1. Background
Leukemia accounts for approximately 8% of all cancers and is the fifth most common cancer worldwide (1). Patients with hematologic malignancies have been classified into 6 groups: Acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), chronic myeloid leukemia (CML), chronic lymphocytic leukemia (CLL), Hodgkin's lymphoma, and non-Hodgkin's lymphoma (1).
According to the increasing incidence of cancers, especially hematologic malignancies, in the population, and the prevalent occurrence of pulmonary symptoms, especially pneumonia, in these patients, diagnosis of symptoms and subsequent complications in the early stages of the disease appears to be helpful in increasing patient survival. Pneumonia in immunocompromised cancer patients can be fatal, and prompt initiation of primary treatment may be a safe and effective way to reduce morbidity and mortality in these patients (2-4). A high mortality rate (approximately 60%) has been reported in leukemia patients with radiological pulmonary infiltration (5). Scientific advances in the diagnosing and managing patients with blood malignancies and treatment-related complications, have increased survival rates. Nevertheless, more than half of patients with hematologic malignancies develop pulmonary complications during their follow-up (6).
Computed tomography is a rapid, easily accessible, and inexpensive assessment tool with a radiation dose in the acceptable range and a very high accuracy coefficient for physicians (7). Chest computed tomography (CT) scan is usually performed in patients with hematologic malignancies for two purposes: (1) early detection of the lesions that are not visible and detectable on chest X-rays, and where clinicians do not agree on the nature of lesion or its diagnosis. (2) better description of CXR findings and recognition of disease progression (8). Advances in science and technology, particularly in the field of diagnostic imaging, and the availability of new multi-slice CT scanners allow clinicians to obtain comprehensive and accurate information about the patient's lung, its parenchyma, and patterns of pulmonary involvement in a short period of time (7). Because many of these patterns have their own definitions in radiology and may predict the type of organism affecting the lung, physicians can initiate the proper treatment for the patient rather than performing time-consuming routine tests such as blood and sputum cultures (9). In addition, CT scan provides comprehensive information on lymphadenopathy, vascular and thromboembolic involvements (when venous contrast is used), and detection of lung mass (nodule larger than 30 mm in largest diameter) (10, 11) in the context of primary malignancy, pleural and pericardial effusion, signs of atherosclerotic and fibrotic changes, and pulmonary hypertension (7). This is of great value for optimizing treatment, depending on the general condition of the patient and the primary pathology.
2. Objectives
The aim of the present study was to determine the frequency of findings of thoracic CT scans in adults with different hematologic malignancies, who were admitted for acute chest symptoms, in addition to their clinical /other paraclinical data in order to make the most accurate diagnosis. However, in cases of missing some paraclinical information (in a few participants), it was not possible to reach an accurate diagnosis.
3. Methods
This study was a retrospective study conducted on 200 patients diagnosed with hematologic malignancy who were referred to Khansari cancer center, Arak, Iran with acute chest symptoms. Spiral CT scans of the chest without contrast were performed using the GE Optima 580RT 16 SLICE. If pulmonary thromboembolism (PTE) was suspected, a contrast-enhanced CT scan was performed at the discretion of the physician. A checklist was completed in all patients who underwent a thoracic CT scan, including demographic data, smoking status, history of obstructive or restrictive lung disease, and radiotherapy and chemotherapy. All procedures performed in the study were confirmed by the Ethical Committee of the Arak University of Medical Sciences (approval ID = IR.ARAKMU.REC.1398.210).
3.1. Inclusion and Exclusion Criteria
Patients diagnosed with six hematologic malignancies who had acute pulmonary symptoms, at least 18 years of age, male or female, and at least 6 months passed from initial diagnosis were included in this study. Participants were excluded from the study if they met any of the following criteria; unwillingness to participate in the study, refusal to cooperate further, presence of concomitant malignancies (other than hematological defined malignancies), history of proven lung disease before hematologic malignancy, presence of a specific risk factor for pulmonary pathology (miners, exposure to asbestos, and environmental /occupational poisons), and low-quality and non-diagnostic CT scan images (severe movement artifact, use of special instruments producing artifacts, low-quality images due to suboptimal parameters of scanning).
The bedside clinical symptom checklist includes pleuritic chest pain, fever (axillary temperature above 38°C), cough (productive or non-productive), dyspnea/shortness of breath, tachypnea (respiratory rate above 20 per minute), respiratory distress, hemoptysis, oxygen dependence (constant need for nasal or oral mask oxygen), and endotracheal tube dependency was also written in the checklist. The paraclinical questionnaire consisting of leukocytosis (WBC count greater than 11,000 µL), neutropenia (neutrophil count less than 1500 µL), anemia (HB less than 12 in women and less than 14 g/dL in men), thrombocytopenia (platelet count less than 150,000 µL), D-dimer, and lung biopsy (if available) which were then followed up with continuous daily testing.
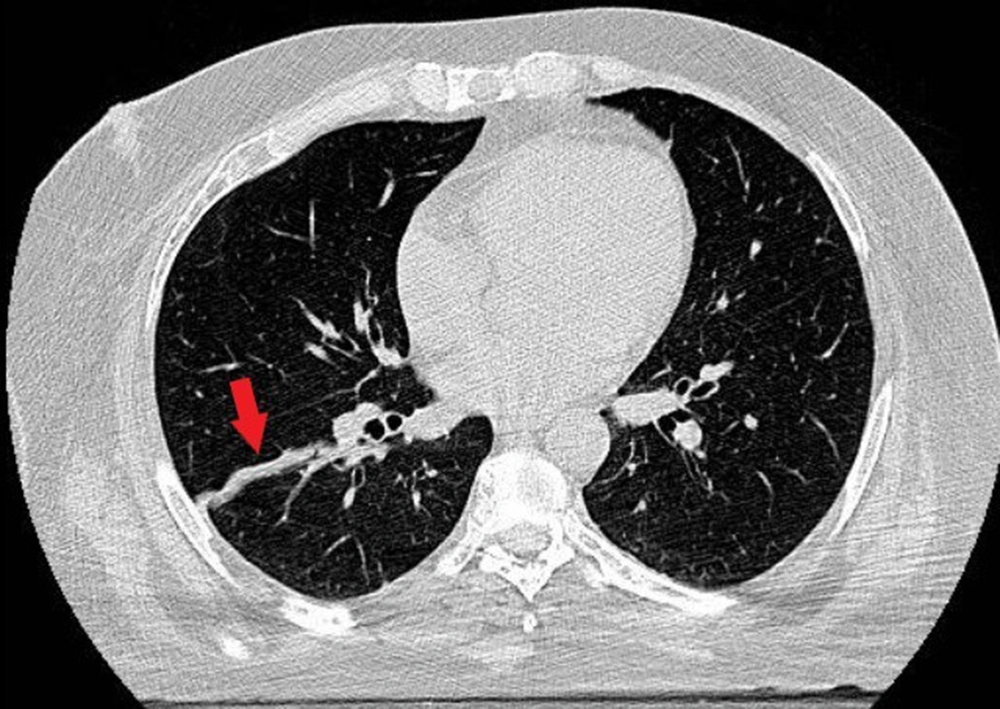
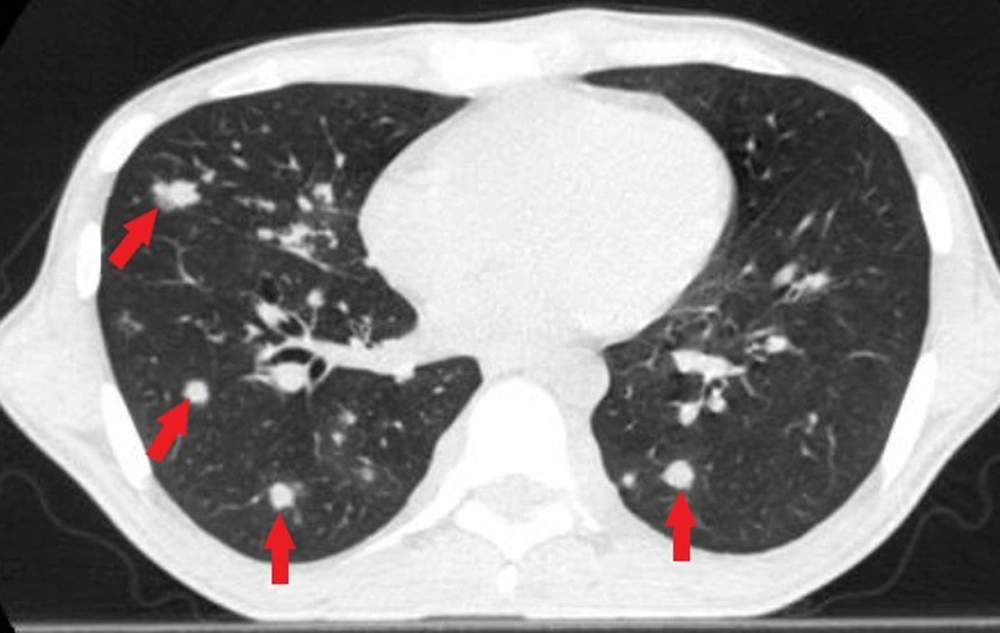
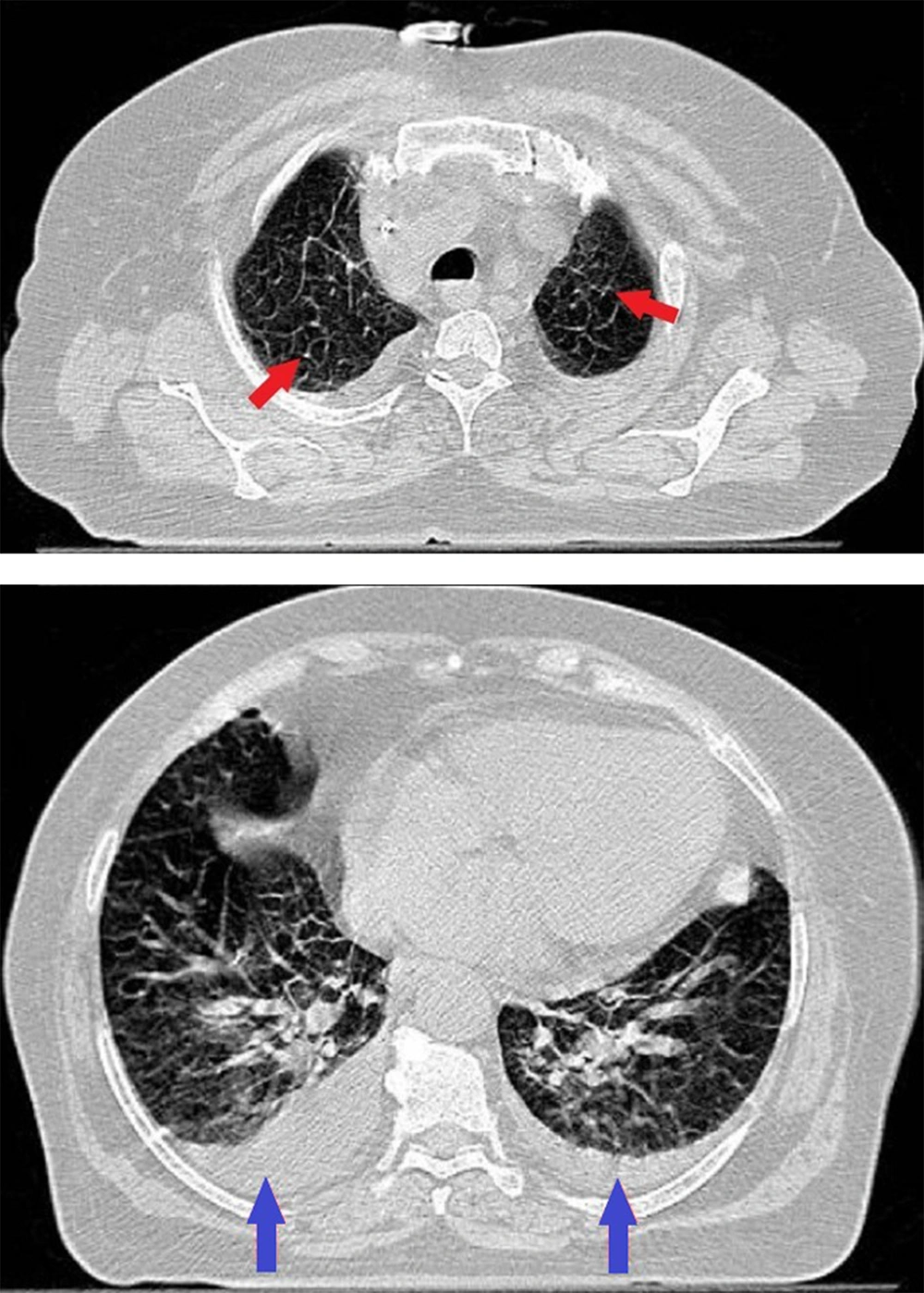
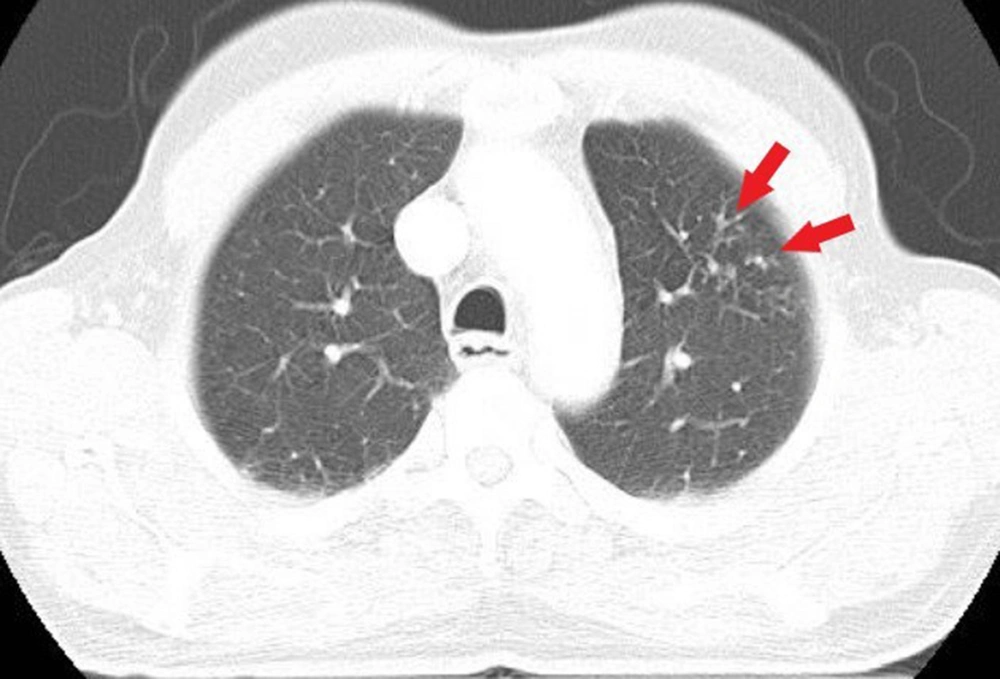
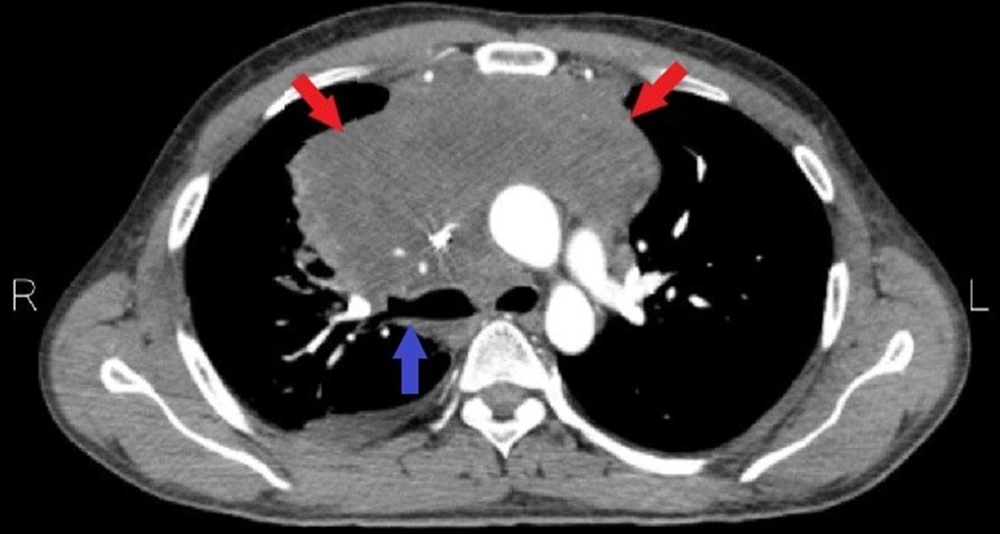
CT images obtained from the patients were fully examined for lung and soft tissue windows in all three axial, coronal, and sagittal sections using the PACS system (picture archiving and communication system) owned by the hospital. All CT scans were obtained using the same machine from a reputable university educational center. In addition, the CT scan findings were confirmed by two radiologists with at least 5 years of experience in the field and two radiology residents. In case of disagreement between radiologists (and radiology residents), the issue was resolved by consensus. Radiological findings based on a checklist (definition according to fleischner society) (11) were completed, including pleural effusion, pericardial effusion, pulmonary nodule (rounded opacity, well or poorly defined, measuring up to 3 cm in diameter), mass (any pulmonary, pleural, or mediastinal lesion seen on chest radiographs as an opacity greater than 3 cm in diameter without regard to contour, border, or density characteristics), consolidation, ground glass opacity (GGO), pneumothorax, empyema, evidence of left heart disease (calcified coronary arteries, prominent heart apex, prominent thoracic aorta [ectasia of ascending aorta greater than 35 mm]), atelectasis, the tree in bud pattern, emphysema, plural thickening, filling defect in the pulmonary artery (in cases of contrast-enhanced CT scan), mediastinal lymphadenopathy, peribronchial thickening, mosaic pattern, bronchial dilatation or narrowing, thickening of interlobular septa, cavities, pulmonary hypertension (diameter of pulmonary trunk more than 30 mm), pulmonary mass (nodule larger than 3 cm), and presence of Halo sign. The distribution of CT scan findings according to vascular, mediastinal, pleural, and pulmonary findings is shown in Table 1. CT scan images of the findings in patients with hematologic malignancies are shown in Figures 1 to 6.
| Type | Findings |
|---|---|
| Pulmonary | Atelectasis |
| Consolidation | |
| Ground glass opacity (GGO) | |
| Pulmonary nodule | |
| Tree in bud pattern/centrilobular nodule | |
| Pulmonary mass | |
| Mosaic attenuation | |
| Interlobular septal thickening | |
| Peribranchial thickening | |
| Bronchial narrowing | |
| Cavity | |
| Halo sign | |
| Mediastinal | Mediastinal lymphadenopathy |
| Vascular | Pulmonary hypertension |
| Feeling defect in the pulmonary artery | |
| Evidence of left heart disease | |
| Pleural | Pleural effusion |
| pneumothorax | |
| Pleural thickness |
Considering the results of CT scans, laboratory tests, clinical symptoms, and the patient’s history, the closest diagnoses were selected from a range of pulmonary pathologies for each patient. In some patients, more than one pulmonary pathology was reported. Two radiologists independently reviewed the images from the patients’ CT scan and any discrepancy was resolved by their discussion of the consensus.
3.2. Data Analysis
Data were carefully recorded in Excel format and double-checked by a second researcher (NN). Data were analyzed by SPSS 20 software using descriptive statistics and chi-square tests and presented as percentages and frequency counts.
4. Results
The frequency of six different hematologic malignancies was as follows: Non-Hodgkin's lymphoma 48% (n = 96), Hodgkin's lymphoma 14.5% (n = 29), acute myeloid leukemia (AML) 13% (n = 26), chronic lymphocytic leukemia (CLL) 11.5% (n = 23), acute lymphocytic leukemia (ALL) 8.5% (n = 17), chronic myeloid leukemia (CML) 4.5% (n = 9). Overall, non-Hodgkin's lymphoma was the most common malignancy in the studied population, and CML was detected at the lowest rate.
4.1. Demographics, Clinical Symptoms, and Paraclinical Signs
The patients' age range varied from 18 to 87 years (mean = 18.94 ± 49.85 years). The Hodgkin's lymphoma group had the youngest incidence age and the CLL group had the highest incidence age. Among patients, 60.5% were male (n = 121). For all six hematologic malignancies, a higher incidence was observed in men. Among clinical symptoms, cough (65.5%) and fever (61.5%) were the most prevalent, followed by dyspnea (36.5%). Among paraclinical criteria, anemia was the most common sign (75.5%), followed by thrombocytopenia (57%) (Table 2).
| Paraclinical Criteria | No. (%) |
|---|---|
| Anemia | 150 (75.5) |
| Thrombocytopenia | 114 (57) |
| Leukocytosis | 65(32.5) |
| Neutropenia | 64 (32) |
| Elevated D-dimer | 9 (4.5) |
4.2. Radiological Findings
Table 3 summarizes the radiological findings and their frequency in the study population.
Atelectasis, pleural effusion, mediastinal lymphadenopathy, and consolidation were the commonest radiological findings with descending order.
| Radiological Findings | No. (%) |
|---|---|
| Atelectasis | 98 (49) |
| Pleural effusion | 84 (42) |
| Mediastinal lymphadenopathy | 77 (38.5) |
| Consolidation | 74 (37) |
| Ground glass opacity (GGO) | 67 (33.5) |
| Pulmonary nodule | 44 (22) |
| Evidence of left heart disease | 39 (19.5) |
| Mosaic attenuation | 29 (14.5) |
| Interlobular septal thickening | 29 (14.5) |
| Pleural thickness | 28 (14) |
| Pulmonary hypertension | 25 (12.5) |
| peribronchial thickness | 19 (9.5) |
| Bronchial narrowing | 12 (6) |
| Cavity | 8 (4) |
| Tree in bud | 8 (4) |
| Halo sign | 6 (3) |
| Pulmonary mass | 5 (2.5) |
| Feeling defect in the pulmonary artery | 3 (1.5) |
4.3. Pulmonary Pathology Results
Table 4 summarizes different pulmonary pathologies and their incidences among study population.
| Pulmonary Pathologies a | No. (%) |
|---|---|
| Pneumonia | 83 (41.5) |
| Normal lung | 40 (20) |
| Small airway disease | 27 (13.5) |
| Mediastinal lymphadenopathy | 25 (12.5) |
| Chronic lung disease | 13 (6.5) |
| Intrapulmonary opacification not related to infection, hemorrhage or chemotherapy | 12 (6) |
| Uncertain diagnosis | 11 (5.5) |
| Pulmonary edema | 10 (5) |
| Perilymphatic opacities | 8 (4) |
| Pulmonary embolism | 4 (2) |
| Isolated pleural effusion | 4 (2) |
| Chemotherapeutic drug-induced pneumonitis | 3 (1.5) |
| Radiotherapy-induced pneumonitis | 3 (1.5) |
| Alveolar hemorrhage | 2 (1) |
a Considering the combination of clinical and paraclinical data, with the results of the CT scan
5. Discussion
Our results showed that non-Hodgkin's lymphoma is the most common malignancy among the study population, whereas CML was the most infrequent one. chronic lymphocytic leukemia, with a mean age of 63 - 91 years, affected mostly the elderly. Malignancies occurred more frequently in men. The most common radiological findings encountered were atelectasis, pleural effusion, mediastinal lymphadenopathy, consolidation, ground-glass opacities, and pulmonary nodules, respectively. Overall, nearly 80% of patients had pulmonary manifestations. Specific pulmonary manifestations (excluding small airway disease, isolated pleural effusion, chronic lung disease, unclear diagnosis, and normal cases) were observed in 66% of patients. Pneumonia was the most common complication observed in these patients. Less than a quarter of patients had no specific pulmonary pathology. By combining the results of CT scans with clinical and paraclinical symptoms, no correct diagnosis could be made in 5.5% of patients.
Compared with previous studies, we considered six types of hematologic malignancies simultaneously (because of the same nature of diseases and also similar treatment options), which provided a broader range of information. Most previous studies were conducted with only one type of hematologic malignancy; for example, Shahid Ahmad et al. conducted their study with patients with CLL only (12), Bugdaci et al. studied patients with AML (3) and Kosichkina et al. conducted research with a limited population of 44 patients with severe neutropenia (13). Shroff et al. presented leukemic involvement in the thorax and stated that lymphadenopathy was the most common manifestation among patients. In our study performed on leukemic patients in addition to people with lymphoma and multiple myeloma, we found that although lymphadenopathy was one of the most frequent findings, atelectasis was the most common (14). In another study performed by Burivong et al. on febrile neutropenic patients with hematologic malignancies, consolidation was the most common chest finding (15).
Consistent with the studies by Ahmad et al., Choi et al., and Bugdaci et al., pneumonia was the most common pulmonary manifestation in these patients (3, 4, 12). Calvillo Batllés et al. also found infection to be the most common cause of pulmonary involvement in patients with hematologic neoplasms (16). Nema et al. also showed that bacterial and fungal pneumonia were the main causes of lung lesions in patients with hematologic malignancies, whereas bacterial pneumonia and tuberculosis were the main causes in patients without hematologic malignancy (17).
In contrast to a study conducted by Bruno et al., on 124 neutropenic patients in the setting of hematologic malignancy, who reported an incidence of 32% for the development of a cavity in patients with aspergillosis and 55% for bacterial pneumonia, the incidence of cavity development in our study was much lower at 4% (18). Similar to the study conducted by Calvillo Batllés et al., spontaneous pneumothorax was also observed more frequently in Hodgkin's disease than in other hematologic malignancies in our study (16). In the study conducted by Kosichkina et al., the bacterial source was considered the most common cause of pneumonia, which was significantly associated with the GGO pattern (13).
In our study, the consolidation pattern was observed more frequently in the segmental form, which was more common in AML and non-Hodgkin's lymphoma, the lobular pattern with greater frequency in ALL and the lobar pattern with greater frequency in non-Hodgkin's lymphoma and CML. The distribution of consolidation was more often unilateral in all malignancies studies except CML. Similarly, the GGO pattern was more often reported as segmental, which was more common in AML and non-Hodgkin's lymphoma. In contrast to the type of distribution of consolidation, GGO was observed bilaterally in all hematologic malignancies, and only unilateral spread of GGO was predominantly observed in ALL.
In the study conducted by Nema et al. on patients with hematologic malignancies (17) bacterial and fungal types of pneumonia were considered the main cause of lung lesions. Considering the radiological patterns and laboratory tests such as sputum culture, Bacterial pneumonia with two lobar and bronchopneumonia patterns was the main cause of infectious lung opacity in our study, while atypical and fungal pneumonia were in second and third positions, respectively. The prevalence of pneumonia was highest in ALL, CLL, and AML (in descending order).
A limitation of our study was the lack of complete information on the paraclinical status of some participants, making more accurate diagnoses difficult. Burivong et all. have shown that despite the high sensitivity of the CT scan for the diagnosis of pulmonary infection in hematologic malignancies (91%), the specificity and positive predictive value are low (40% and 53%, respectively) (15), suggesting that we cannot rely solely on the results of CT to make a diagnosis. However, our main objective was to determine the frequency of CT findings. We suggest that future studies (with a larger population in each group), should be performed with more detailed para-clinical data for each patient to determine the diagnosis more accurately. Also, similar studies could be conducted, specifically in similar but critically ill patients who require treatment in the intensive care unit (ICU).
5.1. Conclusions
In conclusion, considering the increasing prevalence of malignancies in our population, and the relative importance of hematologic malignancies, accurate and rapid recognition of complications, especially pulmonary complications, which may that threaten a patients’ life with immunodeficiency, seems very important. As mentioned earlier, patients with hematologic malignancies have a high incidence of pulmonary complications in various forms. Confirming previous studies, this study proved that performing non-contrast thorax CT scans in patients with acute pulmonary symptoms, in combination with clinical and paraclinical information from the patient, can contribute to early diagnosis, determination of the severity of the disease, detection of infectious complications and may lead to reduced morbidity and mortality in such patients.