1. Background
The health status of the community, residents' satisfaction with the health services, and protection against financial risks are the main purposes of evaluating the health system's performance (1). However, benefiting health services leads to catastrophic health expenditure, that is, can make households pay part of their income directly or out-of- pocket (OOP), which renders the large number of households in poverty (2).
Direct payments or OOP payments are the health care financing resources. The fact is that this approach is the worst strategy to meet the health financing need, from the view point of protection against financial risk and equity (3). These types of payments have negative impacts on health care productivity and health, as well as important effects on living standards. The welfare of a community is under the influence of unmet medical costs and direct payments. Households may borrow to cover the unexpected medical expenditures, but they will run into long-term debt (4). Because of the impact of OOP payment on living standards and well-being, the World Health Organization (WHO), in 2000, declared the equity index as one of the key variables in measuring the health services systems performance (5).
This index is to the extent important that, the WHO has given it a weight of 25% to calculate the general index of health performance (6). However, part of the households’ income in all societies is spent on health care. The rate of its contribution and distribution in societies indicates the imposition of the financial burden of health care on communities (7). Iran's health system is experiencing an epidemiological transitional period and due to the life span increase of individuals and facing the diseases of the industrial world (lifestyle changes, obesity and related diseases, hypertension, cardiovascular events, traffic accidents, cancers, and other chronic diseases), it has been under a double burden of disease (8). These diseases not only threaten the live and well-being, but also endanger financial security. In diseases, such as cancer, the medical cost of OOP can be unaffordable. The medical costs for cancer patients impose rigorous burdens on governments and patients. Studies indicate that the cancer patients, who face the OOP payment, potentially affect their financial performance (9).
In addition, the disease can impair a person’s ability to function and perform tasks, at home and work, and even it influences national production. Cancer disease due to its potentially life-threatening consequences and illness period can be life-threatening and change the person’s life condition. Breast cancer with the highest prevalence rate is the most important health concern in women. Globally, 2.3 million women were diagnosed with breast cancer and 685 000 deaths in 2020. As of the end of 2020, there were 7.8 million women alive, who were diagnosed with this disease in the past 5 years, making it the world’s most prevalent cancer (10).
In Iran, breast cancer is the most common cancer in women and comprises 21.4% of all cancers in women (11). The onset of breast cancer in Iran is 22 per 100,000 and the prevalence rate is 120 per 100,000 women aged 15 to 84 years (12). However, the global survey reveals an elevation in the incidence of breast cancer, but a faster rise in developing countries (13). According to the previous studies, the incidence of breast cancer in Iranian women occurs 10 years earlier than the western women (14). Data indicate that 70% of breast cancer patients in Iran die early due to delay in the diagnosis and being in the advanced stages of the disease (15). In 2013, Iran National Cancer Control was developed with a strategic planning approach that consists of 4 main processes and 7 support processes. Also, this program has been able to relatively achieve its short-term goal, but to achieve the expected outcomes, it is essential to strengthen the governance structure and the commitment of health policy makers to implement this program (16). However, benefiting effective health care is poor for breast cancer patients, who live far from cancer treatment centers. Though effective treatment is important for the physician and patient, the financial problems and the medical cost imposed on the patient, delay the treatment process, because the patient may not cooperate, especially those who live far from the medical setting. OOP payment for health care prevents access to medical services that influences the health and quality of life, and leads to the financial shortage for the other expenditures (17).
In general, breast cancer costs around 2 to 3 thousand dollars per month in the world (11). Treating early-stage breast cancer is more cost-effective than late-stage disease. In Asia and Africa, treatment of stage I, II, or III disease costs less than 390 dollars per disability-adjusted life years (DALY) averted, whereas treatment of stage IV disease costs more than 3500 dollars per DALY averted (18). Various studies have shown that direct health care costs impose the greatest financial burden on the patient and society. A study by Bazyar et al. on cancer patients admitted to the cancer center of Imam Khomeini Hospital in Tehran in 2010 showed that, on average, 91% of the total OOP payment of patients was related to medical direct costs and the share of non-medical direct costs, from out of total costs was only 9%. Bazyar et al. showed that the average OOP payment for the medical direct care costs was about 38.9 dollars. However, the average cost of non-medical direct payments was estimated to be around 23.9 dollars (19).
In Iran, financial resource for health care is provided in part by the government and insurance agencies. It is important to know what services expose the patients to higher OOP payment and what patients face the burden of breast cancer treatment costs. Therefore, the authors decided to identify the rate of these OOP payments in breast cancer patients to find ways to protect them from the negative effects of this condition and to identify the financial burden on these patients.
2. Objectives
This study aimed at determining OOP payments among women with breast cancer at health care centers affiliated to Iran University of Medical Sciences.
3. Methods
This descriptive cross-sectional applied study seeks to estimate the costs imposed on the patients with breast cancer at each stage of the disease in the second trimester of 2018 onwards. The study population included all hospitalized patients with breast cancer, who were admitted to Rasol Akram and Firozgar Hospitals for treatment of breast cancer. The data collection tool in this study was a researcher-made questionnaire; its content was obtained using two other questionnaires used by other authors (20, 21). The final questionnaire after correction and review, consisting of 21 questions was used for OOP payment, aimed at determining the hospital cost of the patients and their families. The validity of this questionnaire was reviewed and validated by health economists and 3 oncologists at both centers. Using the questionnaire, referring directly to the research setting and according to the questionnaire questions, the question on data and cost information from the patients or the patient's family was asked. Results as the average of OOP payments for medical direct costs, the average of OOP payments for non-direct costs, informal payments, and a total of OOP payments were reviewed. Data were analyzed, using SPSS software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.); mean and standard deviation of data collected from questionnaires and bills of hospital expenses were extracted according to the purpose of analysis. Then, sum of the averages obtained was extracted from the average of the total OOP payments.
4. Results
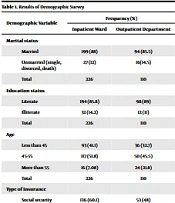
This section discusses the most important findings of OOP payment in breast cancer patients consisting of results of a demographic survey, medical direct and non-medical direct costs from OOP payment, informal OOP payment, and total average OOP payment in women with breast cancer.
4.1. Demographic Features of the Studied Patients
According to the findings of the study (Table 1), the majority of patients under study were married (88% and 85.5%, respectively) and only 12% of inpatients and 14.5% of outpatients were single. Also, the majority of inpatients and outpatients were literate (86% and 89%, respectively), and only 14% of the inpatients and 11% of the outpatients were illiterate. Most hospitalized patients (52%) and most outpatients (45%) were between the ages of 45 and 55 years. Most hospitalized patients (60%) and most outpatients (48%) had social security insurance. Also, all women with breast cancer under study had a companion.
| Demographic Variables | Frequency (%) | |
|---|---|---|
| Inpatient Ward | Outpatient Department | |
| Marital status | ||
| Married | 199 (88) | 94 (85.5) |
| Unmarried (single, divorced, death) | 27 (12) | 16(14.5) |
| Total | 226 | 110 |
| Education status | ||
| Literate | 194 (85.8) | 98 (89) |
| Illiterate | 32 (14.2) | 12 (11) |
| Total | 226 | 110 |
| Age | ||
| Less than 45 | 93 (41.1) | 36 (32.7) |
| 45 - 55 | 117 (51.8) | 50 (45.5) |
| More than 55 | 16 (7.08) | 24 (21.8) |
| Total | 226 | 110 |
| Type of insurance | ||
| Social security | 136 (60.1) | 53 (48) |
| Health service | 58 (25.7) | 42 (38) |
| Public health | 32 (14.1) | 5 (5) |
| Others | 0 (0) | 10 (9) |
| Total | 226 | 110 |
Results of Demographic Survey
According to Table 2, most outpatients have used a taxi to get their services for intra-city travel (43%), and most of them used buses (64%) and private cars (30%) to travel outside the city.
| Vehicle Type | Frequency (%) |
|---|---|
| Intra-city travel | |
| Taxi | 47 (43) |
| private car | 32 (29) |
| Subway | 31 (28) |
| Total | 110 (100) |
| Out-of-city travel | |
| Bus | 41 (64) |
| Private car | 19 (30) |
| Train | 0 (6) |
| Airplane | 0 (0) |
Frequency Distribution Type of Vehicle in Intra-city Travel and Out-of-city Travel for Outpatient
According to the findings, 43% of patients with breast cancer had spent at least one night out of their home to benefit from medical care, living either in the inn or at the home of relatives (Table 3).
| Type of Residence | Frequency (%) |
|---|---|
| Inn | 20 (18) |
| Relatives' home | 27 (25) |
| No need to stay out of home | 63 (57) |
| Total | 110 (100) |
Frequency Distribution of Outpatients Based on Residing or Not Residing at Home
4.2. Out-of-pocket Payment for Inpatients
According to Table 4, among medical direct costs, drug costs with an average of 38 dollars imposed the highest OOP payment on women with breast cancer, which accounted for 30% of direct OOP payment. The chemotherapy and hoteling with 18 dollars and 18 dollars, respectively, ranked second medical direct OOP payment. Radiology with costs of 2 dollars imposed the lowest amount of OOP payments for patients under study.
| Cost Type | Average ± SD (US$) | Percentage |
|---|---|---|
| Visit | 15.25 ± 10.72 $ | 13 |
| Surgical procedure | 22.10 ± 8.18 $ | 9 |
| Anesthesia | 3.97 ± 0.648 $ | 5 |
| Surgery room | 3.21 ± 4.632 $ | 4 |
| Drug | 37.99 ± 26.03 $ | 30 |
| Radiology | 1.24 ± 2.46 $ | 3 |
| Lab | 4.76 ± 15.14 $ | 7 |
| Chemotherapy | 11.28 ± 22.20 $ | 15 |
| Hoteling | 5.73 ± 21.33 $ | 15 |
| total patient payment | 34 ± 118.73 $ |
Monthly Average OOP Payments for Medical Direct Costs in Patients with Breast Cancer a
4.3. Out-of-pocket Payment for Outpatients
4.3.1. The Medical Direct Cost of OOP Payment
According to Table 5, among medical direct costs, chemotherapy with an average of 23 dollars (33%) imposed the highest OOP payment in women with breast cancer in hospitals affiliated to Iran University of Medical Sciences.
| Cost Type | Median Onset of Disease (Non-metastatic) | Patient Payment (US$) | Total Cost (US$) |
|---|---|---|---|
| Visit of specialist physician | 15 | 1 $ | 15 $ |
| Lab | 10 | 1.06 $ | 10.72 $ |
| Sonography | 1 | 1.34 $ | 1.34 $ |
| Mammography | 1 | 21.35 $ | 21.35 $ |
| Chemotherapy | 8 | 2.83 $ | 22.66 $ |
| Total | 35 | 26.42 $ | 68.66 $ |
The Average Types of Medical Direct Cost of OOP Payment in Breast Cancer Outpatients a
4.3.2. The Non-medical Direct Cost of OOP Payment
Among the non-medical direct costs, transportation with an average of 31 dollars imposed the highest rate of OOP payments in women with breast cancer (Table 6).
| Cost Type | Average ± SD (US $) |
|---|---|
| Transportation | 30.65 ± 10.32 $ |
| Accommodation and food | 2.11 ± 2.56 $ |
| The sum of payment | 34.88 ± 31.12 $ |
The Average of All Non-medical Direct Cost of OOP Payments in Breast Cancer Outpatients a
4.4. Unofficial OOP Payments
Based on the completed questionnaires, no informal payments were reported by patients and their companions.
| Out-of-Pocket Payment | Average ± SD (US $) |
|---|---|
| Direct hospitalization costs in the inpatients | 146.45 ± 47.98 $ |
| Direct costs of treatment in outpatients | 68.66 ± 102.99 $ |
| Regarding non-medical direct costs and informal payments | 34.88 ± 3112 $ |
| Total | 250 ± 182.10 $ |
Total Out-of-pocket Payments in Breast Cancer Patients
According to Table 7, each breast cancer patient paid an average of 694 dollars directly to the governmental health care centers. All the costs were converted to US dollars (US $), using the average annual 2018 exchange rate (US$1 = Rial 42,000).
5. Discussion
According to the results of this study, the majority of patients were married (85.7%), literate (89%), with the age range of 45 to 55 years (52%), and those benefiting the health insurance services (60%). Cancer patients' costs are divided into 3 categories of medical direct costs, non-medical direct costs, and informal payments. Along with these costs, informal payments may also be imposed on cancer patients (22). Among medical direct costs, drug costs with an average of 37.99 dollars among inpatients, and, chemotherapy costs in the outpatient with an average of 2.26 dollars imposed the highest rate of OOP on breast cancer patients in hospitals affiliated to Iran University of Medical Science. The costs of chemotherapy and hoteling ranked next in the OOP payment for medical direct costs, respectively. The costs of radiology and ultrasound imposed the lowest amount of OOP payments on the patients under study.
In various studies, the chemotherapy cost included the highest rate of direct medical costs. The study of Imani et al. on patients referring to the Tabriz Shahid Qazi Clinic in 2013 indicated the highest rate of medical direct costs related to medical and drug costs ranked next (23). One of the reasons for the discrepancies between the present study with these studies could be due to the implementation of the health transformation plan in Iran and its effect on the costs of chemotherapy. On the other hand, the findings of studies of Dahlberg et al. and Barron et al. are consistent with the data of the present study. Dahlberg et al. concluded that the cost of medicine was the highest among medical direct costs in breast cancer patients (24, 25). Barron et al. in their study on economic costs of breast cancer in the United States estimated drug costs of about 375 dollars, which is attributed to the highest rate of treating breast cancer patients (25).
Imani et al. showed that the lowest direct medical costs were related to the costs of visiting the patients and outpatient care but did not agree with the findings of the present study (23). One of the reasons for differences between our findings with the other studies could be due to the implementation of the health transformation plan in Iran, which has reduced the cost of diagnostic tests, such as radiology. Among the direct non-medical costs, transportation with an average cost of 30.65 dollars (87%) imposed the highest rate of OOP payments on breast cancer patients. Lodging and boarding rated the lowest costs with an average of 2.11 dollars.
In the study of Lee et al. the most common direct non-medical cost of OOP payment was for traveling and accommodation, which is inconsistent with the findings of the present study (26). In the study of Longo the highest rate of non-medical direct OOP payment was related to traveling ccosts (27), which is consistent with the findings of the present study. A study by Gordon et al. in Australia on OOP payment revealed that 70% of non-medical direct OOP payment was related to traveling (28), which is in line with the findings of the present study.
Cancer patients' costs are divided into 3 categories of medical and non-medical direct costs and informal payments. In addition to these costs, informal payments may also be imposed on cancer patients. Among the medical direct costs, drug costs averaging 37.99 dollars shared the highest OOP payment for the women cancer patients admitted in hospitals affiliated to Iran University of Medical Sciences. Among the non-medical direct costs, traveling had an average cost of 30.65 dollars. Along with these costs, informal payments may also be imposed on cancer patients. These findings show that individuals with breast cancer endure high OOP payments that could adversely affect their quality of life. It should also be noted that the exchange rate is one of the important economic variables that affect the inflation of the health sector. The effect of exchange rate fluctuation on the consumer price index is very high, which can naturally lead to an increase in the price of medicine and health care, and consequently the payment from patients' pockets (29).
On the other hand, lower levels of social support are associated with higher mortality rates due to cardiovascular diseases, cancer, and infection (30). Also, there is a significant relationship between income variables and health-promoting lifestyle (31, 32). There is a relationship between income and forgone care influenced by the amount of public health expenditure. This issue is very important for health policies. This is because cost-related barriers not only block access to health care, but also affect patients' subsequent trust in health care systems when they perceive themselves to be critically ill (33). As a result, it can be said that people's income can have a significant impact on treatment and OOP payments.
Regarding the use of new treatment methods, it can be said that the number of cancer survivors is increasing thanks to early diagnosis, new treatment methods, and population growth.
Surgery, radiotherapy, and chemotherapy are common methods of cancer treatment. Today, radiotherapy is an important part of cancer treatment, and almost two-thirds of cancer patients are treated with radiotherapy. Also, hyperthermia using high-intensity focused ultrasound (HIFU) is one of the newest and most practical non-invasive technologies in the treatment of cancer tumors (34, 35). A point that should be noted is about the economic status of countries and their economic power and that of patients as well as economic support for patients to use new technologies. Of course, it should be noted that decision-makers in low- and middle-income countries cannot get comparable breast cancer control strategies as actualized in high-income countries since most low- and middle-income countries depend on much smaller budgets (36, 37). Iran's National Cancer Control Program has 4 main components, including prevention, early detection, diagnosis and treatment, and supportive and palliative care (38). The correct implementation of these components can greatly help in the cost reduction of patients.
5.1. Limitations and Strength
There were some limitations in our article. Firstly, limiting the sample to two hospitals was one of limitations of the study. Secondly, no informal payments were reported in this study. The strength of the study is providing details of different types of costs available for researchers and policy making.