1. Introduction
Struma ovarii is a rare distinct ovarian tumor characterized by containing either entirely or predominantly thyroid tissue (> 50%), which accounts for less than 1% of all ovarian tumors and approximately 3% of ovarian teratomas (1, 2). The prevalence of struma ovarii in the general population remains uncertain due to its rarity and often asymptomatic nature (2, 3). The condition was first described in the early 19th century in the literature and has since attracted significant interest due to its rarity and diverse clinical manifestations. Clinical and biochemical features of hyperthyroidism are rare in women with struma ovarii, happening in fewer than 5 to 8 percent of cases (4, 5). On imaging techniques its morphology is similar to neoplastic lesion. Therefore, definitive diagnosis is made only after surgery on the basis of histopathological examination of the surgical specimen, which reveals the presence of thyroid follicles or other thyroid tissue within the ovary (1, 5). To the best of our knowledge, no cases of struma ovarii presenting with elevated levels of CA-125, hyperthyroidism, and weight loss have been previously reported from Kabul, Afghanistan. In this case report, we presented the first documented case from the pathology department of Kabul University of Medical Sciences. Our aim was to bring attention to this rare pathology among clinicians and underscore the importance of recognizing and managing such cases effectively.
Written informed consent was obtained from the guardian of the patient for the publication of this case report and accompanying images. All ethics considerations were taken into account, ensuring the privacy of the patient’s identity, profile, and photograph
2. Case Presentation
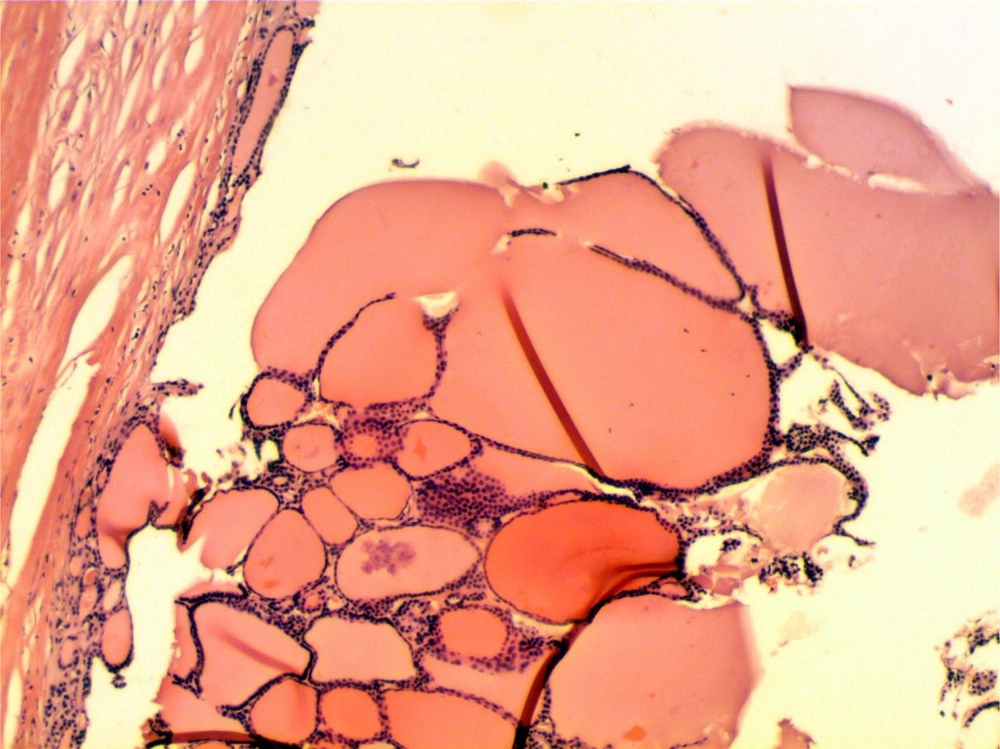
A 50-year-old Afghan woman, who was menopausal and had a history of two pregnancies and two deliveries (gravida 2, para 2) referred to our hospital. She presented with a 5-month history of weight loss, anorexia, abdominal pain, palpitation and tremor. Upon arrival, her vital signs were recorded as follows: Blood pressure (BP) = 140/75, heart rate (HR) = 106 bpm, pulse rate (PR) = 106 bpm, respiratory rate (RR) = 20 cycle/min, and oxygen saturation (SpO2) = 95% at room temperature. The patient appeared anxious, and the physical examination revealed tachycardia in the cardiovascular system (CVS) and a palpable mass in the lower abdomen. CT scan of abdomen and pelvis with IV contrast showed a large well-defined complex cystic lesion with multiple enhancing internal septa and a few enhancing mural nodules. This lesion was located posterior to the uterus, abutting both ovaries, measuring 11.0 × 9.1 ×7.3 cm. However, the possibility of malignancy could not be entirely rule out. Blood tests indicated elevated levels of T3 and T4, along with low levels of TSH. Additionally, both the thyroid-stimulating hormone receptor antibody and thyroid-stimulating antibody were found to be negative. The patient’s thyroid gland was not palpable and cervical ultrasonography showed normal thyroid morphology. However, The CA-125 serum level was evaluated at 640 U/mL (normal range level < 35 U/mL). Based on the patient’s symptoms, radiological findings and high level of CA-125; the clinician suggested a diagnosis of ovarian cancer. Given the patient’s referral to our governmental hospital and her limited financial resources, which prevented her from affording the costs associated with biopsy and other diagnostic tests, the surgeon initially recommended a procedure of hysterectomy with bilateral salpingo-oophorectomy. This approach was chosen considering her menopausal status, with the procedure serving both diagnostic and therapeutic purposes. However, the patient and her relatives consented only to the operation targeting the identified lesion and declined the removal of normal organs. Consequently, a left ovarian salpingo-oophorectomy procedure was performed. The surgical specimen was subsequently sent to our governmental pathology department for accurate diagnosis. Before surgery, we administered a beta-blocker to maintain the patient’s pulse rate below 80 bpm. Additionally, a thionamide was given until the patient achieved a euthyroid state. Grossly, the specimen consisted of gray-white cystic lesion with smooth surface, measuring 10 × 8.0 × 6.0 cm (Figure 1). On the sections, a multicystic lesion with scattered areas showing solid papillary growth was observed. Microscopic examination revealed a benign cystic lesion characterized by degenerated overlying epithelial cells. In the cystic wall fibrosis, hemorrhage and hemosiderin laden macrophages were noted. Additionally, there were variably sized macro and microfollicular of thyroid parenchyma and some often seen with colloid materials (Figure 2). Grossly and microscopically the left fallopian tube was unremarkable. Based on the histopathologic examination report, the diagnosis of the benign struma ovarii was confirmed. The patient was discharged home on the fifth postoperative day. Six months post- surgery, the patient’s condition had improved significantly. She had partially regained the lost weight and the serum level of thyroid hormone, thyroid stimulating hormone and CA-125 serum level were within the normal ranges.
5. Discussion
Struma ovarii is a rare ovarian lesion, which accounts less than 1% of ovarian tumor. It typically affects women of reproductive age, with a peak incidence in the fourth to sixth decades of life. The clinical presentation of struma ovarii can vary widely and thus misdiagnosis to other ovarian lesions is very common. Around 40% of cases are asymptomatic and incidentally detected during imaging or surgery and in symptomatic cases of struma ovarii, some patients may experience symptoms like abdominal pain, pelvic mass, menstrual abnormalities, or compressive symptoms due to tumor enlargement. In our patient apart from the above non-specific symptoms, she had also hyperthyroidism with weight loss; which only reported in 5% to 8% of cases in the literature (4, 5). The connection of struma ovarii with high CA-125 titers is similarly rare, with just a few cases lately recorded in the literature (6). The precise cause of the increased CA-125 in our case is unknown. Due to non-specific clinical symptoms, no specific characteristics on imaging techniques, and rarity of this lesion; the clinician misdiagnosed it as the common cysts of the ovary. The definitive diagnosis is made only by histopathological examination of surgical specimen (1, 5). The management of struma ovarii depends on several factors including the patient’s age, symptoms, tumor size, and presence of malignancy. Surgical removal of the tumor, either through unilateral oophorectomy or, in more extensive cases, bilateral salpingo-oophorectomy has been accepted as therapeutic approach. In rare instances of malignant transformation, additional treatments such as radiotherapy or chemotherapy may be warranted (7). In our patient, left ovarian salpingo-oophorectomy was performed, which after six months following up, the patient’s serum level of T3, T4, TSH and CA-125 were in normal range and her weight lost were recovered.
5.1. Conclusions
Struma ovarii is a rare ovarian neoplasm, and its association with CA-125 and hyperthyroidism is an extremely rare. Complete surgical resection of this lesion is sufficient for management. Diagnosis based solely on clinical manifestations or imaging studies is challenging due to the diverse presentation of features. Accurate diagnosis is made only by postoperative histopathological examination and should be kept in the differential diagnosis of all ovarian cystic lesions.