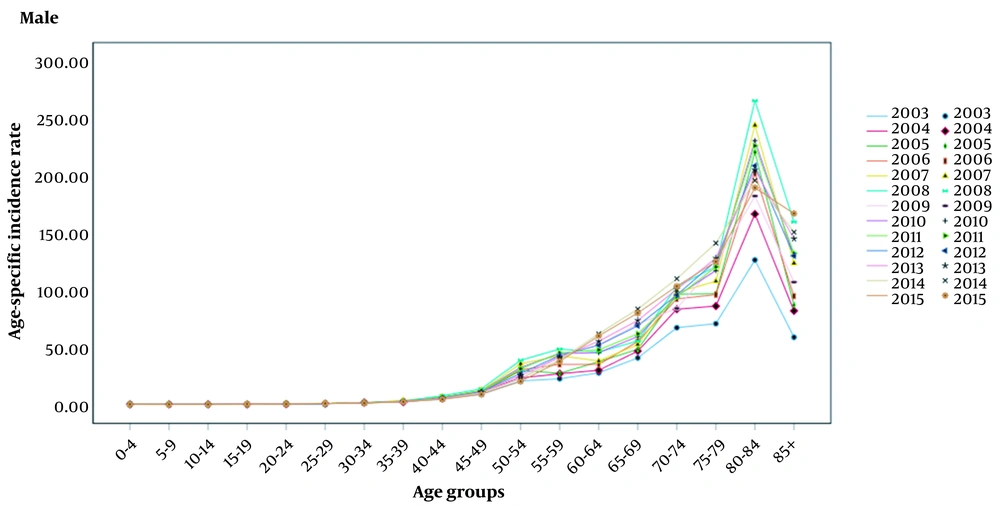
The incidence rate of bladder cancer increased with age in both sexes and the highest ASIR of bladder cancer was observed in the age group of 80 to 84 years (Figures 1 and 2).
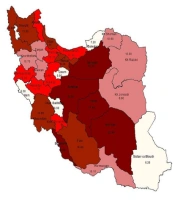
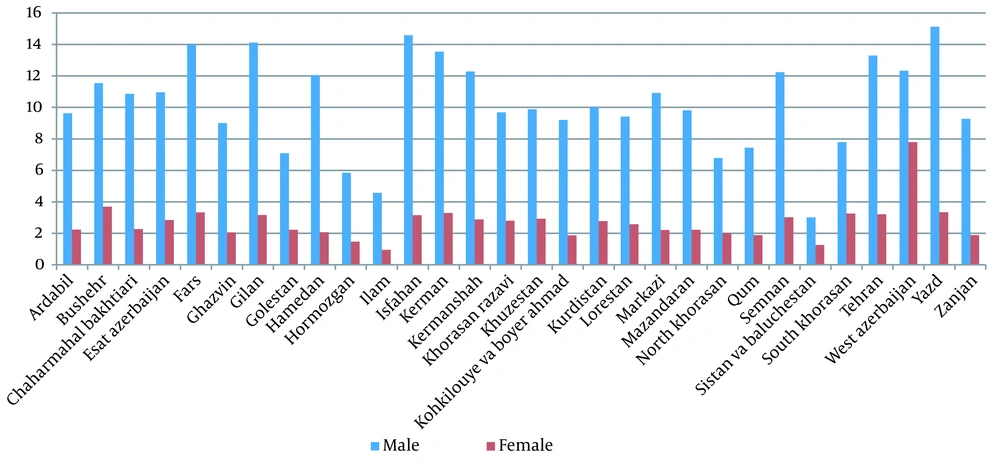
The highest ASIR of male bladder cancer was related to Yazd (15.13 per 100,000) followed by Isfahan (14.59 per 100,000), Gilan (14.12 per 100,000), and Fars (14.00 per 100,000) whereas the lowest one was related to Sistan va Baluchestan and Ilam (3.01 and 4.58 per 100,000, respectively). In women, the highest ASIR was related to West Azerbaijan (7.79 per 100000) followed by Bushehr (3.69 per 100000), Fars (3.33 per 100000), and Kerman (3.30 per 100000). Also, our result showed that the lowest ASIR of female bladder cancer was related to Ilam, Sistan va Baluchestan and Hormozgan (0.96, 1.26 and 1.48 per 100000, respectively).
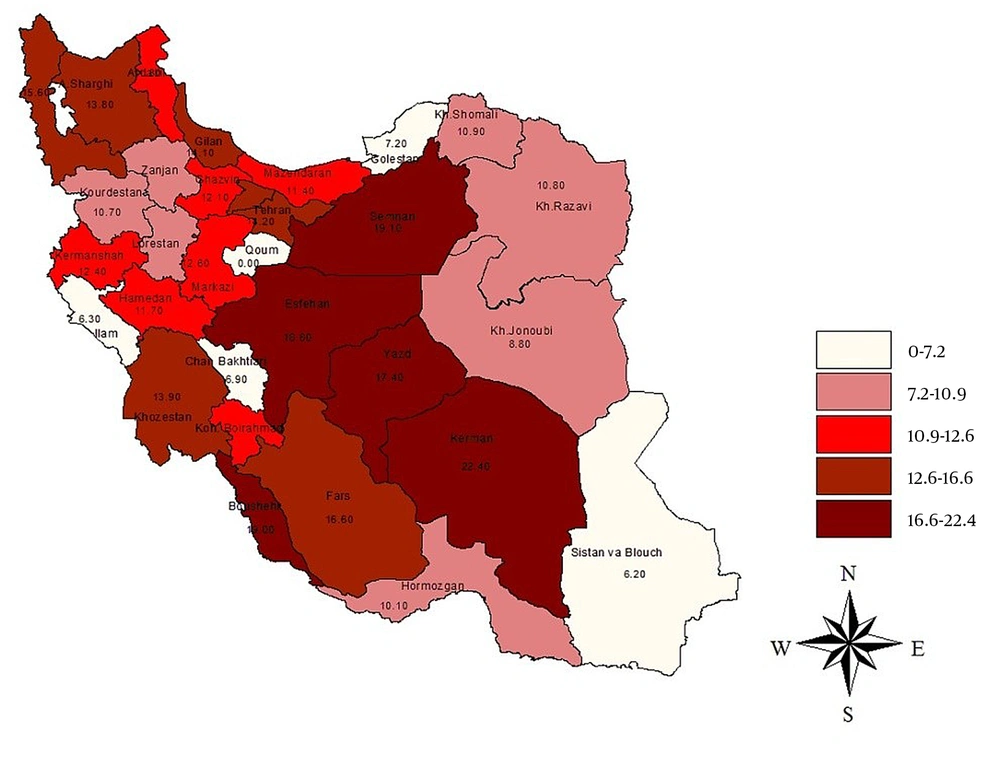
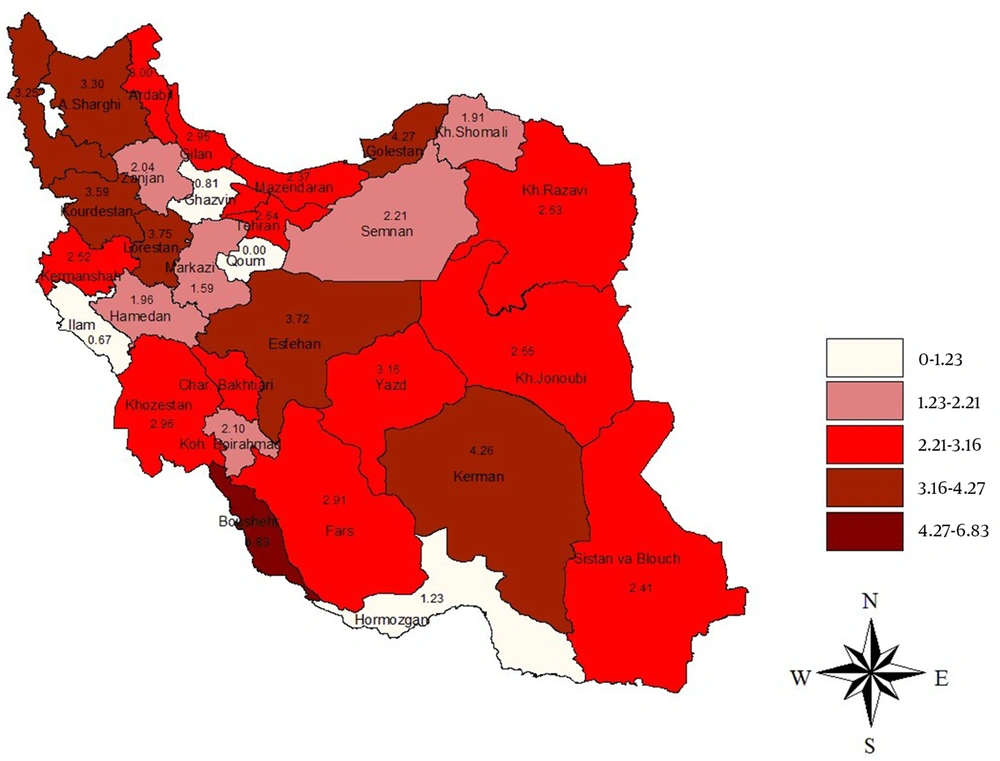
During the years of study, the highest peaks of women’s bladder cancer incidence rate occurred in Bushehr (6.19 per 100,000 in 2014), East Azerbaijan (6.19 per 100,000 in 2008), and Khuzestan (5.17 per 100,000 in 2008). Moreover, Kerman (27.3 per 100,000 in 2014 and 22.4 per 100,000 in 2015), Tehran (21.24 per 100,000 in 2008), as well as Gilan (20.12 per 100,000 in 2008) had the highest incidence rates of men’s bladder cancer in Iran (Table 2 and Figure 3). Analyzing the geographical distribution of new bladder cancer cases indicated that Bushehr province presented the highest ASIR in females in 2015 (6.83 per 100,000), while the highest ASIR in males in the same year was observed in Kerman province (22.40 per 100,000) (Figures 4 and 5).
| Province and Sex | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 a | 2011 a | 2012 a | 2013 a | 2014 | 2015 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ardabil | ||||||||||||||
| Male | 8.44 | 10.56 | 6.32 | 11.66 | 7.45 | 9.92 | 9.92 | 9.1 | 9.65 | 9.55 | 9.93 | 10.60 | 11.80 | 9.63 |
| Female | 1.81 | 1.90 | 1.79 | 2.99 | 1.02 | 3.22 | 2.15 | 2.13 | 2.5 | 2.26 | 2.36 | 2.33 | 3.00 | 2.249 |
| Bushehr | ||||||||||||||
| Male | 5.88 | 7.51 | 8.20 | 9.70 | 7.44 | 11.57 | 16.06 | 11.69 | 13.11 | 13.62 | 15.08 | 18.50 | 19.00 | 11.54 |
| Female | 2.73 | 2.52 | 2.30 | 2.67 | 4.50 | 3.28 | 3.56 | 3.78 | 3.54 | 3.63 | 3.99 | 4.80 | 6.83 | 3.69 |
| Chaharmahal Bakhtiari | ||||||||||||||
| Male | 4.54 | 7.89 | 8.65 | 11.35 | 15.67 | 16.04 | 11.76 | 14.49 | 14.1 | 13.45 | 14.15 | 14.90 | 6.90 | 10.86 |
| Female | 0.36 | 3.99 | 1.91 | 1.90 | 2.70 | 3.20 | 1.38 | 2.43 | 2.34 | 2.05 | 2.33 | 2.60 | 2.37 | 2.27 |
| East Azerbaijan | ||||||||||||||
| Male | 2.46 | 11.2 | 2.95 | 3.00 | 15.75 | 19.64 | 15.92 | 17.1 | 17.55 | 16.86 | 16.07 | 13.80 | 13.8 | 10.95 |
| Female | 0.35 | 1.75 | 0.85 | 0.65 | 4.88 | 6.19 | 4.46 | 5.18 | 5.28 | 4.97 | 4.49 | 3.22 | 3.30 | 2.85 |
| Fars | ||||||||||||||
| Male | 10.85 | 10.45 | 13.49 | 11.62 | 17.89 | 13.70 | 15.68 | 15.76 | 15.05 | 15.49 | 15.41 | 15.70 | 16.6 | 14.00 |
| Female | 2.68 | 2.42 | 2.49 | 2.98 | 4.45 | 3.70 | 4.96 | 4.37 | 4.34 | 4.56 | 4.11 | 3.42 | 2.91 | 3.33 |
| Ghazvin | ||||||||||||||
| Male | 6.36 | 5.99 | 7.83 | 7.17 | 10.32 | 10.72 | 7.21 | 9.42 | 9.12 | 8.58 | 10.37 | 13.40 | 12.10 | 9.01 |
| Female | 1.55 | 1.67 | 2.13 | 1.46 | 3.18 | 2.79 | 1.78 | 2.58 | 2.38 | 2.25 | 2.61 | 3.19 | 0.81 | 2.062 |
| Gilan | ||||||||||||||
| Male | 7.67 | 11.52 | 13.82 | 14.51 | 15.93 | 20.12 | 16.55 | 17.53 | 18.07 | 17.38 | 16.12 | 12.90 | 14.10 | 14.12 |
| Female | 1.47 | 2.14 | 3.49 | 4.74 | 4.88 | 4.20 | 2.46 | 3.85 | 3.5 | 3.27 | 2.99 | 2.19 | 2.95 | 3.17 |
| Golestan | ||||||||||||||
| Male | 5.75 | 4.84 | 6.34 | 7.61 | 4.30 | 9.23 | 8.31 | 7.28 | 8.27 | 7.95 | 8.81 | 10.20 | 7.20 | 7.09 |
| Female | 3.14 | 2.37 | 2.17 | 2.80 | 0.85 | 1.65 | 2.20 | 1.57 | 1.81 | 1.86 | 1.9 | 2.04 | 4.27 | 2.39 |
| Hamedan | ||||||||||||||
| Male | 7.84 | 9.13 | 12.20 | 12.54 | 16.92 | 14.37 | 11.20 | 14.16 | 13.24 | 12.87 | 12.9 | 12.60 | 11.70 | 12.05 |
| Female | 1.08 | 1.28 | 3.24 | 2.11 | 2.16 | 2.18 | 2.15 | 2.16 | 2.16 | 2.16 | 2.28 | 2.51 | 1.96 | 2.07 |
| Hormozgan | ||||||||||||||
| Male | 2.71 | 7.87 | 3.79 | 3.95 | 6.26 | 5.45 | 4.13 | 5.28 | 4.95 | 4.79 | 6.01 | 8.30 | 10.10 | 5.84 |
| Female | 0.92 | 1.17 | 0.23 | 1.21 | 2.17 | 1.93 | 2.04 | 2.05 | 2.01 | 2.03 | 2.17 | 2.46 | 1.23 | 1.48 |
| Ilam | ||||||||||||||
| Male | 2.33 | 3.75 | 2.28 | 4.48 | 5.49 | 4.69 | 5.45 | 5.21 | 5.12 | 5.26 | 5.63 | 6.50 | 6.30 | 4.58 |
| Female | 0.49 | 1.92 | 0.49 | 0.63 | 1.28 | 0.96 | 0.47 | 0.9 | 0.78 | 0.72 | 1.08 | 1.75 | 0.67 | 0.96 |
| Isfahan | ||||||||||||||
| Male | 7.64 | 12.37 | 11.78 | 14.43 | 16.83 | 16.33 | 15.95 | 16.37 | 16.22 | 16.18 | 16.53 | 17.20 | 18.80 | 14.59 |
| Female | 2.11 | 3.13 | 2.53 | 3.13 | 3.74 | 3.42 | 3.11 | 3.42 | 3.32 | 3.28 | 3.38 | 3.55 | 3.72 | 3.16 |
| Kerman | ||||||||||||||
| Male | 6.29 | 7.73 | 9.71 | 9.41 | 11.17 | 13.20 | 14.66 | 13.01 | 13.62 | 13.76 | 18.23 | 27.30 | 22.40 | 13.54 |
| Female | 2.07 | 2.40 | 1.76 | 3.91 | 3.31 | 3.27 | 4.35 | 3.64 | 3.75 | 3.92 | 4.01 | 4.37 | 4.26 | 3.3 |
| Kermanshah | ||||||||||||||
| Male | 14.62 | 10.61 | 11.03 | 9.32 | 12.64 | 13.55 | 15.74 | 13.98 | 14.42 | 14.71 | 13.25 | 10.60 | 12.40 | 12.28 |
| Female | 3.50 | 2.08 | 2.24 | 2.64 | 3.17 | 3.90 | 4.39 | 3.82 | 4.04 | 4.08 | 3.2 | 1.49 | 2.52 | 2.88 |
| Khorasan Razavi | ||||||||||||||
| Male | 6.65 | 7.73 | 5.78 | 9.88 | 10.53 | 12.43 | 9.99 | 10.98 | 11.13 | 10.7 | 11.75 | 13.40 | 10.80 | 9.69 |
| Female | 2.12 | 2.80 | 1.45 | 3.07 | 3.74 | 3.60 | 3.04 | 3.46 | 3.37 | 3.29 | 3.15 | 2.79 | 2.63 | 2.80 |
| Khuzestan | ||||||||||||||
| Male | 7.22 | 6.83 | 7.11 | 9.84 | 8.90 | 11.71 | 10.52 | 10.38 | 10.87 | 10.59 | 11.49 | 13.00 | 13.90 | 9.89 |
| Female | 2.56 | 1.56 | 2.33 | 3.52 | 2.37 | 5.17 | 2.79 | 3.44 | 3.8 | 3.34 | 3.43 | 3.13 | 2.96 | 2.93 |
| Kohkilouye va Boyer Ahmad | ||||||||||||||
| Male | 1.30 | 10.54 | 7.74 | 11.91 | 8.99 | 9.18 | 8.98 | 9.05 | 9.07 | 9.03 | 10.1 | 12.20 | 12.10 | 9.21 |
| Female | 0.00 | 3.19 | 0.40 | 0.25 | 2.66 | 1.00 | 1.93 | 1.86 | 1.6 | 1.8 | 2.92 | 5.36 | 2.10 | 1.87 |
| Kurdistan | ||||||||||||||
| Male | 5.81 | 8.10 | 12.24 | 11.76 | 10.02 | 11.41 | 10.27 | 10.57 | 10.75 | 10.53 | 10.36 | 9.80 | 10.70 | 10.01 |
| Female | 3.58 | 2.52 | 2.24 | 1.95 | 3.22 | 3.28 | 3.22 | 3.24 | 3.25 | 3.24 | 2.65 | 1.47 | 3.59 | 2.78 |
| Lorestan | ||||||||||||||
| Male | 5.40 | 9.52 | 8.64 | 8.24 | 10.39 | 13.03 | 12.50 | 11.97 | 12.5 | 12.32 | 11.01 | 8.20 | 8.80 | 9.41 |
| Female | 0.42 | 2.62 | 2.71 | 2.40 | 3.22 | 3.96 | 2.93 | 3.37 | 3.42 | 3.24 | 2.64 | 1.26 | 3.75 | 2.58 |
| Markazi | ||||||||||||||
| Male | 7.36 | 9.83 | 10.15 | 9.68 | 11.63 | 11.17 | 16.06 | 12.95 | 13.39 | 14.14 | 12.44 | 9.80 | 12.60 | 10.92 |
| Female | 1.70 | 1.81 | 2.12 | 2.16 | 3.30 | 2.85 | 2.72 | 2.96 | 2.84 | 2.84 | 2.49 | 1.78 | 1.59 | 2.22 |
| Mazandaran | ||||||||||||||
| Male | 7.91 | 10.72 | 10.83 | 8.70 | 8.16 | 8.81 | 11.19 | 9.39 | 9.8 | 10.12 | 10.17 | 10.60 | 11.40 | 9.81 |
| Female | 1.19 | 1.89 | 2.46 | 3.45 | 1.80 | 2.67 | 1.80 | 2.09 | 2.19 | 2.03 | 2.22 | 2.46 | 2.37 | 2.23 |
| North Khorasan | ||||||||||||||
| Male | 6.65 | 7.73 | 3.77 | 5.00 | 5.42 | 6.59 | 4.87 | 5.63 | 5.7 | 5.4 | 7.06 | 10.10 | 10.90 | 6.78 |
| Female | 2.12 | 2.80 | 1.00 | 1.23 | 1.89 | 1.99 | 1.29 | 1.72 | 1.67 | 1.56 | 2.38 | 3.90 | 1.91 | 2.01 |
| Qom | ||||||||||||||
| Male | 3.70 | 10.46 | 7.30 | 6.82 | 9.49 | 9.80 | 4.52 | 7.94 | 7.42 | 6.63 | 7.02 | 5.91* | 6.89* | 7.44 |
| Female | 2.31 | 0.46 | 4.73 | 1.87 | 0.94 | 1.30 | 1.60 | 1.28 | 1.39 | 1.42 | 1.41 | 1.24* | 1.36* | 1.89 |
| Semnan | ||||||||||||||
| Male | 5.04 | 9.00 | 10.75 | 14.79 | 10.76 | 16.50 | 10.72 | 12.66 | 13.29 | 12.22 | 13.01 | 13.50 | 19.10 | 12.24 |
| Female | 0.54 | 3.03 | 5.03 | 3.32 | 3.91 | 3.42 | 3.48 | 3.6 | 3.5 | 3.53 | 3.12 | 2.33 | 2.21 | 3.03 |
| Sistan va Baluchestan | ||||||||||||||
| Male | 1.62 | 1.24 | 2.19 | 2.80 | 2.41 | 1.96 | 2.27 | 2.21 | 2.15 | 2.21 | 3.59 | 6.40 | 6.20 | 3.01 |
| Female | 0.39 | 0.92 | 0.72 | 0.50 | 1.19 | 1.06 | 1.04 | 1.1 | 1.07 | 1.07 | 1.76 | 3.14 | 2.41 | 1.26 |
| South Khorasan | ||||||||||||||
| Male | 6.65 | 7.73 | 10.29 | 9.61 | 0.30 | 8.75 | 7.00 | 5.35 | 7.03 | 6.46 | 8.16 | 11.00 | 8.80 | 7.79 |
| Female | 2.12 | 2.80 | 7.96 | 2.44 | 0.49 | 5.66 | 1.46 | 2.54 | 3.22 | 2.41 | 3.17 | 3.90 | 2.55 | 3.26 |
| Tehran | ||||||||||||||
| Male | 15.20 | 7.70 | 10.03 | 9.41 | 9.14 | 21.24 | 15.79 | 15.39 | 17.47 | 16.22 | 16.86 | 16.9 | 14.20 | 13.29 |
| Female | 4.01 | 2.26 | 2.65 | 2.00 | 2.42 | 5.05 | 4.54 | 4 | 4.53 | 4.36 | 4.07 | 3.33 | 2.64 | 3.21 |
| West Azerbaijan | ||||||||||||||
| Male | 8.48 | 10.25 | 11.08 | 10.89 | 13.37 | 9.97 | 10.60 | 11.31 | 10.63 | 10.85 | 14.06 | 20.70 | 15.60 | 12.33 |
| Female | 1.47 | 2.72 | 2.85 | 2.49 | 2.02 | 1.94 | 4.00 | 2.65 | 2.86 | 3.17 | 3.49 | 4.42 | 3.25 | 2.793 |
| Yazd | ||||||||||||||
| Male | 9.85 | 10.26 | 11.24 | 13.91 | 16.09 | 15.46 | 17.05 | 16.2 | 16.24 | 16.5 | 19.21 | 24.90 | 17.40 | 15.13 |
| Female | 3.59 | 2.53 | 3.64 | 2.09 | 3.90 | 3.80 | 4.24 | 3.98 | 4.01 | 4.08 | 3.74 | 3.13 | 3.16 | 3.34 |
| Zanjan | ||||||||||||||
| Male | 7.00 | 8.79 | 9.51 | 8.54 | 9.28 | 9.60 | 8.74 | 9.21 | 9.18 | 9.04 | 9.84 | 11.30 | 10.80 | 9.28 |
| Female | 2.04 | 2.77 | 1.10 | 1.98 | 1.90 | 3.19 | 1.20 | 2.1 | 2.16 | 1.82 | 1.86 | 1.60 | 0.94 | 1.88 |
Abbreviation: ASIR, age-standardized incidence rate.
a Results are provided by time series model.
Age-standardized incidence rates (ASIRs) per 100,000 of male bladder cancer among provinces of Iran in 2015 (20)
Age-standardized incidence rates (ASIRs) of female bladder cancer among provinces of Iran in 2015 (20)
5. Discussion
While cancer is the third leading cause of mortality in Iran (21), few epidemiological studies have been conducted related to this issue. In this study, we used data from Iran’s Ministry of Health and Medical Education to present the most recent trends of bladder cancer incidence in the country and its provinces from 2003 to 2015.
We showed that the ASIR of bladder cancer increased from 8.35 in 2003 to 13.57 in 2015 among men. ASIR of bladder cancer also showed a slight increase in females (2.12 in 2003 versus 2.86 in 2015), which indicates that the rise of bladder cancer ASIR in men (63%) has been much higher than in women (35%) through the years of the study. In 2015, the ASIR of bladder cancer among Iranian males and females was 13.57 and 2.86, respectively. Although the incidence rate of bladder cancer in men in Iran is higher than in Asian countries such as Bhutan (1.1 in 100,000), Vietnam (1.8 in 100,000), and Mongolia (2.2 in 100,000), this incidence in comparison to West Asian countries and Iran’s neighbors including Lebanon (29.1 per 100,000), Turkey (28.7 per 100,000) and Armenia (27.3 per 100,000) are significantly lower (22). However, the incidence rate of bladder cancer is comparable to the global average (11.81 in men and 2.69 in women) but illustrating the incidence trend shows an opposite development of this cancer in our country. Although ASIR of bladder cancer incidence in Iran has increased in years 2003 to 2015 among both men and women, the global trend of bladder cancer has declined globally from 1990 to 2016 (1).
During the years of the study, the highest ASIRs of men and women with bladder cancer (14.42 and 3.78 per 100,000, respectively) were observed in 2008. Bladder cancer in both sexes occupied the fifth rank of all cancers and bladder cancer in men was the third cancer in Iran (16). In the interpretation of our results, we found that in 2008, the incidence of bladder cancer in women and men in Tehran, Gilan, and East Azerbaijan provinces had a sharp increase compared to the previous and subsequent years. For example, bladder cancer in men in 2008 was 21.24 per 100,000 people, while it was 9.14 per 100,000 people in the previous year and 15.79 per 100,000 people in the following year, which indicates a sharp increase in a short time. To explain the reason for these increases, in addition to checking the accuracy of information registration, more detailed investigations are needed, especially regarding environmental factors in these regions.
Our results showed that the incidence rate of bladder cancer is higher in men as only 17.8% of all bladder cancers occurred in women. This is similar to global numbers where approximately 23% of new cases of bladder cancer are females (1). Moreover, we showed that the incidence of bladder cancer is higher in the older population. Iranian males and females have life expectancies of 81.6 and 71.6, respectively, which have been increasing constantly over the last 40 years (23). If the trend continues, the incidence rate of bladder cancer increases may increase further due to the aging of the population. Interestingly, our hypothesis is supported by a recent study by Roshandel et al. that predicts an overall increase in the number of new cases with bladder cancer in Iran including a 26.2% rising by 2025 (13).
Assessing cancer incidence based on the different geographical distributions has a significant impact on the formation of a new hypothesis that can not only indicate the potential risk factors of bladder cancer but can also lead to the emergence of methods of prevention or screening of high-risk individuals. The incidence in a particular area changes over time while the actual increase in cancer in an area can be explained by the increased exposure to a variety of carcinogens, it should be noted that early screening programs can lead to a false increase in cancer rates due to early detection of cancer (24).
Notably, the highest incidence rates of bladder cancer in Iran are reported in Kerman province (27.30 per 100,000) in 2014 which could compatible with the prevalence of opium addiction in this area. Investigating the risk factors of bladder cancer in Iran by Shakhssalim et al. and Ghadimi et al. revealed that some lifestyle factors, such as opium consumption, may play an important role in the development of bladder cancer in our region (25, 26). Opium is one of the most frequently used drugs that have been widespread from hundred years ago in Iran and unfortunately, the number of opium abusers has increased by about 8% annually in the country (27). North and southern regions of the country are reported as high-risk areas in terms of opium consumption (28, 29). It has been found in Iran that the use of opium leads to an increased risk of bladder cancer by 4.60 times (30). Our results emphasize the need for more research and supervision of addiction control in these areas.
Our results found the high-risk provinces in Iran; the highest ASIR of bladder cancer in men is related to Yazd (15.13 per 100,000) followed by Isfahan (14.59 per 100,000), and Gilan (14.12 per 100,000) and the highest ASIR of bladder cancer in women is related to Bushehr (3.69 per 100,000) followed by Yazd (3.34 per 100,000) and Fars (3.33 per 100,000) showing the spatial distribution of bladder cancer in hot and arid regions in Iran. Iran is a vast country with diverse kinds of climates including mild and wet on the northern coast, continental and arid in the central plateau, cold in the high mountains, desert hot in the southeast and on the southern coast. The higher incidence of bladder cancer in arid and hot areas of Iran with a lower density of population underscores the need for further ecological investigations to find the associated risk factors. High temperature, ultraviolet radiation, soil, and water component are the risk factors that may be effective in the higher incidence rate of bladder cancer.
Iran is a developing country and as mentioned previously, its population is getting older. Therefore, bladder cancer incidence is likely to rise, as older age groups are more likely to be diagnosed with bladder cancer. Also, higher age might worsen the complications and burden of the disease.
Smoking and increased fasting plasma glucose play a crucial role in the burden of bladder cancer (2). However, some important risk factors of bladder cancer such as smoking and obesity (31) are modifiable and the importance of educational and preventive strategies cannot be overstated. Inequality in health resource allocation may also contribute to varying incidence rates in different provinces; for instance, lower ASIRs of bladder cancer in Sistan and Balouchestan, and Ilam can be due to inequity in diagnostic facilities in these provinces however developing precise investigations in this regard is necessary.
5.1. Conclusions
The increasing trend of bladder cancer incidence in Iran which is despite of clear decreasing global trend accompanying to ongoing aging of the population highlights the disease as a potential health problem in the upcoming years in Iran. The higher incidence of bladder cancer in arid and hot areas of Iran underscores the need for further epidemiological investigations to find the associated risk factors. Therefore, it is necessary for health organizations to implement effective research and control programs including public awareness programs to avoid smoking and drugs, follow a healthy diet, timely treatment of urinary infections, avoid certain chemical exposure at the workplace as well as provide the necessary facilities for timely diagnosis and rapid treatment of bladder cancer in all parts of the country to prevent further increases in the disease burden.