1. Background
Colon cancer is one of the most prevalent gastrointestinal malignancies worldwide and accounts for more than half of all common tumors with over 1 million new cases and 500,000 deaths annually (1, 2). Currently, surgery is the best treatment option for colon cancer, which includes various techniques such as conventional laparoscopic surgery, hand-assisted laparoscopic surgery, robotic surgery, single-pore laparoscopic surgery, and open surgery (3). In addition, colon cancer accounts for nearly 60% with approximately 106 180 new cases expected to be diagnosed in 2022 (4, 5).
Laparoscopic surgery has become the preferred procedure for the surgical management of various colon diseases. Several large randomized controlled trials have shown that laparoscopic surgery is effective and safe, with minimal invasiveness, better short-term outcomes, and improvement compared to open surgery, which should only be performed by experienced surgeons (6-8).
Laparoscopic surgery has advantages such as little blood loss and lower pain. However, prior studies have shown that laparoscopic surgery has some limitations, such as prolonged operative time and a longer learning curve for surgeons (9). Some publications have shown that laparoscopic surgery may be less expensive or more cost-effective than open surgery (10). Decreased mortality after laparoscopic surgery may be a direct result of decreased postoperative complications (11).
Lymph node status is considered the most powerful pathological predictor of patient outcome for accurate cancer staging and is an indicator of the quality of cancer care. Adequate lymph node staging (TNM) is crucial for predicting prognosis and planning better therapy. Removing and examining an adequate number of lymph nodes is important because more extensive node removal is associated with better survival rates and less recurrence (12). The quality of the surgical method plays a key role in obtaining an optimal number of lymph nodes (13), and a recent systematic review investigated whether the number of lymph nodes retrieved after colon resection is related to lifespan (14).
2. Objectives
The purpose of this study was to compare the number of lymph nodes removed and the outcomes of laparoscopic colon surgery to open colectomy in colon cancer.
3. Methods
This prospective study was conducted at the surgical department of Modares Hospital, Shahid Beheshti University of Medical Sciences in Tehran, between 2019 and 2021. A total of 120 patients with colon cancer, who required surgical treatment, were enrolled in our unit, comprising 57 females and 63 males. Of these, 78 patients underwent open surgery, while 42 patients underwent laparoscopic surgery. Patients were categorized into two groups based on their clinical conditions: laparoscopic surgery and open surgery.
Exclusion criteria for the study included patients outside the age range of 30 to 60 years, those with tumors located in the rectum, patients who underwent laparoscopic surgery initially but were changed to open surgery due to any reason, patients with multiple metastases and inoperable conditions at the beginning of surgery and during the initial abdominal examination.
The complete history of the patients was taken and recorded in the file. Patients were informed about the advantages and disadvantages of laparoscopic surgery and open surgery, and written informed consent was obtained from all patients.
A checklist containing 8 variables was prepared for all patients, which included postoperative pain, duration of hospitalization, infection of the operation site during the first 30 days, the number of lymph nodes removed in pathology, the rate of drop in hemoglobin, anastomotic leakage, urinary tract injury, and duration of surgery.
Patients were administered intravenous Cefazolin 1 gr and Metronidazole 500 mgr before surgery, and then every 12 hours until 24 to 72 hours after surgery, and longer if there was any sign of infection. Intravenous fluid treatment was continued until the liquid meal was covered.
The Foley catheter was removed as early as possible. Enrolled patients were managed postoperatively by the same surgeons' staff. A thorough follow-up was conducted after 1 month of surgery with a physical examination.
Data were analyzed, using SPSS software (version 21) and Mann-Whitney and independent t test. A significance level of P < 0.05 was considered statistically significant.
3.1. Surgical Technique
All surgeries in this study were performed by a surgical team with extensive experience in laparoscopic surgery, and the same team performed the open surgeries to ensure consistency. For open surgery, the patient was placed in the supine position and a midline incision was made for the colectomy according to standard surgical principles.
In laparoscopic surgery, the patient was placed in the supine and Trendelenburg position, and a pneumoperitoneum was created, using an open method. A 12 mm port was inserted in the umbilical region for the camera, and other trocars were placed by the surgical team based on the tumor location. For right colectomy and transversal surgery, the surgeon and camera operator stood on the patient's left side, while for left colectomy, they stood on the right side. An assistant was also present on the opposite side of the surgeon near the monitor, and the scrub colleague was positioned between the patient's legs. The anastomosis technique was performed, using a small incision of 2cm to 4cm outside with a stapler.
4. Results
From 2019 to 2021, 120 patients were included in this study, with 57 females and 63 males with colon cancer. Of these, 78 patients (64.7%) underwent open surgery and 42 patients (35.3%) underwent laparoscopic surgery (Table 1).
| Laparoscopic Group | Open Group | |
|---|---|---|
| Age, y (mean ± SD) | 49.21 ± 6.61 | 48.65 ± 6.71 |
| Sex | ||
| Male | 22 | 41 |
| Female | 20 | 37 |
The age of patients ranged from 30 to 60 years with a mean age of 48.8 ± 6.65 years (Table 1).
The mean operative time for laparoscopic surgery was significantly longer than that for open surgery (199.10 ± 21.99 minutes vs. 175.51 ± 17.77 minutes, P < 0.05).
Of the patients who underwent open surgery, 7 (8.97%) developed an infection, compared to 3 (7.1%) of those, who underwent laparoscopic surgery. However, there was no significant difference between the two groups (P = 0.7).
Anastomotic leak complication was seen in 5 (6.41%) patients, who underwent open surgery and 4 (9.5%) patients who underwent laparoscopic surgery. There was no significant difference between the two groups (P = 0.5).
The number of removed lymph nodes was 13.93 ± 3.6 for laparoscopic surgery and 16.3 ± 3.8 for open surgery, which was not statistically significant (P = 0.13).
Urinary tract injury was observed in 2 (2.56%) patients who underwent open surgery and zero patients who underwent laparoscopic surgery. However, this difference was not statistically significant (P = 0.02).
Severe postoperative pain was reported in 43 (55%) patients who underwent open surgery, compared to only 4 (9.5%) patients who underwent laparoscopic surgery. This finding was statistically significant (P < 0.05).
The decrease in hemoglobin levels after surgery, compared to preoperative levels, was greater in patients who underwent open surgery (2.45 ± 0.35) than those who underwent laparoscopic surgery (1.21 ± 0.14), which was statistically significant (P < 0.05).
The length of hospital stay was significantly longer for patients who underwent open surgery (15.14 ± 3.66 days) than for those who underwent laparoscopic surgery (11.64 ± 2.93 days) (P < 0.05) (Table 2).
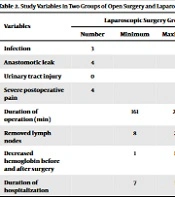
| Variables | Laparoscopic Surgery Group (N = 42) | Open Surgery Group (N = 78) | P-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Number | Minimum | Maximum | Mean ± SD | Number | Minimum | Maximum | Mean ± SD | ||
| Infection | 3 | 7 | 0.7 | ||||||
| Anastomotic leak | 4 | 5 | 0.5 | ||||||
| Urinary tract injury | 0 | 2 | 0.02 | ||||||
| Severe postoperative pain | 4 | 43 | 0.0 | ||||||
| Duration of operation (min) | 161 | 238 | 199.10 ± 21.99 | 143 | 206 | 175 ± 17.77 | 0.0 | ||
| Removed lymph nodes | 8 | 20 | 13.93 ± 3.65 | 9 | 22 | 16.13 ± 3.82 | 0.13 | ||
| Decreased hemoglobin before and after surgery | 1 | 1.5 | 1.21 ± 0.14 | 1.9 | 3.00 | 2.45 ± 0.35 | 0.0 | ||
| Duration of hospitalization | 7 | 16 | 11.64 ± 2.93 | 8 | 21 | 15.14 ± 3.66 | 0.0 | ||
5. Discussion
In this study, we aimed at comparing laparoscopic surgery and open surgery in treating colon cancer by examining the number of lymph nodes removed.
Our findings showed that although the average duration of laparoscopic surgery was longer than open surgery, which was statistically significant, it confirms the effectiveness of the surgical method in colon cancer on the duration of surgery. In the study by Song et al. in China in 2019, it was shown that the length of surgery in laparoscopic surgery is longer than in open surgery (1).
Laparoscopic surgery requires special equipment and experienced and skilled people; so, the more skillful the operating room staff and the surgeon are in preparing the equipment and performing the surgery, the shorter the operation time will be.
We also found that laparoscopic surgery had fewer common and unusual complications compared to open surgery, except for urinary and genital complications; no other significant complications were observed between the two groups in our study. A study by Numata et al. in 2018 showed that laparoscopic surgery for patients with severe disorders is safer and has fewer complications than open surgery (15).
Although relative prohibitions for laparoscopy are mentioned in surgical sources, it seems that this type of surgery can be performed in most patients.
Moreover, our study revealed that laparoscopic surgery was associated with a significantly less decrease in hemoglobin and shorter hospital stays compared to open surgery.
In the study of Neki et al. in 2017, the laparoscopic group had significantly less intraoperative bleeding, complications, and duration of postoperative hospitalization than the open-surgical group (16). A study by Yamaguchi et al. in 2017 showed that laparoscopic surgery for transverse and descending colon cancer is oncologically safe, and short-term outcomes such as bleeding, operative time, food intake, hospitalization, and postoperative complications are better than open surgery (17). Our study also confirms these findings. The study by Song et al. in 2019 in China (1) and the study by Ribeiro et al. in 2019 in Brazil (6) were similar to the results of our study.
Our study also showed that many short-term and long-term complications, such as urinary tract injury and anastomotic leak, and the rate of site infection were similar in both surgical groups.
Also, the number of lymph nodes removed in laparoscopic surgery was similar to open surgery, which confirms the safety of laparoscopic surgery against open surgery. In a study by Biondi et al. in 2013 in Italy, the results showed that laparoscopic surgery was as safe as open surgery, and early and late complications reported in both groups were similar (18). A study by Bedirli et al. in 2014 in Turkey showed that the results of open and laparoscopic surgery for colon cancer were similar and that laparoscopic surgery was a safe method for colon cancer (19). A study by Balducci et al. in 2017 showed that oncological safety for colon cancers can also be achieved by performing a laparoscopic approach, and long-term results can overlap with those of the open technique (20). These studies confirm our findings.
5.1. Strengths
In the laparoscopy group, the length of hospital stay was shorter compared to open surgery, which helps the patient return to work faster. Severe postoperative pain was less in the laparoscopic group than in the open surgery. The amount of hemoglobin drop in laparoscopic surgery was lower than in open surgery, but the duration of surgery in open surgery was less than in laparoscopic surgery. And the number of lymph nodes removed in open and laparoscopic surgery was not significantly different, which confirmed the safety of laparoscopic surgery in colon cancer.
5.2. Limitations
Although it has been tried to observe all the necessary things to conduct flawless research, some of the cases were beyond the reach and ability of the researcher. Among these cases are the lack of follow-up of patients in the future period, as well as the examination of the pathological stage of the disease, or the integration of the variables of the patient's operation status or patient and hospital costs. Another factor was the impossibility of prospective research.
5.3. Conclusions
Our study shows that laparoscopic surgery is associated with fewer short-term complications and has advantages such as shorter hospital stays, less severe postoperative pain, and a lower drop in hemoglobin. There was no significant difference in the number of lymph nodes removed in laparoscopic and open surgery, indicating the safety of laparoscopic surgery for colon cancer.