1. Introduction
Primary thyroid lymphoma is defined as a lymphoma (i.e malignant transformation of the lymph node) arising de novo from the thyroid gland. The invasion of the thyroid gland as a consequence of either metastasis or direct extension is excluded from this definition. Primary thyroid lymphomas are non-Hodgkin lymphomas (NHLs) in its pathological variant. Primary thyroid Hodgkin disease is extremely rare condition (1).
Chronic lymphocytic leukaemia (CLL) is a low-grade neoplasm composed of small, mature B lymphocytes in the peripheral blood, bone marrow, lymph nodes, and other tissues (2, 3). Secondary Lymphomas occur due to the extension of cells from other systemic diseases which is quite rare. The prevalence of CLL involving the thyroid is extremely low, accounting for about 3% to 4% of all thyroid lymphoproliferative neoplasms (4-7).
Here we reported a case of CLL, which presented initially as a thyroid swelling which later on, it lead to the final diagnosis of secondary thyroid lymphoma due to CLL. Very minimal cases have been reported in the literature and this is a first-ever reported case in the Indian Subcontinent where CLL is rare.
2. Case Presentation
A 55-year- old female presented to the General Surgery Department of our institution with swelling over the anterior part of the neck for one month, along with complaints of general weakness, fatigue, dizziness for the past one week. The swelling in the anterior part of the neck was initially small but has gradually progressed to the current size of 4 × 3 cm. In addition, she reported palpitations, weight loss, intermittent episodes of fever. However, there were no reported history or symptoms related to primary or secondary thyrotoxicosis.
On examination, the patient appeared pale and had a solitary oval swelling in the front of the neck (Figures 1 and 2), moving with deglutition but not with protrusion of tongue. It extended from 2 cm below the midline of the hyoid bone to 2 cm above the sternal notch, with lateral margins 2 cm from the midline. The consistency of the swelling was firm to hard, and there was no evidence of r retrosternal extension and also enlargement of the parotid gland was observed (Figure 3). Level II and III cervical nodes were clinically palpable.
The routine Hemogram revealed a hemoglobin level of 7.8 g/dL and WBC count of 3.31 × 103/μL (3). The patient's thyroid function test results showed that she was in a euthyroid state (T3 levels at 1.13 nmol/L, T4 levels at 7.96 μg/dL, and TSH levels at 3.21 μIU/mL). Based on these findings, suspicion of carcinoma was kept and the patient underwent further to invasive investigations as given below.
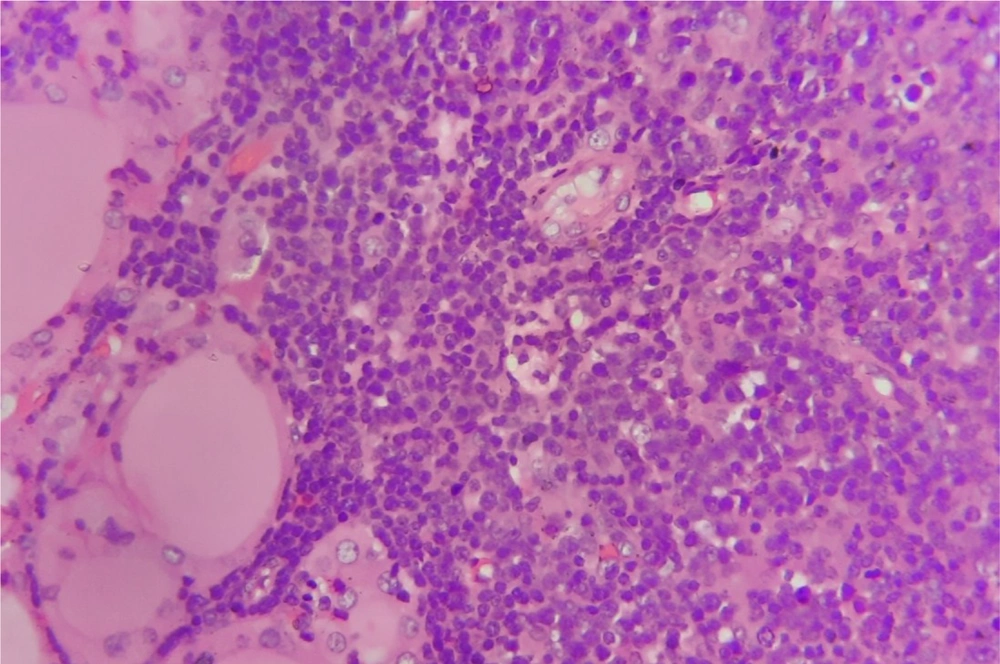
Fine needle aspiration cytology of the thyroid swelling was performed and the results indicated Bethesda category II lymphocytic thyroiditis, suggesting a core needle biopsy (Figure 4) to confirm Hashimoto's thyroiditis. However, Anti Thyroid Antibodies were negative. Two weeks later, the patient reported multiple swellings over the axillary, cervical, and inguinal region. Abdominal examination revealed splenomegaly and hepatomegaly. Fine needle aspiration cytology of the lymph nodes revealed a monomorphic cluster of Lymphocytes. Based on these findings, the patient was diagnosed with chronic lymphocytic leukemia (CLL). The CLL was graded as Stage IV according to the Rai-Sawitsky classification and Stage C according to the Binet classification. The final diagnosis was CLL with secondary thyroid lymphoma was confirmed.
Based on the oncologist's recommendation, the patient underwent three cycles of chemotherapy (Bendamustine 100mg IV) achieving a positive response and stable disease during the initial 6-month follow-up. However, at 16 months, the patient developed alarming symptoms of breathlessness and restlessness, leading to the initiation of the CHOP regime. Tragically, the patient's condition deteriorated, and she succumbed to febrile neutropenia. On examination, the vital signs were as follow: Heart rate (HR) of 82 bpm, blood pressure (BP) of 120/70 mm Hg, and oxygen saturation (SPo2) of 92% at room air. During the local examination, it was observed that the thyroid nodule did not show any change in size. However, there was a concerning development of satellite nodules all over the body (Figure 5).
3. Discussion
Thyroid Lymphomas represent very rare cause of thyroid swellings, typically associated with non-hodgkin B-cell lymphomas and Hashimoto’s thyroiditis. These cases are commonly observed in individuals in their 5th to 6th decades of life. The exact pathogenesis remain unclear, but they are considered to be a form of MALT-oma’s. unlike other thyroid malignancies, thyroid lymphomas show a favorable response to Chemotherapy (8).
Chronic Lymphocytic leukemia CLL is a neoplastic lymphoproliferative disorder, which is more prevalent in the western population and its typically diagnosed in the individual. Additionally, CLL is more commonly observed in males than females. The patients with CLL typically present with symptoms such as fatigue, weakness, and multiple swellings over the body accompanied by night sweats. The diagnosis of CLL is usually performed if lymphocyte count exceeds 5 × 109/L persistently for at least 3 months. Peripheral smear study revealed that the leukemic cells found in the peripheral blood smear are characteristically small, mature lymphocytes with a very narrow border of cytoplasm and a dense nucleus lacking discernible nucleoli. These cells exhibit partially aggregated chromatin, leading to the characteristic appearance of smudge cells (9).
In the case of the secondary thyroid lymphomas, the FNAB picture may often resemble that of Hashimoto’s thyroiditis, posing challenge in the accurate diagnosis of this condition (1). To enhance diagnostic accuracy, additional use of Flowcytometry (CD5, CD19) and gallium scintigraphy can be helpful. These supplementary diagnostic tools aid in distinguishing secondary thyroid lymphomas from other thyroid disorders, enabling the development of treatment guidelines for optimal management (8).
In developed countries, the treatment for these conditions usually involves medical management trough chemotherapy with the bendamustine- alemtuzumab regimen with allogenic stem cell transplantation. In our case, the patient received three cycles of bendamustine. Surgical intervention is generally limited to incisional biopsy, and in emergency situations, pretracheal tumor debulking may be considered (10).
In our case, the rarity begins with the ethnicity, as the patient is of Asian descent, and the fact that she is female adds to the uniqueness. The rarest feature is the thyroid swelling being the first presenting symptom, followed by the development of splenomegaly, hepatomegaly, and lymphadenopathy. Achieving an accurate diagnosis pre-operatively is crucial in such cases as it could avoid unwarranted surgeries when it is not indicated in the treatment protocol.
Thyroid lymphomas are an exceedingly rare group of lymphomas accounting for only 3 - 4% of all thyroid swellings. Considering it as one of the potential diagnoses requires a high level of suspicion, especially in cases with a a background of other systemic diseases, such as chronic lymphocytic lymphoma. Accurate pre-operative diagnosis is crucial as unnecessary surgeries could exacerbate the disease's progression instead of providing the intended benefit. Therefore, early and precise diagnosis is essential to guide appropriate treatment decisions and improve patient outcomes.