1. Background
The mediastinal lymph nodes are effective and helpful in examining infections such as tuberculosis, lung cancer, sarcoidosis, lymphoma, silicosis, and asbestosis. Mediastinal nodal staging is a crucial step in management and treatment decision in patients with lung cancer because the presence of nodal metastasis affects prognosis and suitability for surgical treatment. The noninvasive evaluation of metastatic infiltration of hilar and mediastinal lymph nodes is based on Computed tomography (CT) scan or Magnetic resonance imaging (MRI). Lymph nodes with short axis diameter of 1 cm or larger are regarded as metastases (1, 2).
The mediastinal lymph nodes are further investigated in five sites and are treated in radiological reports: (1) supraclavicular lymph nodes, (2) superior mediastinal lymph nodes, (3) aortic lymph nodes, (4) inferior mediastinal lymph nodes, (5) hilar, lobar and segmental glands (3). Tuberculin skin testing is a reliable tool for investigating primary mycobacterial infections. The correct interpretation of this test requires accurate and sufficient information. In this test, the appropriate antigen is tuberculin purified protein derivative (PPD) (4, 5). In all routine tests, a moderate PPD dose should be used. In most countries, especially the United States, this dose consists of 5 units standardized by biological measurement versus reference antigen (PPD-Standard) (6). The tuberculin test is usually performed on the forearm's ventral surface. The reactions are calculated by measuring the transverse diameter of the hardened area through touching after 48 and 72 hours. If the induration diameter is < 5, 5 - 10, and > 10 mm, the result is negative, suspected, and positive, respectively (4, 6). The Mantoux test (tuberculin) is widely used in determining latent tuberculosis infection. This test also examines people with suspected active TB but whose sputum mycobacterium culture is negative. It is usually recommended to read the test results (Mantoux method) 48 and 72 hours after injection (7). Following the incidence of Mycobacterium tuberculosis in regional lymph nodes, T lymphocytes become sensitive to mycobacterial antigens, multiply, enter the bloodstream after 3 - 8 weeks, and remain active for years. Subsequent stimulation of these sensitized lymphocytes with antigens such as tuberculin solution leads to further stimulation of these cells and local reactions. Delayed reactions to tuberculin solution begin within the first 5 - 6 hours and reach their peak value within 48 - 72 hours later (8, 9). The results of the tuberculin test in vaccinated individuals can confirm or rule out the diagnosis of tuberculosis infection. However, in vaccinated individuals, using interferon-gamma release measurement tests is superior to the tuberculin test (10).
2. Objectives
Chest radiography is a simple, inexpensive, and essential method for examining the mediastinal lymph nodes. On the one hand, there has been no study on changes in the density of mediastinal lymph nodes and PPD, and the findings of the present study can help in diagnosing a people's previous exposure to tuberculosis and the possibility of its activation in immunodeficiency processes. On the other hand, tuberculosis prevalence is increasing due to the increased number of people with decompensated immune system. Moreover, the results of the present study could be of great help to these individuals. Therefore, we decided to study PPD changes based on mediastinal lymph node density.
3. Methods
This cross-sectional observational study was performed on 130 patients referred to Valiasr and Amir Al-Momenin Hospitals, Arak, Iran to undergo a CT scan for non-infectious and non-tumor reasons. Inclusion criteria included patients above 18 years of both sexes; patients who underwent CT scans for non-infectious and non-tumorous reasons; non-pregnant and non-breastfeeding mothers; and the absence of immunodeficiency disease. The exclusion criterion also included reluctance to participate in the study.
Patients initially underwent non-contrast CT scans, and their mediastinal lymph node density was measured and recorded based on Hounsfield units. Then, we obtained their written informed consent to undergo a tuberculin test. Patients were evaluated for changes in the tuberculin test. All patients went to the reference laboratory. The tuberculin test was then performed, and the results were evaluated within 72 hours. A syringe with a very fine needle was filled with 0.1 mL of PPD solution. PPD was then injected into the forearm skin layers. Unlike conventional vaccination, which is injected deep into a muscle, PPD injection is superficial in forming a raised spot. If no spot appears during the injection, the test should be repeated. The skin spot disappears spontaneously within a few hours. The injection is given in an area of the forearm with no sores or veins. The skin reaction is very specific when a person suffers from TB. Therefore, this test can be used as a reliable method to identify people with tuberculosis. The peak of the induration reaction occurs after 27 - 84 hours of the test injection, which is the time required to examine the target area. The test result may be misread if this time is prolonged or shortened. A positive reaction causes symptoms of redness, itching, and thickening of the skin layer (stiffness). The presence or absence of stiffness and size is the most critical indicator in distinguishing a positive result from a negative one. The redness or bruising is not considered in determining the results of this test. Fluid-filled blisters or sores are also regarded as symptoms of a positive test. The resulting number was then written. According to the test, if the induration diameter is < 5, 5 - 10, and > 10 mm, the result is negative, suspected, and positive, respectively. Finally, data analysis was carried out using SPSS software ver. 20.
4. Results
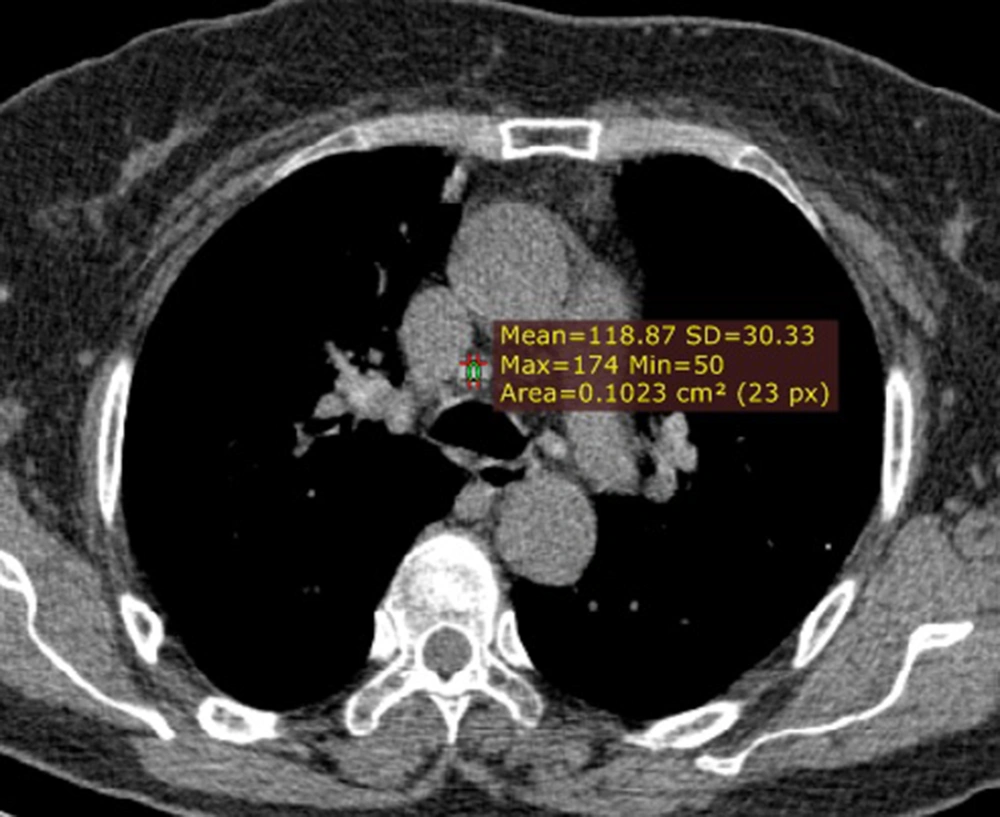
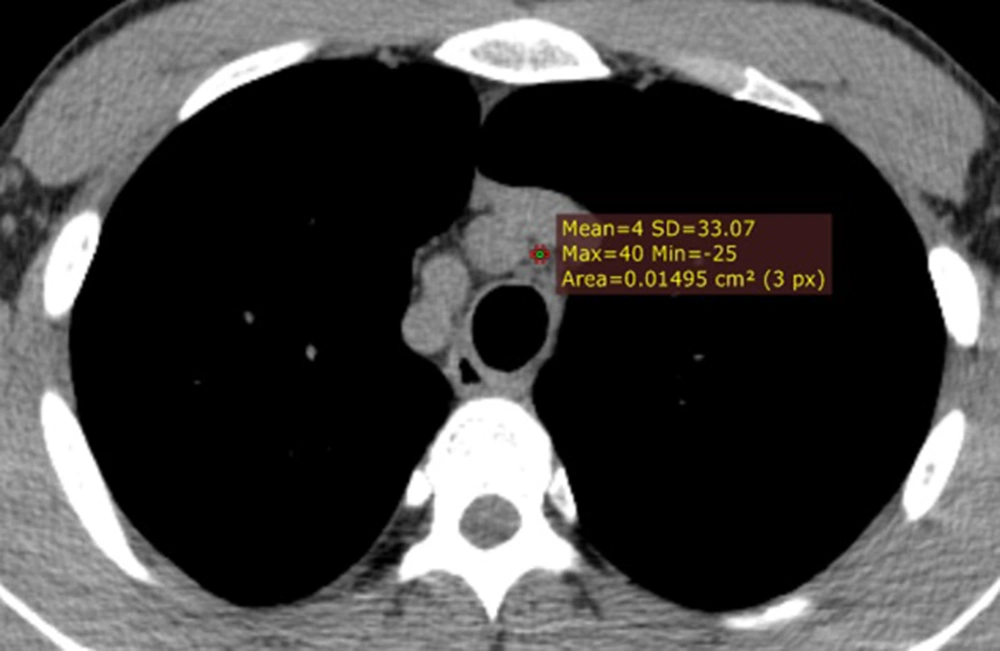
The minimum and maximum age ranges were 20 and 76 years, respectively. The mean ± SD of patients’ age was 47.51 ± 16.72 years. Of the 130 patients included in the study, 69 (53.1%) were male, and 61 (46.9%) were female. The median (Interquartile range = IQR) density of lymph nodes was 55.23 (39) HU. The minimum and maximum densities were 0 and 180, respectively (Figures 1 & 2). The frequency of tuberculin test results is given in Table 1. The mean tuberculin test induration diameter was 15.93 ± 1.50 mm. The minimum and maximum of the tuberculin test induration diameter were 1 mm and 52 mm, respectively. A total of 63(48.5%) subjects had a positive test result (> 10 mm).
| Group | No. (%) |
|---|---|
| Induration diameter < 5 mm (negative) | 38 (29.2) |
| Induration diameter 5 - 10 mm (suspected) | 29 (22.3) |
| Induration diameter > 10 mm (positive) | 63 (48.5) |
a A total of 63 subjects (48.5%), had a positive test result (> 10 mm).
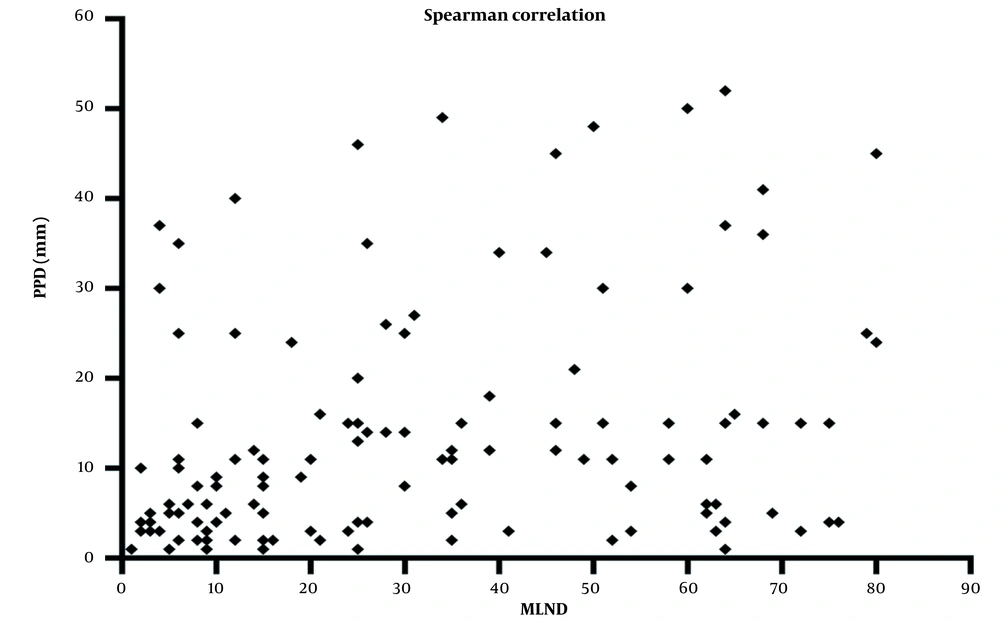
Figure 3 presents the correlation between mediastinal lymph node density and tuberculin test reaction diameter. It can be seen that there is a significant relationship between the density of mediastinal lymph nodes and the diameter obtained in the tuberculin test (P < 0.001). The correlation coefficient is 0.416, which is a number between 0 and 1. There is a positive correlation between the mediastinal lymph node density and the induration diameter, i.e., the induration diameter increases with increasing lymph node density. There was a negative correlation between mediastinal lymph node density and age, i.e., mediastinal lymph node density decreased with increasing age (P < 0.001, r = -0.616).
Comparison of mean and standard deviation of mediastinal lymph node density and sex (Table 2) revealed that there is a significant relationship between mediastinal lymph node density and sex (P = 0.022), and the huns field number of lymph nodes is higher in men than in women.
| Variable | Women, Mean ± SD | Men, Mean ± SD | P-Value |
|---|---|---|---|
| Lymph node density | 50.5 ± 5.31 | 72.5 ± 13.31 | 0.022 |
5. Discussion
Based on the results of the present study, the minimum and maximum age ranges were 20 and 76 years, respectively. The mean ± SD of the patients’ age was 47.51 ± 16.72 years. Of the 130 patients included in the study, 69 (53.1%) were male, and 61 (46.9%) were female. The median (IQR) density of lymph nodes was 55.23 (39) UT. The mean induration diameter of the tuberculin test was 15.93 ± 1.50 mm. A total of 63 (48.5%) subjects had a positive test result (> 10 mm). There was a positive correlation between mediastinal lymph node density and tuberculin test induration diameter in individuals; i.e., with increasing lymph node density, tuberculin test induration diameter also increased (r = 0.416, P < 0.001). Lymph node density was also higher in men than in women (P = 0.022). Tang et al. conducted a study to differentiate between tuberculosis and lymphoma in the mediastinal lymph nodes. The findings of their research suggested that the description of the anatomical distribution and pattern of increased lymphadenopathy, shown in contrast-enhanced MDCT, can be helpful in the diagnosis of cells with lymphoma in the mediastinal lymph nodes (11). In addition, this results result may be helpful in the earlier diagnosis of patients with pulmonary tuberculosis. Mukund et al. conducted a study to investigate the pattern of lymph node CT scans in pediatric pulmonary tuberculosis. Increased mediastinal lymph nodes were found in 96.7% of cases; The treatment reduced the lymph node size in 87.4% of cases (12). In fact, Mukund et al. reported a reduction in the lymph size after treatment, and the current study also showed a positive relationship between lymph node density and tuberculin test induration diameter. Andronikou et al. also surveyed mediastinal tuberculous lymphadenitis CT scan results on one hundred children (54 boys, 46 girls) with clinically suspected pulmonary tuberculosis. They found the prevalence, distribution, and characteristics of mediastinal lymph nodes on a CT scan. Lymph nodes were present in 92 patients, and nodes larger than 1 cm in diameter were present in 46 patients. Increased lymph node size was observed in 67 patients. Calcification was also presented in only nine patients. The most common site of lymphadenopathy was the sub carinal region (n = 90 patients), followed by the anterior mediastinal region (n = 79 patients) (13). In agreement with the results of other studies showing an increase in tuberculosis with an increase in lymph node size or a decrease in size with treatment of the disease, the results of the present study also show a positive correlation between tuberculin test induration diameter (suffering from tuberculosis) and mediastinal lymph node density.
Although this study found a significant correlation between mediastinal lymph node density and tuberculin test induration diameter, considering that the present study was cross-sectional and that there is a possibility of selection bias in individuals, as well as the possibility of misclassification bias in the classification of individuals, also because of the nature of the study design and the type of analysis, it is suggested that stronger studies be conducted with a larger sample size and with the presence of a comparison group. QuantiFERON-TB (QFT) test had more accuracy than the ppd test. Therefore, we recommend this test should be employed in future studies.
5.1. Conclusions
There is a positive correlation between mediastinal lymph node density and tuberculin test induration diameter; tuberculin test induration diameter increases with increasing lymph node density. Lymph node density was also higher in men than women. Therefore, the results of the present study can play a role in helping earlier diagnosis of pulmonary tuberculosis. It is also recommended to measure mediastinal lymph node density in individuals.