1. Background
In adults, kidney cancer encompasses malignant tumors that originate from the parenchyma and pelvis. Renal cell carcinoma (RCC) is the most prevalent type of kidney tumor, accounting for over 80% of all kidney tumors. In pediatric cases, the most common type of kidney cancer is nephroblastoma (Wilms tumor), comprising 1% of all kidney cancers (1). Worldwide, renal cell carcinoma (RCC) ranks sixth among men and tenth among women, accounting for 5% and 3% of all malignancies, respectively (2). Renal cell carcinoma incidence rates have been on the rise globally. Kidney cancer is prevalent in western countries, whereas its incidence rate is lower in African and Asian countries (3). Renal cell carcinoma is considered as the most lethal urogenital cancer with a fatality rate of 30 to 40% (4). Despite the increasing incidence of renal cell carcinoma, survival has improved considerably due to the popularity of treatment methods such as active surveillance, robot-assisted nephron - sparing surgical procedures, and minimally invasive techniques, such as thermal ablation (5).
Dissimilarities in kidney cancer incidence and mortality rates in different parts of the world could point to the role of risk factors and genetic variations in the development of this cancer. The most important risk factors of RCC are age and gender and other potential risk factors for kidney cancer include lifestyle factors, comorbidities, medications, and environmental factors (6).
2. Objectives
Investigating the incidence trend of kidney cancer can be a guide to controlling the condition of this disease in the coming years. In this study, we intend to investigate the incidence trend of kidney cancer between 2003 and 2016 in Iran and its 31 provinces to determine the possible changes in national and subnational levels.
3. Methods
In order to carry out this study, we utilized the most recent national and subnational data on confirmed cases of kidney cancer obtained from Iran's national cancer registry system. This registry system was initiated by the Iran Ministry of Health in 2000, and it gathers software - based data from all pathology centers, covering 100% of the country's provinces (7) and has been developed since 2014 by collecting clinical, paraclinical, and mortality data nationwide (8). In this registry system, cancer types are coded using the International Classification of Diseases for Oncology, third edition (ICD-O-3) (9), and the topography of cancers is detected according to the International Classification of Diseases, 10th edition (ICD-10) that introduced kidney cancer as C64, malignant neoplasm of kidney (10). The incident cases were obtained from an Excel file provided by the Iran Ministry of Health and Medical Education. This study calculated and reported the results for the entire country and its provinces, presenting the crude number of cases and the age-standardized incidence rate (ASIRs) per 100,000 people per year for both sexes in each province from 2003 to 2016.To calculate the Age-Standardized Incidence Rates (ASIRs), we obtained the entire population of Iran (both sexes) and the population of each province (both sexes) from the Iran Statistics Center. This center conducts and reports a population census every 5 years (11). Due to the lack of population estimates in the interval years, we used the population of the nearest year for calculating the rates.
We computed the ASIRs directly based on the World Health Organization's (WHO) standard population using SPSS software version 19. The WHO has developed a new standard population to facilitate the comparability of incidence rates in different societies (12).
4. Results
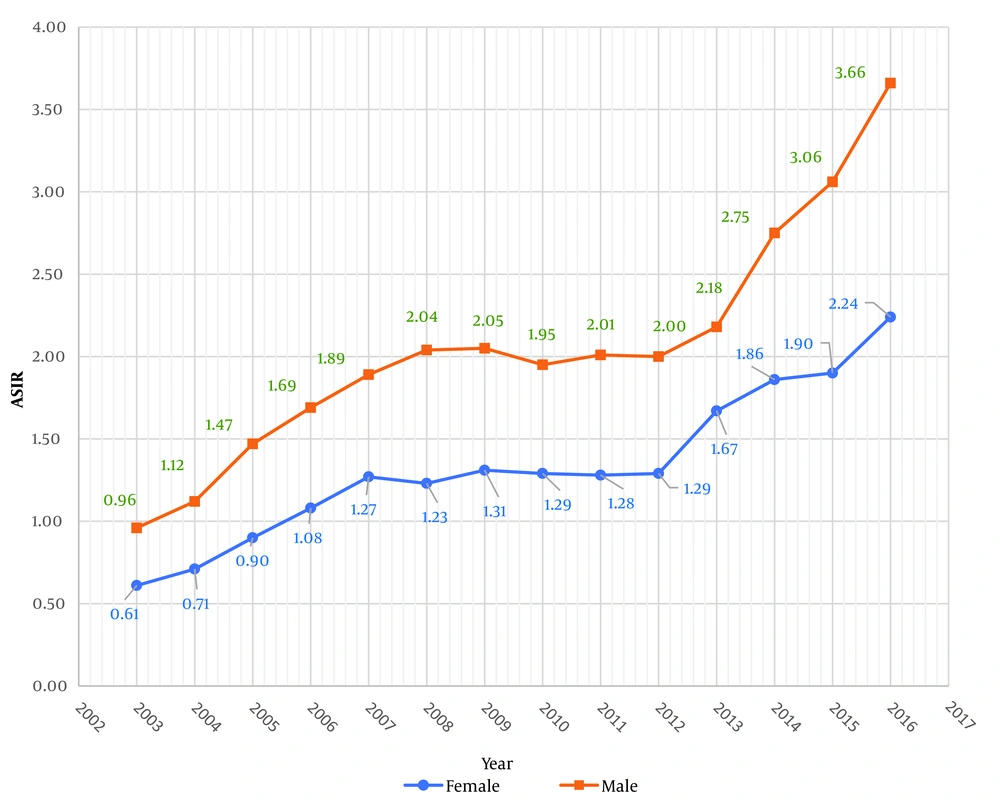
The study revealed a rising trend in the incidence of kidney cancer over the years. The ASIR of kidney cancer in men increased from 0.96 in 2003 to 3.66 in 2016 in Iran. Although the ASIR of kidney cancer in women was lower compared to men, it exhibited a similar increasing trend, rising from 0.61 in 2003 to 2.24 in 2016 (Figure 1).
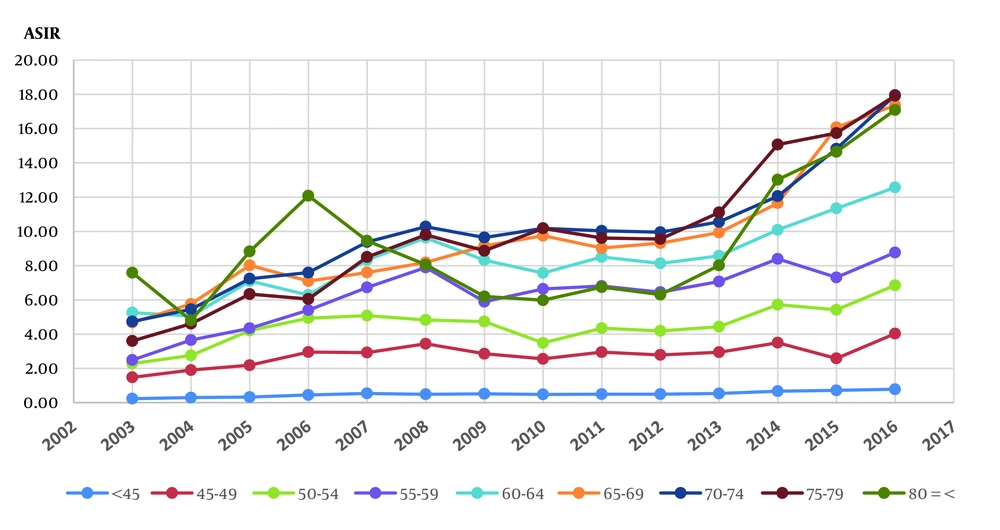
In 2016, the lowest Age - Standardized Incidence Rates (ASIRs) of kidney cancer were observed in the age group below 45 years, with rates of 0.89 per 100,000 in men and 0.68 per 100,000 in women. The highest ASIR in men was found in the age group of 75 to 79 years (25.31 per 100,000), while in women, it was in the age group of 80 years and above (12.34 per 100,000). Table 1 illustrates the ASIRs per 100,000 of kidney cancer with a 95% confidence interval (CI) based on age groups during the study years in Iran. The CI was calculated using the method described by Keyfitz in 1996 (13). Additionally, Figure 2 showcases the nationwide changes in ASIRs of kidney cancer from 2003 to 2016 across different age groups.
| Year | Age | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| < 45 | 45 - 49 | 50 - 54 | 55 - 59 | 60 - 64 | 65 - 69 | 70 - 74 | 74 - 79 | 80 + | |
| 2003 | 0.23248 (0.23242 - 0.23254) | 1.4761 (1.4746 - 1.4776) | 2.2864 (2.2837 - 2.2891) | 2.4894 (2.4859 - 2.4930) | 5.2579 (5.2494 - 5.2665) | 4.6762 (4.6678 - 4.6846) | 4.7350 (4.7262 - 4.7438) | 3.6016 (3.5932 - 3.6101) | 7.5898 (7.5713 - 7.6083) |
| 2004 | 0.2954 (0.2953 - 0.2955) | 1.9019 (1.8999 - 1.9039) | 2.7582 (2.7549 - 2.7615) | 3.6547 (3.6495 - 3.6599) | 5.0531 (5.0449 - 5.0613) | 5.76177 (5.7514 - 5.7721) | 5.4497 (5.4397 - 5.4598) | 4.6101 (4.5993 - 4.6210) | 4.8017 (4.7900 - 4.8134)) |
| 2005 | 0.3234 (0.3233 - 0.3235) | 2.1858 (2.1835 - 2.1881) | 4.2099 (4.3371 - 4.3495) | 4.3433 (4.3371 - 4.3495) | 7.1016 (7.0901 - 7.1131) | 8.0164 (8.0020 - 8.0307) | 7.2365 (7.2231 - 7.2499) | 6.3389 (6.3240 - 6.3539) | 8.8290 (8.8074 - 8.8505) |
| 2006 | 0.4475 (0.4474 - 0.4476) | 2.9522 (2.9491 - 2.9553) | 4.9357 (4.9299 - 4.9416) | 5.4026 (5.3949 - 5.4103) | 6.2822 (6.2720 - 6.2924) | 7.0978 (7.0851 - 7.1105) | 7.5939 (7.5798 - 7.6080) | 6.0508 (6.0366 - 6.0650) | 12.0818 (12.0523 - 12.1112) |
| 2007 | 0.5384 (0.5382 - 0.5385) | 2.9238 (2.9208 - 2.9269) | 5.0809 (5.0749 - 5.0869) | 6.7268 (6.7172 - 6.7364) | 8.3308 (8.3173 - 8.3443) | 7.5988 (7.5852 - 7.6125) | 9.3807 (9.3633 - 9.3981) | 8.5000 (8.4800 - 8.5200) | 9.4486 (9.4260 - 9.4716) |
| 2008 | 0.4894 (0.4893 - 0.4895) | 3.4348 (3.4312 - 3.4384) | 4.8269 (4.8212 - 4.8325) | 7.8920 (7.8808 - 7.9033) | 9.6282 (9.6126 - 9.6438) | 8.1834 (8.1687 - 8.1980) | 10.27414 (10.2551 - 0.2931) | 9.7965 (9.7735 - 9.8196) | 8.0545 (8.0349 - 8.0742) |
| 2009 | 0.5161 (0.5160 - 0.5163) | 2.8533 (2.8505 - 2.8560) | 4.7344 (4.729 - 4.7393) | 5.8953 (5.8882 - 5.9023) | 8.3203 (8.3084 - 8.3323) | 9.1536 (9.1381 - 9.1691) | 9.6431 (9.6253 - 9.6610) | 8.8667 (8.8485 - 8.8849) | 6.1988 (6.1861 - 6.2114) |
| 2010 | 0.4787 (0.4785 - 0.4788) | 2.5555 (2.5530 - 2.5580) | 3.4870 (3.4833 - 3.4906) | 6.6415 (6.6335 - 6.6494) | 7.5688 (7.5579 - 7.5797) | 9.7490 (9.7325 - 9.7655) | 10.1789 (10.1600 - 0.1977) | 10.1803 (10.1594 - 0.2012) | 5.9813 (5.9690 - 5.9935) |
| 2011 | 0.4906 (0.4905 - 0.4907) | 2.8036 (2.8009 - 2.8064) | 3.9973 (3.9931 - 4.0014) | 6.0321 (6.0248 - 6.0393) | 7.8193 (7.8081 - 7.8305) | 8.7319 (8.7171 - 8.7467) | 10.0300 (10.0115 - 10.0486) | 8.8302 (8.8121 - 8.8483) | 5.9450 (5.9329 - 5.9572) |
| 2012 | 0.4916 (0.4915 - 0.4918) | 2.6452 (2.6427 - 2.6478) | 3.9654 (3.9613 - 3.9695) | 5.8494 (5.8426 - 5.8562) | 7.4392 (7.4289 - 7.4496) | 8.9306 (8.9157 - 8.9454) | 10.0310 (10.0124 - 10.0497) | 9.5596 (9.5397 - 9.5794) | 6.0255 (6.0132 - 6.0378) |
| 2013 | 0.5490 (0.5489 - 0.5492) | 2.9302 (2.9274 - 2.9329) | 4.5076 (4.5030 - 4.5122) | 6.5882 (6.5807 - 6.5957) | 8.2168 (8.2057 - 8.2279) | 9.6486 (9.6329 - 9.6644) | 10.7723 (10.7522 - 10.7924) | 11.2857 (11.2619 - 1.3093) | 8.3052 (8.2882 - 8.3221) |
| 2014 | 0.6704 (0.6703 - 0.6706) | 3.4971 (3.4939 - 3.5003) | 5.7196 (5.7138 - 5.7254) | 8.3943 (8.3850 - 8.4036) | 10.0893 (10.0761 - 0.1025) | 11.6479 (11.6293 - 11.6665) | 12.0580 (12.0355 - 12.0805) | 15.0701 (15.0382 - 5.1020) | 13.0197 (12.9930 - 13.0464) |
| 2015 | 0.7168 (0.7166 - 0.7170) | 2.5805 (2.5782 - 2.5828) | 5.4209 (5.4155 - 5.4263) | 7.3126 (7.3047 - 7.3205) | 11.3445 (11.3301 - 1.3590) | 16.0703 (16.0454 - 16.0953) | 14.8248 (14.7973 - 14.8523) | 15.7396 (15.7061 - 15.7732) | 14.6476 (14.6175 - 14.6777) |
| 2016 | 0.7828 (0.7826 - 0.7830) | 4.0298 (4.026 - 4.033) | 6.8511 (6.8443 - 6.8578) | 8.7647 (8.7554 - 8.7740) | 12.5644 (12.5489 - 12.5799) | 17.3681 (17.3419 - 17.3943) | 17.9577 (17.9247 - 17.9908) | 17.9211 (17.8828 - 17.9595) | 17.0921 (17.0568 - 17.1274) |
Age-standardized Incidence Rate (ASIRs) per 100,000, 95% CI of Kidney Cancer According to Age Groups and Year in Iran from 2003 to 2016 a
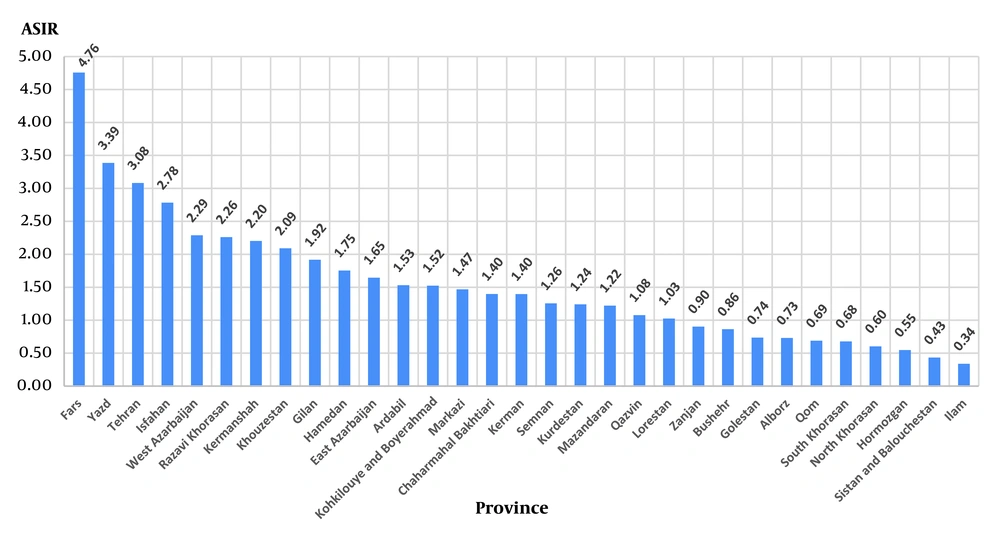
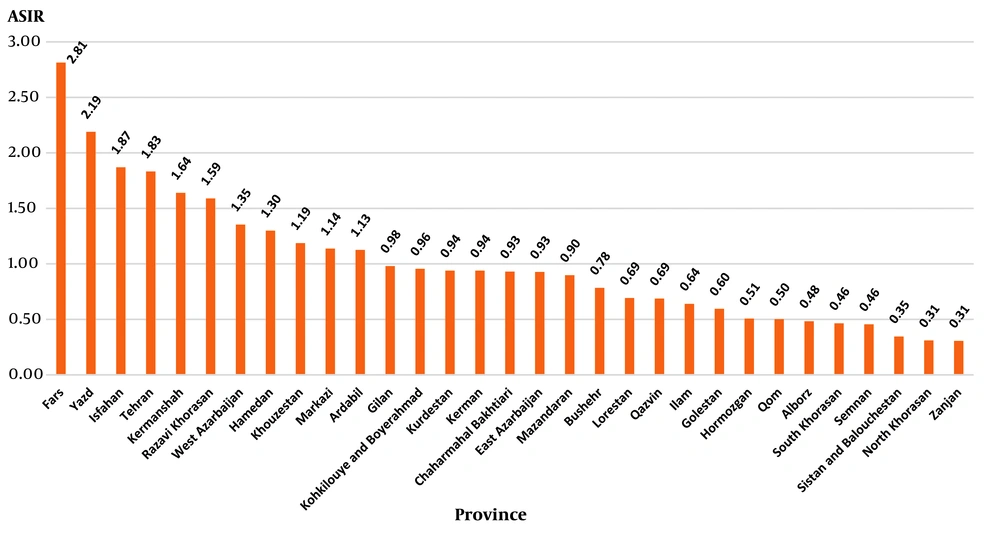
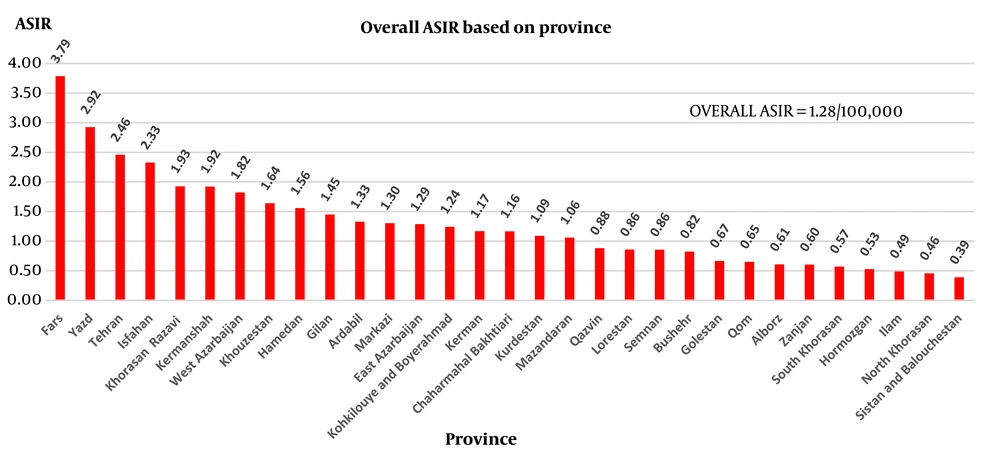
Table 2 shows the number of incident cases and ASIR of kidney cancer in all provinces in both genders during the study period. The average of ASIRs of male patients with kidney cancer from 2033 to 2016 in different provinces showed that Fars and Yazd occupied the first and second ranks of kidney cancer incidence in Iranian males, respectively while Ilam and Sistan and Balouchestan had the lowest related rates (Figure 3). Additionally, a comparison of ASIRs of women with kidney cancer in different provinces showed that Fars and Yazd had the highest ASIRs. In contrast, North Korasan and Zanjan had the lowest ASIRs (Figure 4). Nationwide ASIRs of kidney cancer was 1.28 per 100,000 and ASIRs of kidney cancer for each province from 2003 to 2016 are illustrated in Figure 5.
| Province | Year | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
| Ardabil | ||||||||||||||
| Male | 0.97 (6) | 0.00 (0) | 1.13 (7) | 0.65 (4) | 1.15 (7) | 3.08 (19) | 1.42 (9) | 1.42 (9) | 1.97 (13) | 1.60 (10) | 1.71 (11) | 1.56 (10) | 1.70 (11) | 3.07 (20) |
| Female | 0.00 (0) | 0.00 (0) | 0.33 (2) | 0.98 (6) | 1.13 (7) | 0.82 (5) | 2.43 (15) | 0.81 (5) | 1.35 (8) | 1.53 (9) | 1.38 (7) | 1.27 (8) | 0.78 (5) | 2.95 (19) |
| Isfahan | ||||||||||||||
| Male | 0.90 (21) | 2.61 (61) | 2.83 (66) | 3.47 (81) | 2.23 (52) | 2.10 (49) | 2.83 (70) | 1.82 (45) | 2.25 (55) | 2.30 (57) | 2.70 (62) | 3.55 (90) | 4.65 (119) | 4.73 (122) |
| Female | 0.40 (9) | 1.44 (32) | 1.89 (42) | 2.20 (49) | 1.74 (39) | 1.21 (27) | 1.83 (44) | 2.08 (50) | 1.71 (40) | 1.87 (45) | 1.95 (48) | 2.27 (56) | 2.29 (57) | 3.30 (83) |
| Alborz | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 1.72 (21) | 0.74 (9) | 0.82 (10) | 1.09 (13) | 0.88 (11) | 1.10 (13) | 1.32 (17) | 0.76 (10) | 1.80 (24) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.50 (6) | 1.01 (12) | 0.59 (7) | 0.70 (8) | 0.77 (9) | 0.78 (9) | 0.87 (11) | 0.55 (7) | 0.99 (13) |
| Ilam | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 1.08 (3) | 0.43 (1) | 0.00 (0) | 0.35 (1) | 0.26 (1) | 0.20 (1) | 0.38 (1) | 0.69 (2) | 0.00 (0) | 1.35 (4) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 1.12 (3) | 0.75 (2) | 0.00 (0) | 1.09 (3) | 0.73 (2) | 0.73 (2) | 0.72 (2) | 0.70 (2) | 2.09 (6) | 1.02 (3) |
| East Azarbaijan | ||||||||||||||
| Male | 0.16 (3) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 2.17 (40) | 1.36 (25) | 2.5 (47) | 1.75 (33) | 1.87 (35) | 2.04 (38) | 2.02 (37) | 2.14 (41) | 2.49 (48) | 4.54 (88) |
| Female | 0.06 (1) | 0.00 (00 | 0.17 (3) | 0.00 (0) | 0.91 (16) | 1.25 (22) | 1.09 (20) | 0.60 (11) | 0.98 (17) | 0.89 (160 | 1.06 (18) | 1.32 (250 | 2.10 (40) | 2.55 (49) |
| West Azarbaijan | ||||||||||||||
| Male | 1.44 (21) | 1.92 (28) | 2.06 (30) | 1.78 (26) | 1.85 (27) | 1.51 (22) | 1.67 (26) | 1.80 (28) | 1.66 (25) | 1.71 (26) | 2.07 (31) | 2.85 (46) | 5.67 (76) | 4.05 (67) |
| Female | 0.64 (9) | 1.13 (16) | 0.85 (12) | 1.06 (15) | 1.34 (19) | 1.41 (20) | 1.38 (21) | 1.05 (16) | 1.28 (19) | 1.24 (18) | 1.72 (24) | 2.65 (42) | 1.74 (28) | 1.47 (24) |
| Bushehr | ||||||||||||||
| Male | 0.21 (1) | 0.00 (0) | 0.43 (2) | 0.43 (2) | 1.92 (9) | 1.07 (5) | 1.07 (6) | 1.78 (100 | 1.31 (7) | 1.39 (8) | 1.01 (6) | 0.33 (2) | 0.82 (5) | 0.32 (2) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.24 (1) | 0.96 (4) | 1.43 (6) | 1.48 (7) | 0.42 (2) | 1.11 (5) | 1.00 (4) | 1.13 (5) | 1.27 (8) | 0.97 (5) | 0.96 (5) |
| Tehran | ||||||||||||||
| Male | 1.04 (72) | 1.07 (74) | 1.45 (100) | 1.45 (100) | 1.52 (105) | 2.93 (202) | 3.33 (204) | 2.78 (170) | 3.01 (192) | 3.04 (189) | 3.83 (224) | 5.44 (344) | 5.02 (321) | 7.25 (468) |
| Female | 0.66 (43) | 0.64 (42) | 0.83 (54) | 0.77 (50) | 0.95 (62) | 1.73 (113) | 1.99 (1200 | 1.84 (111) | 1.85 (114) | 1.89 (115) | 2.40 (139) | 3.44 (214) | 2.72 (171) | 3.94 (250) |
| Chaharmahal Bakhtiari | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 4.17 (18) | 2.32 (10) | 2.22 (10) | 1.11 (5) | 1.88 (8) | 1.74 (7) | 2.07 (9) | 2.58 (12) | 1.49 (8) | 0.00 (0) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 1.64 (7) | 1.88 (8) | 2.25 (10) | 1.13 (5) | 1.75 (8) | 1.71 (7) | 1.37 (5) | 0.65 (3) | 0.65 (3) | 0.00 (0) |
| South Khorasan | ||||||||||||||
| Male | 0.00 (0) | 0.93 (3) | 0.31 (1) | 1.24 (4) | 0.00 (0) | 0.93 (3) | 0.00 (0) | 0.90 (3) | 0.61 (2) | 0.50 (1) | 0.72 (3) | 1.05 (4) | 1.03 (4) | 1.27 (5) |
| Female | 0.00 (0) | 0.64 (2) | 0.32 (1) | 0.32 (1) | 0.32 (1) | 0.32 (1) | 0.00 (0) | 1.22 (4) | 0.51 (2) | 0.58 (2) | 0.45 (1) | 0.26 (1) | 0.79 (3) | 0.77 (3) |
| Khorasan Razavi | ||||||||||||||
| Male | 1.14 (32) | 1.35 (38) | 1.67 (47) | 1.49 (42) | 2.14 (60) | 1.71 (48) | 2.10 (63) | 2.33 (70) | 2.05 (60) | 2.16 (64) | 2.64 (78) | 3.70 (116) | 3.46 (110) | 3.72 (120) |
| Female | 0.75 (21) | 1.01 (28) | 1.11 (31) | 1.47 (41) | 1.40 (39) | 1.27 (390 | 1.30 (390 | 1.60 (48) | 1.39 (42) | 1.43 (430 | 1.83 (54) | 2.68 (84) | 2.43 (77) | 2.58 (83) |
| North Khorasan | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.25 (1) | 1.22 (5) | 0.93 (4) | 1.16 (5) | 1.10 (5) | 1.06 (4) | 0.95 (4) | 0.67 (3) | 0.44 (2) | 0.66 (3) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.49 (2) | 0.00 (0) | 0.46 (2) | 0.46 (2) | 0.31 (1) | 0.41 (2) | 0.46 (2) | 0.66 (3) | 0.44 (2) | 0.65 (3) |
| Khouzestan | ||||||||||||||
| Male | 0.733 | 1.10 (24) | 1.42 (31) | 1.74 (38) | 1.97 (43) | 3.07 (67) | 1.84 (42) | 2.14 (49) | 2.35 (53) | 2.11 (48) | 2.26 (51) | 2.31 (55) | 2.91 (70) | 3.32 (81) |
| Female | 0.772 | 0.29 (6) | 0.96 (20) | 0.96 (20) | 1.00 (21) | 1.77 (37) | 0.71 (16) | 1.25 (28) | 1.24 (27) | 1.07 (24) | 1.27 (28) | 1.49 (35) | 1.89 (45) | 1.95 (47) |
| Zanjan | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 1.45 (7) | 1.77 (9) | 0.98 (5) | 1.40 (7) | 1.38 (7) | 1.50 (8) | 1.71 (9) | 0.57 (3) | 1.88 (10) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.83 (4) | 0.21 (1) | 0.59 (3) | 0.20 (1) | 0.33 (2) | 0.37 (2) | 0.43 (2) | 0.57 (3) | 0.38 (2) | 0.37 (2) |
| Semnan | ||||||||||||||
| Male | 0.33 (1) | 0.33 | 0.66 (2) | 0.33 (1) | 0.66 (2) | 3.64 (11) | 1.26 (4) | 1.89 (6) | 2.26 (7) | 1.80 (6) | 1.85 (6) | 1.49 (5) | 0.59 (2) | 0.49 (2) |
| Female | 0.35 (1) | 0.00 (0) | 0.35 (1) | 0.35 (1) | 0.70 (2) | 0.70 (2) | 0.32 (1) | 0.32 (1) | 0.45 (1) | 0.36 (1) | 0.37 (1) | 0.31 (1) | 0.60 (2) | 1.19 (4) |
| Sistan and Balouchestan | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.25 (3) | 0.33 (4) | 0.33 (4) | 0.82 (10) | 0.71 (9) | 0.71 (9) | 0.75 (9) | 0.72 (9) | 0.59 (8) | 0.29 (4) | 0.22 (3) | 0.35 (5) |
| Female | 0.00 (0) | 0.17 (0) | 0.25 (3) | 0.25 (3) | 0.51 (6) | 0.25 (3) | 0.24 (3) | 0.95 (12) | 0.48 (6) | 0.56 (7) | 0.40 (6) | 0.15 (2) | 0.14 (2) | 0.49 (7) |
| Fars | ||||||||||||||
| Male | 3.76 (83 | 4.49 (99 | 7.26 (160 | 8.48 (187 | 6.35 (140 | 2.45 (54 | 2.59 (60 | 3.72 (86 | 2.92 (67 | 3.08 (71 | 3.76 (87 | 5.29 (126 | 6.89 (166 | 5.55 (135 |
| Female | 2.81 (60) | 3.47 (74) | 4.17 (89) | 5.02 (107) | 4.08 (87) | 1.55 (33) | 1.67 (38) | 1.58 (36) | 1.60 (36) | 1.62 (37) | 1.90 (42) | 2.47 (58) | 3.49 (83) | 3.96 (95) |
| Qazvin | ||||||||||||||
| Male | 0.69 (4) | 0.69 (4) | 0.34 (2) | 0.69 (4) | 1.37 (8) | 1.03 (6) | 1.31 (8) | 0.98 (6) | 1.11 (7) | 1.13 (7) | 1.21 (8) | 1.39 (8) | 1.58 (10) | 1.56 (10) |
| Female | 0.18 (1) | 0.00 (0) | 0.36 (2) | 0.36 (2) | 0.89 (5) | 0.36 (2) | 1.18 (7) | 0.68 (4) | 0.74 (4) | 0.87 (5) | 0.92 (5) | 1.15 (7) | 0.65 (4) | 1.28 (8) |
| Qom | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 1.30 (7) | 2.24 (12) | 1.19 (7) | 1.02 (6) | 1.11 (8) | 1.11 (7) | 0.74 (5) | 0.00 (0) | 0.00 (0) | 2.49 (16) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.39 (2) | 0.78 (4) | 1.24 (7) | 0.06 (6) | 0.69 (6) | 0.66 (6) | 0.45 (4) | 0.00 (0) | 0.17 (1) | 2.59 (16) |
| Kurdestan | ||||||||||||||
| Male | 0.14 (1) | 0.14 (1) | 0.55 (4) | 0.82 (6) | 1.23 (9) | 2.33 (17) | 1.73 (13) | 1.86 (14) | 1.97 (15) | 1.85 (14) | 1.50 (12) | 0.66 (5) | 0.91 (7) | 1.69 (13) |
| Female | 0.28 (2) | 0.00 (0) | 0.56 (4) | 1.41 (10) | 1.27 (9) | 1.41 (10) | 1.62 (12) | 0.94 (7) | 1.32 (10) | 1.29 (9) | 1.09 (7) | 0.66 (5) | 1.17 (9) | 0.13 (1) |
| Kerman | ||||||||||||||
| Male | 0.89 (12) | 0.89 (12) | 1.33 (18) | 2.07 (28) | 0.81 (11) | 0.96 (13) | 1.62 (24) | 1.69 (25) | 1.42 (21) | 1.58 (23) | 1.45 (22) | 1.36 (21) | 1.79 (28) | 1.70 (27) |
| Female | 0.62 (8) | 0.69 (9) | 0.39 (5) | 0.54 (7) | 0.62 (8) | 0.77 (10) | 1.51 (22) | 1.10 (16) | 1.13 (16) | 1.25 (180 | 1.16 (170 | 1.12 (17) | 1.29 (20) | 0.95 (15) |
| Kermanshah | ||||||||||||||
| Male | 1.88 (18) | 1.57 (15) | 0.84 (8) | 1.78 (17) | 2.61 (25) | 1.78 (17) | 2.75 (27) | 1.83 (18) | 2.12 (20) | 2.23 (21) | 2.36 (22) | 2.73 (27) | 2.72 (27) | 3.63 (36) |
| Female | 0.65 (6) | 1.19 (11) | 0.65 (6) | 0.98 (9) | 1.80 (18) | 1.60 (16) | 1.66 (16) | 2.49 (24) | 1.92 (19) | 2.02 (20) | 1.92 (19) | 1.83 (18) | 2.64 (26) | 1.61 (16) |
| Kohkilouye and Boyerahmad | ||||||||||||||
| Male | 0.62 (2) | 0.31 (1) | 0.00 (0) | 0.93 (3) | 4.05 (13) | 1.25 (4) | 1.85 (6) | 2.74 (9) | 1.95 (6) | 2.18 (7) | 2.05 (7) | 2.02 (7) | 0.28 (1) | 1.11 (4) |
| Female | 0.00 (0) | 0.00 (0) | 0.32 (1) | 1.60 (5) | 1.91 (6) | 0.96 (3) | 0.91 (3) | 1.21 (4) | 1.03 (3) | 1.05 (4) | 0.98 (3) | 0.87 (3) | 0.57 (2) | 1.97 (7) |
| Golestan | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.99 (8) | 0.50 (4) | 0.56 (5) | 0.56 (5) | 0.54 (5) | 0.55 (5) | 0.93 (8) | 1.71 (16) | 2.10 (20) | 1.86 (18) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.49 (4) | 1.11 (9) | 0.67 (6) | 0.45 (4) | 0.74 (6) | 0.62 (5) | 1.06 (8) | 1.82 (17) | 1.37 (13) | 0.00 (0) |
| Gilan | ||||||||||||||
| Male | 0.92 (11) | 0.75 (9) | 1.51 (18) | 1.33 (16) | 1.67 (20) | 2.25 (27) | 1.87 (23) | 1.79 (22) | 1.97 (24) | 1.88 (23) | 2.19 (26) | 2.72 (34) | 2.45 (31) | 3.54 (45) |
| Female | 0.25 (3) | 0.50 (6) | 1.58 (19) | 0.91 (11) | 0.58 (7) | 0.58 (4) | 0.96 (12) | 1.04 (13) | 0.86 (10) | 0.95 (12) | 1.07 (13) | 1.41 (18) | 1.95 (25) | 1.08 (14) |
| Lorestan | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 1.95 (17) | 1.72 (15) | 2.04 (18) | 1.25 (11) | 1.67 (15) | 1.65 (15) | 1.44 (12) | 0.99 (9) | 0.77 (7) | 0.87 (8) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 2.37 (20) | 1.19 (10) | 0.69 (6) | 1.03 (9) | 0.97 (8) | 0.90 (7) | 0.77 (6) | 0.45 (4) | 0.44 (4) | 0.88 (8) |
| Mazandaran | ||||||||||||||
| Male | 0.68 (10) | 0.55 (8) | 0.95 (14) | 0.48 (7) | 0.82 (12) | 1.09 (16) | 1.36 (21) | 1.04 (16) | 1.16 (18) | 1.19 (18) | 1.33 (19) | 1.64 (26) | 1.94 (31) | 2.86 (46) |
| Female | 0.41 (6) | 0.27 (4) | 0.62 (9) | 0.82 (12) | 0.55 (8) | 0.96 (14) | 0.98 (15) | 0.65 (10) | 0.86 (13) | 0.83 (13) | 0.90 (13) | 1.02 (16) | 1.95 (31) | 1.75 (28) |
| Markazi | ||||||||||||||
| Male | 1.61 (11) | 2.05 (14) | 0.59 (4) | 1.17 (8) | 1.17 (8) | 1.47 (10) | 2.17 (15) | 1.68 (12) | 1.77 (12) | 1.87 (13) | 1.40 (10) | 0.54 (4) | 2.42 (18) | 0.66 (5) |
| Female | 1.50 (10) | 1.20 (8) | 0.15 (1) | 1.50 (10) | 0.75 (5) | 0.30 (2) | 1.15 (8) | 1.43 (10) | 0.96 (7) | 1.18 (8) | 1.13 (8) | 1.25 (9) | 1.52 (11) | 1.91 (14) |
| Hormozgan | ||||||||||||||
| Male | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.97 (7) | 0.55 (4) | 0.87 (7) | 0.75 (6) | 0.72 (6) | 0.78 (6) | 0.73 (6) | 0.70 (6) | 0.81 (7) | 0.79 (7) |
| Female | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.00 (0) | 0.88 (6) | 0.88 (6) | 0.64 (5) | 1.03 (8) | 0.85 (6) | 0.84 (6) | 0.56 (5) | 0.00 (0) | 0.95 (8) | 0.47 (4) |
| Hamedan | ||||||||||||||
| Male | 1.40 (12) | 0.35 (3) | 0.82 (7) | 1.75 (15) | 0.82 (7) | 1.98 (17) | 2.15 (19) | 1.58 (14) | 1.90 (17) | 1.88 (17) | 2.12 (18) | 2.57 (23) | 2.46 (22) | 2.78 (25) |
| Female | 0.83 (7) | 0.24 (2) | 0.47 (4) | 1.18 (10) | 0.83 (7) | 0.95 (8) | 1.49 (13) | 1.49 (13) | 1.31 (11) | 1.43 (12) | 1.62 (14) | 2.12 (19) | 2.01 (18) | 2.22 (20) |
| Yazd | ||||||||||||||
| Male | 0.77 (4) | 1.16 (6) | 0.97 (5) | 2.52 (13) | 1.55 (8) | 1.74 (9) | 1.81 (10) | 4.34 (24) | 2.63 (14) | 2.93 (16) | 3.67 (21) | 5.45 (30) | 8.59 (48) | 9.28 (53) |
| Female | 1.27 (6) | 1.06 (5) | 0.84 (4) | 0.63 (3) | 2.53 (12) | 0.00 (0) | 1.15 (6) | 2.11 (11) | 1.09 (6) | 1.45 (8) | 2.78 (14) | 5.80 (30) | 6.05 (32) | 3.90 (21) |
Frequency and Age-standardized Incidence Rate (ASIRs) per 100,000 of Kidney Cancer in Provinces of Iran from 2003 to 2016 a
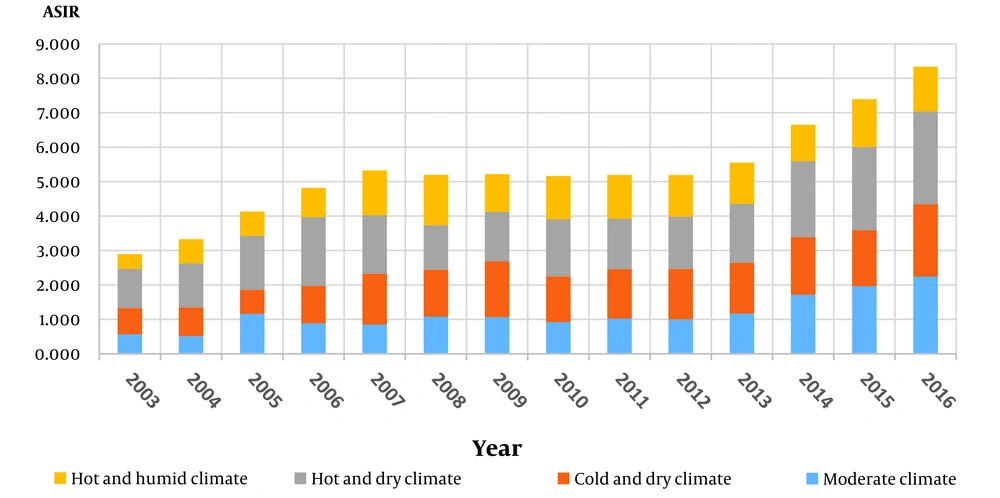
The southern coastline of the Caspian Sea has a moderate climate with high precipitation and humidity. There's a slight temperature difference between the cold and warm seasons. The northern coast of the Persian Gulf has a hot and humid climate characterized by high humidity and very hot summers, along with mild winters. Central parts of Iran have a hot and dry climate with very low humidity and rainfall throughout the year. These areas are deserts with little plant life and experience windstorms with dust. The northwest and northeast regions have a cold and dry climate with extremely cold winters and hot summers. These areas experience heavy snow in autumn and winter, low humidity, and relatively low summer rainfall (Figure 6).
5. Discussion
According to Global Cancer Statistics, there were 431,288 new cases of kidney cancer in 2020, accounting for 2.2% of all new cancer cases. Additionally, there were 179,368 reported deaths related to kidney cancer in 2020, representing 1.89% of all cancer-related deaths (14). The all age incidence ASR of RCC for both sexes is 4.4 per 100,000. Renal cancer is most common in Europe and North America, while the lowest occurrence rate is reported in Asia (6).
The worldwide incidence rate of RCC is on the rise. In high-income countries, this increase could be attributed to the discovery of kidney masses incidentally during abdominal imaging for non - specific musculoskeletal and gastrointestinal complaints (5, 15). Our study revealed that the incidence rate of RCC continued to rise from 2003 to 2016, with the most significant increases observed in men. However, this finding contradicts the results of King et al.'s report. They found that the increasing trend was higher in women than in men (2.3 vs 1.9) (16).
In this study, we showed that ASIR of kidney cancer in 2016 was 3.66/100,000 and 2.24/100,000 for men and women, respectively which are lower than the global incidence of kidney cancer. The highest average of ASIR of kidney cancer from 2033 to 2016 in both genders is reported from central provinces of Iran such as Fars, Yazd, Tehran, and Isfahan. The comparison between 4 climate zones of Iran showed that hot climate zones are associated with a higher incidence of kidney cancer while moderate climate is linked to lower incidence rates. Investigating the spatial distribution of kidney cancer in Iran is valuable for hypothesis setting for risk factors of kidney cancer in high-risk provinces. Our results underscore the necessity of further research on the environmental determinants of kidney cancer such as exposure to radon, and sunlight as well as the presence of arsenic, nitrate, and radon in drinking water.
The first report on the incidence of kidney cancer in Iran was from a study by Sajjadi et al. in Ardabil province between 1996 and 1999. They reported the ASIR of kidney cancer to be 1.10 in men and 1.30 in women (17). Another report by Babaei et al. in Ardabil province from 2000 to 2004 showed an incidence of 3.10 in men and 2.90 in women, respectively (18). Masoompour et al. reported the incidence of kidney cancer in Fars province as 0.97 from 1985 to 1989, 1.30 from 1998 to 2000, and 3.81 from 2007 to 2010 (19). Basiri et al. reported an ASIR of kidney cancer in Iran at 1.8 per 100,000 for men and 2.01 per 100,000 for women between 2003 and 2009 (20). Mirzaei et al. indicated that the ASIR of kidney cancer increased from 1.18 in 2003 to 2.52 in 2009 per 100,000 population (3).
In 2017, Arabsalmani et al. published a study on the relationship between the incidence of kidney cancer and the Human Development Index (HDI) in Asia. They discovered a positive correlation between ASIR and HDI. The ASR of kidney cancer incidence in Iran in 2012 was reported as 2.10 in men and 3.00 in women (21) In 2018, Hassanipour et al. conducted a systematic review of kidney cancer studies conducted in Iran and estimated the ASIR of kidney cancer in men 1.94 (95% CI: 1.62 - 2.55) and in women 1.36 (95% CI: 1.09 - 1.62). They concluded that the incidence of kidney cancer in Iran is lower than in other parts of the world, but more studies are needed to accurately determine the incidence of kidney cancer and its trend in Iran (22).
Renal cell carcinoma typically occurs between the ages of 60 and 70 and decreases after the age of 70. This decline could be due to fewer aggressive diagnostic procedures being used in older individuals (16). In our study, the lowest incidence rate of kidney cancer was in the age group of ≤ 45 years old, while the highest incidence among men was observed in the 75 to 79 age group. However, in contrast to other reports, kidney cancer occurred more frequently in women aged 80 years and older. RCC is more common in men than in women (1.5: 1) and the mortality rate is higher in men (6). In this study, we showed that the ratio for male to female ASIR was 1.65:1 which is parallel with world statistics. However, a recent global study in 2020 showed that ASR of incidence and mortality of male kidney cancer is about 2-folds in men; in 2020, ASIR of male kidney cancer was reported 6.1 per 100,000 while ASIR of female kidney cancer was 3.2 per 100,000 (14).
5.1. Conclusions
While the incidence rate of kidney cancer in Iran and its provinces is low, there is a growing concern, especially among men. It is essential to develop cost-effective screening tests for high - risk individuals at the national level. Implementing control and prevention programs are crucial in high - incidence provinces such as Fars, Tehran, Chaharmahal Bakhtiari, Kohkilouye, and Boyer Ahmad. Additionally, kidney cancer has common and controllable risk factors such as occupational exposure, smoking, and obesity. This highlights the significance of prevention in addressing kidney cancer. Therefore, it is highly recommended to conduct studies on kidney cancer risk factors in high - risk areas in Iran.