1. Context
Patients require accurate and reliable information about their diagnosis, treatment options, and potential outcomes to make informed healthcare decisions (1). Medical staff and nurses often have to disclose bad news about their patient's health status, including difficult information related to life-threatening or progressive diseases, poor prognosis, treatment failure, complications, amputation, and death (2, 3). The process of delivering bad news involves the patient care team, who must cooperate effectively with social workers and the patient’s family to ensure successful outcomes (4). It is ideal to share tough news with the entire healthcare team—physicians, nurses, social workers, and chaplains—in a collaborative manner. Each person can share his/her knowledge and offer the patient and family comprehensive support. This multidisciplinary approach aids in making sure that every facet of the matter is taken care of (5). Although some studies suggest that physicians are considered responsible for breaking bad news (BBN) (6, 7), nurses are also integral members of the care team in terms of informing and supporting patients and their families (8). In addition to providing information, nurses can also play a crucial role in assisting patients in understanding and coping with bad news (9); 90% of patients in one study stated that providing emotional support was among nurses’ main roles (10). Therefore, nurses must acquire the necessary skills to assist patients in preparing, receiving, understanding, and dealing with bad news (11).
In terms of nurses’ perspectives on their role in BBN, Reinke et al. determined that oncology and pulmonary care nurses in the US considered it a team process, in which physicians take the lead in introducing bad news, while nurses continue discussions afterward, liaise between patients and physicians, and foster patients’ hope (12). It is acknowledged that BBN for patients and their families is a delicate and intricate procedure, and nurses are essential to this process. Their assistance goes beyond the disclosure moment to include planning, assistance, and aftercare (13, 14). Similarly, Mahasti Jouybari et al. (as cited by Imanipour) noted that nurses did not consider delivering bad news their responsibility and preferred an indirect role, and Karim et al. reported that only 34% of intensive care and emergency department nurses delivered bad news directly to patients or families (15, 16). Imanipour et al. determined that most coronary care and intensive care nurses in Iran had positive attitudes toward their involvement in the process of BBN, but acknowledged that few (16.2%) were very knowledgeable about how to deliver bad news (16). Ptacek and Ellison’s study highlighted the crucial role of nurses in providing emotional support and facilitating patients’ emotional expression while delivering bad news (17). Warnock et al. also reported that nurses were involved in various stages of the news delivery process, but had little education on the subject (18).
Several factors affect nurses’ communication skills when announcing bad news, including burnout and fatigue, time constraints, lack of experience, and personal barriers such as spiritual and cultural beliefs, personal attitudes, and fear of harming the patient or being blamed (19). Identifying nurses’ roles in delivering bad news can minimize ethical gaps and align care with their values and needs despite the challenges associated with their participation (20). Nurses are crucial in the communication between doctors, patients, and their companions, yet their role in delivering bad news has been undervalued (21). There are also differences of opinion regarding nurses’ professional responsibility regarding the disclosure of bad news. In Iran, nursing education lacks specific content on delivering bad news, but clinical evidence suggests that nurses in intensive care and emergency departments often need to be involved in the process, sometimes independently (22). A study by Shomoosi et al. showed that in Iran, 71.1% of nurses lack formal training on how to deliver bad news (23). In specialty care departments, when doctors are unavailable and bad news is delayed, nurses face additional pressure and difficult situations (24).
Despite nurses’ diverse roles in the process of delivering bad news, these roles have not been given importance in education and clinical practice. This has resulted in challenges, psychological problems, and a lack of organizational support. Therefore, this study aims at characterizing and raising awareness of the roles of nurses in the delivery of bad news with the ultimate goal of guiding future educational initiatives.
2. Methods
This integrated review was based on the approach proposed by Whittemore and Knafl (11). Based on a pilot review, we determined the most effective literature review approach for the study would be an integrated review, which combines various document types and approaches to summarize the available data (11, 25). This approach has 5 main stages: Problem identification, literature search, data evaluation, data analysis, and presentation (11).
2.1. Stage 1: Problem Identification
The first step in an integrated literature review is identifying the problem (11). The unclear scope of nurses’ role in reporting bad news can lead to neglect in care provision and associated problems, as well as pose a barrier to effective education in this area. The present integrative review was conducted to answer the following research question: What specific roles do nurses play in the process of BBN to patients and their families in hospitals?
2.2. Stage 2: Literature Search
At this stage, 2 researchers independently searched for articles related to the role of nurses in delivering bad news to patients and families published in the English or Persian literature between January 1, 1980, and January 1, 2022, in the following online databases: Magiran and Scientific Information Database (SID), PubMed, Web of Science, ScienceDirect, Google Scholar, and Scopus. These databases were selected because of their large number of scientific journals and a large number of results obtained searching with the selected keywords in the title and abstract (tiab) or article keywords. The searched keywords, extracted from MeSH, included variants of the terms “breaking bad news”, “truth disclosure”, “error disclosure”, “patients”, “clients”, “families”, and “nurse’s roles” using the Boolean operators (AND, OR): (“bad news”[tiab] OR “breaking bad news”[tiab] OR “truth disclosure”[MeSH] OR “truth disclosure*”[tiab] OR “error disclosure*”[tiab]) AND (“patients”[MeSH] OR “family”[MeSH] OR “patient*”[tiab] OR “client*”[tiab] OR “famil*”[tiab] OR “relativ*”[tiab] OR “patient* and famil*”[tiab]) AND (“nurses”[MeSH] OR “nurse*”[tiab] OR “nursing personnel*”[tiab] OR “team nurse*”[tiab]) AND (“role of the nurse”[tiab] OR “nurse’s role”[tiab]). A medical librarian validated the literature search strategy. Other examples of literature search strategies are provided in the supplementary file. A manual search was also carried out by reviewing the list of references to ensure that all candidate studies were identified and reviewed. Books, policy papers, clinical guidelines, letters to the editor, publications in languages other than English and Persian, articles unrelated to the objective, articles for which the full text was not available, and those concerning the roles of staff other than nurses were excluded. A literature search was performed based on the inclusion criteria shown in Table 1.
| Variables | Description |
|---|---|
| Inclusion criteria | Open access studies; having full text; publication in English or Persian language; publication between 1980 - 2022; description of the role of nurses in delivering bad news to the patient and family |
| Exclusion criteria | Books, policies, clinical guidelines; letter to the editor; other languages; articles unrelated to the goal; the full text of the article is not available; related to the role of other treatment staff |
Inclusion and Exclusion Criteria
2.3. Stage 3: Data Evaluation
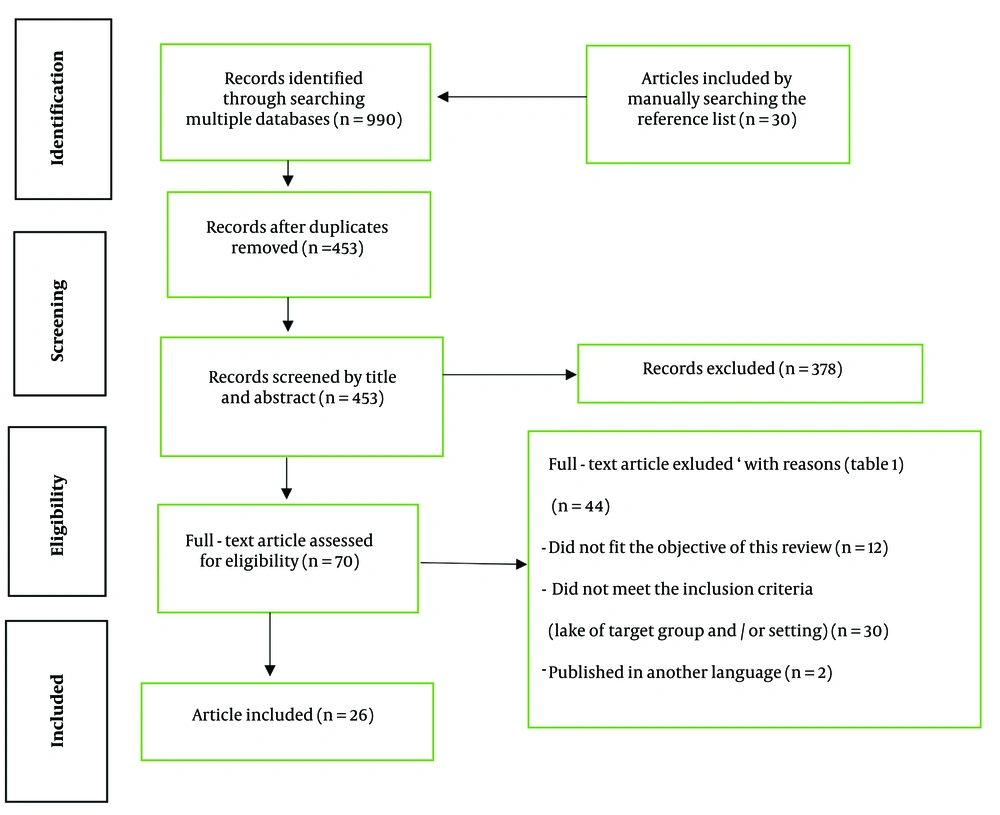
Selection and screening of the documents were done, using the Preferred Reporting Items for Meta-Analyses and Systematic Reviews (PRISMA) guidelines (Figure 1) (11, 26). The first and second authors independently evaluated the titles and abstracts of the retrieved documents to determine their eligibility after eliminating duplicate records. If there were any doubts about whether a particular document should be included or excluded, its entire text was evaluated. Any disagreements between the first and second authors were resolved by the third author.
The first and second authors independently appraised the quality of the included studies, using the critical appraisal techniques of the Joanna Briggs Institute (JBI) (27). Any disputes were resolved by the third author. According to the integrative review methodology, (26, 28) regardless of the quality appraisal scores of the included studies, all were included in the final analysis.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) abstract diagram for process of search, study selection and extract. Notes: Designed based on the Moher et al. (29)
Finally, the first and second authors separately extracted information on the studies’ authors, country, date of publication, design, and objectives and recorded this information on a data collection sheet (Table 2). The roles of nurses in delivering bad news were also extracted from the included articles (Table 3). Any disagreements on data extraction were resolved by discussion.
| Purpose | Design | Country | Year | Author(s) |
|---|---|---|---|---|
| Communication of bad news in the context of neonatal palliative care: Experience of intensivist nurses | Qualitative | Brazil | 2022 | Camilo et al. (30) |
| Supporting hope and prognostic information: Nurses ’perspectives on their role when patients have life-limiting prognoses | Qualitative | USA | 2011 | Reinke et al. (12) |
| Exploration of Irish nurses’ experiences of caring for patients when a cancer diagnosis is given in an acute care facility | Phenomenological | Ireland | 2012 | Tobin (31) |
| Death telling: Managing the delivery of bad news | Qualitative | USA | 1982 | Clark and LaBeff (32) |
| To explore the role of district nurses in breaking bad news of transition to dying | Qualitative focus groups | UK | 2015 | Griffiths et al. (33) |
| Nurses' experiences of being present with a patient receiving a diagnosis of cancer | Phenomenological descriptive | Northern Ireland | 2000 | Dunniece and Slevin (34) |
| To explore the difficulties experienced by nurses and healthcare professionals when engaging in the process of breaking bad news | A descriptive survey | UK | 2017 | Warnocket al. (35) |
| Nurses experiences in giving bad news to patients with spinal cord injuries | Grounded theory | Canada | 2000 | Dewar (36) |
| Explore the perspectives of Iranian nurses on breaking bad news to patients and their families. | Qualitative content analysis | Iran | 2014 | Abbaszadeh1 et al. (37) |
| Nurses' experiences of delivering bad news to patients and their companions | Qualitative content analysis | Iran | 2013 | Mahasti Jouybari et al. (as cited by Imanipour) (16) |
| To examine the phenomenology of truth-telling based on nurses’ experiences | Qualitative | Iran | 2013 | Ezadi et al. (38) |
| Role of the critical care nurse in disclosing difficult news | Review | USA | 2019 | Uveges et al. (20) |
| The role of the critical care nurse in the delivery of bad news | Review | Canada | 2003 | Peel (39) |
| Nursing’s role in disclosure and apology | Review | USA | 2010 | Pfrimmer et al. (40) |
| A process for delivering Bad News: Supporting families when a child is diagnosed | Review | Canada | 2001 | Boyd (41) |
| To increase readers’ understanding of the role of the nurse in the process of breaking bad news and the factors that influence nursing care | Review | UK | 2014 | Warnock (14) |
| Breaking bad news to parents: The children’s nurse’s role | Review | UK | 2006 | Price et al. (42) |
| Critical care nurses’ attitudes, roles, and barriers regarding breaking bad news | A descriptive, cross-sectional | Amman | 2022 | Rayan et al. (5) |
| The role of health care professionals in breaking bad news about death: The perspectives of doctors, nurses and social workers | A descriptive | Israel | 2013 | Rassin et al. (43) |
| Caregivers’ role in breaking bad news patients, doctors, and nurses’ points of view | A descriptive | Israel | 2006 | Rassin et al. (44) |
| Disclosing bad news to patients with life threatening illness: Differences in attitude between physicians and nurses in Israel | A descriptive | Israel | 2009 | Ben Natan et al. (45) |
| The physician-nurse collaboration in truth disclosure: From nurses’ perspective | A cross-sectional survey | Chinese | 2021 | Cheng et al. (46) |
| Report of an exploration of the role of the nurse in the process of breaking bad news in the inpatient clinical setting and the provision of education and support for nurses carrying out this role | A descriptive survey | UK | 2010 | Warnock et al. (18) |
| How to break bad News: Physicians’ and nurses’ attitudes | A descriptive | Iran | 2010 | Arbabi et al. (47) |
| Assessment of nurses' knowledge about how to convey bad news to patients and their companions | A descriptive | Iran | 2014 | Ravanipour et al. (9) |
| Determine types of bad news common in intensive care units and emergency departments and investigate nurses ‘participation in the process of breaking bad news | A descriptive | Iran | 2015 | Karim et al. (15) |
List of Selected Studies, Related to the Role of Nurses in Delivering Bad News
| Main Roles of Nurses | Subordinate Roles Nurses | Number of Articles | Reference |
|---|---|---|---|
| Facilitator | The nurse's active presence when delivering bad news to explain the doctor's words in a more straightforward and understandable language, listen to the patient's words, explain complex medical terms, answer questions and ambiguities | 17 | (5, 12, 14, 16, 18, 31, 34-37, 40-42, 46) |
| Allowing the patient and family to talk | 6 | (5, 16, 18, 31, 36, 40) | |
| Assess patient's needs, requests, and conditions to provide information, identify and clarify misunderstandings, and provide information on the next steps in the care plan | 2 | (14, 41) | |
| Establishing proper communication in the announcement team | 3 | (14, 31, 40) | |
| Maintaining, strengthening, and communicating effectively with the patient and family | 3 | (20, 30, 37) | |
| Coordination and referral to other support resources | 5 | (14, 20, 41, 42) | |
| A bridge between patient, family, and service providers, facilitating the patient's cultural needs | 1 | (20) | |
| Facilitating family presence at the patient's bedside | 1 | (42) | |
| Increasing families' trust in the information given | 1 | (20) | |
| Facilitating parent-to-parent support, suggesting how to inform other family members | 1 | (41) | |
| Helping to make a rational and informed decision to continue treatment | 3 | (33, 35, 42) | |
| Providing a translator, if necessary | 3 | (20, 37, 38) | |
| Manager | Announce bad news independently | 16 | (9, 12, 16, 18, 32, 33, 35, 36, 38, 43-47) |
| Preparing the patient, the family, and the environment for delivering the bad news | 13 | (5, 12, 14, 16, 18, 33, 35, 37, 41) | |
| Set up a scheduled meeting | 1 | (42) | |
| Organizing team members to deliver bad news | 4 | (12, 18, 20, 42) | |
| Preparation of all documents and documents related to the patient | 2 | (20, 42) | |
| Knowledge and confidence of the content discussed in the meeting | 1 | (42) | |
| Cooperation in the process of delivering bad news | 6 | (12, 16, 18, 32, 42, 46) | |
| Creating satisfaction and peace for the patient, avoiding unnecessary expenses, cooperating and participating in the treatment of the patient, | 1 | (38) | |
| Helping the patient manage the disease's consequences, providing guidance for adaptation and self-care, predicting and managing the reactions of the patient and family, Informing the relatives of the deterioration of the patient's condition or the news of the patient's death, explaining the process of care and dying, and care at the end of life | 2 | (32, 35) | |
| Addressing the cultural needs of the patient and family | 2 | (20, 42) | |
| Secrecy and privacy in delivering bad news | 2 | (20, 42) | |
| Minimizing the negative effects of bad news | 3 | (20, 32, 37) | |
| Frequent examination of the patient's condition, creating space and conditions for timely visits for the patient, providing comfort facilities in the last stage of the disease | (39) | ||
| Educator | Assessing patients' level of knowledge about the disease and its progress before providing information | 3 | (12, 14, 39) |
| Examining the need for hope and education about the quality of life, and communication between the patient and the doctor in the last stage of the disease | 1 | (12) | |
| Providing information about disease and prognosis and treatment measures | 12 | (12, 14, 16, 18, 20, 32, 35, 39, 41, 42, 46) | |
| Considering the preferences and values of the patient and the family in the educational content, creating an appropriate academic environment for information exchange, providing information in a calm and unhurried tone, maintaining privacy in providing information, and ensuring the understanding of the given information | 1 | (20) | |
| Teaching the patient's companions how to break the bad news to other family members | 1 | (42) | |
| Supporter and advocate | Emotional support for the patient and family | 20 | (5, 12, 14, 16, 18, 20, 30, 31, 33, 35, 36, 39-44, 48) |
| Giving hope to the patient, finding financial sponsors, talking about the possibility of death, creating an opportunity to be alone and cry, meeting with a religious person, consulting with the doctor about the patient's treatment, evaluating and getting to know the people visiting the patient, | 1 | (39) | |
| Consultation with the family about the whistleblower, support for asking questions of the doctor, advice for clarifying ambiguities, support in deciding to continue care, confirmation of emotional reactions | 2 | (14, 41) | |
| Supporting the family during suffering and mourning, defending the patient's independence and values, informing them about the potential risks of treatment | 2 | (20, 30) | |
| Accompanying the patient with sympathetic silence | 5 | (20, 31, 40, 42, 44) | |
| Transitional support to end-of-life care | 2 | (20, 35) | |
| Helping the patient and family to come to terms with the news | 4 | (14, 16, 18, 36) | |
| Social, physical, spiritual, and psychological support for the patient | 2 | (31, 40) | |
| Palliative care support | 1 | (20) | |
| Using therapeutic touch at the right time, conveying kindness and compassion | 1 | (42) | |
| Pay attention to the feelings expressed | 5 | (14, 39, 41, 42, 44) | |
| Answering questions related to the concerns of patients and families | 2 | (14, 39) |
The Roles of Nurses in the Process of Delivering bad News to the Patient and Family
2.4. Stage 4: Data Analysis
Ordered, categorized, and summarized data are obtained and used in an integrative review (11). The data were analyzed, using the constant comparison approach, which was chosen based on the purpose of the study and the nature of the included documents. Constant comparison, a well-known data analysis technique that aids in the methodical classification of data, consists of data reduction, data visualization, data comparison, conclusion formulation, and verification. Because the data included in integrative reviews come from a wide range of sources with different approaches, constant comparison is a suitable strategy for data analysis. This method involves continuously comparing and grouping collected data based on similarities, then summarizing and describing the results in the form of themes or categories (25, 28). To analyze the data, the first and second writers read over each included article in its entirety several times, chose relevant meaning units, and organized related meaning units in an orderly manner. Ultimately, every member of the research team evaluated, edited, and accepted the categories they had created.
2.5. Stage 5: Presentation
The initial search of databases and the manual search of resources by the first and second researchers yielded 990 articles, of which 537 were discarded due to duplication in 2 or more databases. The remaining 453 articles were examined in the second stage based on keywords, titles, and study summaries. Another 383 articles were removed due to being unrelated to the research objective, lacking full text, not being freely available, or being in other languages. In the third stage, the full text of the remaining 70 articles was read and examined in terms of the content inclusion criteria. After excluding 44 articles that did not meet the study criteria, 26 studies were included in the research. Of these, 6 were conducted in Iran and the remaining 20 were conducted in other countries. Figure 1 shows the PRISMA flowchart of the study (49).
3. Results
3.1. Studies Characteristics
The studies were published from 1980 to 2022. The specific year of publication, authors, country, design, and stated objective of the studies are summarized in Table 2. There were 6 reviews, 11 qualitative, and 9 quantitative studies included. They were conducted in England (n = 5), the USA (n = 4), Ireland (n = 2), Brazil (n = 1), Oman (n = 1), Israel (n = 3), Canada (n = 3), China (n = 1), and Iran (n = 6). A total of 22 studies were in English, and 4 were in Persian. The results show that delivering bad news is a team process, in which nurses play various important roles in 3 stages: Before, during, and after the bad news is announced. Findings regarding the specific roles of nurses in this process were described, summarized, classified, and reported (11, 25). In general, the key roles of nurses in this study were categorized into 4 main roles (manager, educator, facilitator, and supporter/advocate) and 74 subordinate roles (Table 3).
3.2. The Role of Nurses as Managers in the Process of Delivering Bad News
One of the important role’s nurses play in the process of delivering bad news is the manager. Nurses often face undue pressure in special and emergency departments, which highlights their independent role in delivering bad news (5, 12, 16, 45-47). Imanipour et al. found that 35% of nurses often independently deliver bad news to patients or their families (16), while this rate was 22.5% and 97.2% in studies by Warnock et al. (18) and Reinke et al., respectively (12). In the study by Mahasti Jouybari et al. (as cited by Imanipour), nurses reported delivering bad news via distant relatives (16). In Arbabi ett al., 74% of nurses disclosed the diagnosis to the patient or their family, but only 24% wanted to discuss life expectancy (47). Ben Natan et al. reported that 76% of nurses would inform their patients of bad news independently (45). According to Cheng et al., 81% of nurses cooperated with doctors in truth disclosure and providing disease information (46). Rayan et al. reported that the majority of intensive care nurses are involved in delivering news of a patient’s death, and 84.3% had a positive attitude toward conveying bad news (5). In a study by Clark and LaBeff, nurses independently announced the news of death, managed the emotional reactions of the recipients, and reduced the negative effects of the bad news (32). According to Rassin et al., 34.5% of nurses cooperated with doctors in announcing death news, and 27% also independently announced the news of death (43). Nurses are vital in preparing patients for death announcements, discussing resuscitation, medication, mobility equipment, preferred care locations, saying goodbyes, and preparing children (33). Nurses are vital in providing patients with essential support, including decision-making, discharge planning, self-care, reactions, predicting responses, end-of-life care, and informing relatives (35). Nurses communicate patients' truths to maintain trust, satisfaction, and comfort, avoid unnecessary expenses, encourage cooperation, and facilitate informed decision-making (38). Nurses exercise their management skills before the delivery of bad news by ensuring the right conditions, environment, and time for delivering bad news to the patient and their family (35). Confidentiality and privacy of the patient in announcing the news, being sensitive to the patient's cultural needs, providing an interpreter if necessary, coordinating with other team members, and cooperating with the doctor are other important roles (5). Ensuring the content discussed in the news announcement meeting, following up, and preparing all documents related to the disease, such as test results, pathology results, and photographs, setting up a pre-planned meeting, talking with the patient and family who would like to be present at the meeting, and coordinating their participation are other managerial roles of nurses in this process (42). The roles of nurses are effective communication with the patient and family, preparing the ground for delivering bad news, minimizing the negative effects of bad news, and helping the patient and family make rational decisions to continue treatment (37). Nurses manage patients' conditions, communicate changes to families, regularly check their condition, schedule visits, and provide comfort facilities in the final stages of disease (39).
3.3. The Role of the Nurse as a Supporter and Advocate in Delivering Bad News
Nurses support the patient and the family mentally and physically when delivering bad news. Emotional support was one of the most critical roles investigated in these studies (5, 12, 14, 16, 18, 20, 30, 33-36, 39-42, 44, 45). Therefore, the patient and the family put forth their most crucial need in conveying bad news emotional support (22). In Imanipour et al.’s study, 40% of nurses participated in emotional support for the patient and their family. Other supporting roles of nurses include helping the patient and family reconcile with the bad news and introducing them to other support groups (16). In Warnock et al.'s study, nurses' emotional support was 55.5%, helping to adapt after bad news was announced (47.7%) (18). This issue was mentioned in Imanipour et al., 14.3% always and 47.8% often (16). Joybari emphasized encouraging the patient and the family (16). The most common roles for nurses were related to providing emotional support to patients, such as acknowledging emotions like fear, silence, denial, and crying, and responding appropriately to these emotions when delivering bad news (5, 14). Nurses play an important role in helping patients understand and adjust to bad news, including answering questions, supporting decision-making, listening to emotional reactions, and creating opportunities for discussion after the news is announced and its consequences (14). Nurses provide support to families during illness, prevent complicated mourning, defend independence, and inform patients about treatment risks while promoting their values and protecting their independence (20, 30). Patients and families were allowed to express their feelings, accompanied by sympathetic silence and supported by cooperative sentences, praise, and encouragement (44). Peel highlighted the supportive role of nurses in patient care, including expressing hope, finding financial support, and dealing with feelings of death. They also ensured the comfort of the patient and consulted with the doctor (39). Supporting patients and families through the transition to end-of-life care was part of nurses' roles (35). Providing physical, social, emotional, and spiritual support to the patient, being the patient's advocate, assessing care needs, and accompanying the patient is part of the support duties of nurses in the process of delivering the news (31, 40). Nurses play a crucial role in patient care, providing emotional and practical support through empathy, observation, and identification of cognitive, behavioral, and emotional responses (42). Nurses should exhibit kindness and compassion through therapeutic touch, recognizing when to use it to prevent negative effects (42).
3.4. The Role of Nurses as Facilitators in Delivering Bad News
Nurses are crucial facilitators in delivering bad news, actively presenting, explaining information, answering questions, and listening to the patient's concerns, emphasizing the importance of their presence in such situations (34), allowing the patient and family to talk after giving bad news (55.9%), being with the doctor when announcing the bad news (39.1%), and answering the patient's and family's doubts about the bad news (36.5%) (18). Nurses provided explanations of doctors' words, were present when bad news was announced, and provided opportunities for patient or family discussion (40). The importance of examining patient status, identifying preferences, establishing communication, clarifying misunderstandings, explaining medical terms, and providing information about care plan stages were examined (14). Studies indicate that nurses with long-term patient contact establish a strong, reliable relationship, and actively participate in reporting bad news (20, 30). In addition, the presence of nurses during news delivery increases families' confidence in the provided information (20). Nurses often recognize patients' religious or spiritual needs after delivering bad news, referring them to resources such as ethics committees, religious counseling, social workers, psychotherapists, and cultural services, facilitating the process with communication skills and information (41). Nurses play a crucial role in facilitating cultural aspects for non-English-speaking patients, their families, and health service providers by organizing information in their preferred language (20). Nurses can assist families in providing crucial support to patients by facilitating their presence at their bedside (42). Nurses play a crucial role in healthcare by facilitating effective communication, delivering bad news, establishing therapeutic relationships, and maintaining trust through honesty (31, 40). Nurses, as part of a multidisciplinary team in patient care, play a crucial role in delivering bad news and ensuring effective communication (41).
3.5. The Role of Nurses as Educator in Delivering Bad News
Nurses are vital educators, assessing patients' and families' educational needs and providing crucial information about diseases, prognosis, treatment, and care paths, ensuring patient knowledge and quality of life (39). In Cheng’s study, 81% of nurses cooperate with doctors in providing disease information (46). Nurses offer patient education during bad news, focusing on their preferences and decision-making roles. They create a calm, unhurried space for information exchange (20). Explaining the process of care and dying is one of the duties of nurses (35). They also play an essential role in preparing educational packages about disease diagnosis, prognosis, and diagnostic and therapeutic measures based on the needs of the patient and family (41). Nurses gather patient and family information, understand their preferences, and support decision-making styles. They also aid in understanding patients' prognoses (20).
4. Discussion
In this study, we investigated the role of nurses in the process of delivering bad news by studying 26 articles from 9 countries. Delivering bad news is one of the most difficult tasks that healthcare professionals perform (50). According to the literature, physicians are responsible for delivering bad news, while nurses play an important role in assisting the physician and the care team (14, 18). The results of this study show that nurses have essential roles in delivering bad news and acting as managers, educators, and patient supporters. Their role continues throughout the care pathway, from diagnosis and treatment to rehabilitation and, ultimately, death. This process can span long periods and involve multiple interactions with the patient and their family.
The diverse roles of nurses highlight the complexity of their responsibilities, and each of them faces many challenges. On the other hand, the realities of the health system show that the role of nurses in delivering bad news is not fully confirmed (20). One of the responsibilities of nurses in a managerial role was to prepare patients and their families to receive difficult news. McSteen and Peden-McAlpine also emphasized this role in their study (51). Another important responsibility of nurses is independently delivering bad news in their managerial role. In most countries, it is the doctor's responsibility to announce bad news, but in certain circumstances, nurses may find themselves in a position where they need to inform the patient and their family independently. Nurses in the intensive care and emergency departments have independent managerial responsibilities when it comes to delivering bad news, given the specific circumstances (22). Of course, in the study by Arbabi et al., only 2% of nurses inform the patient or their family about the diagnosis (47). The reason for this difference is in the research environment cancer patients with chronic conditions need time to diagnose and make decisions about the disease. When doctors are not available and circumstances are such, they cannot delay BBN (24) Effective communication between nurses and patients, the management of conditions, uncontrolled incidents, and the anticipation of reactions when delivering bad news are critical (52).
In this study, one of the most vital roles of nurses is to support and defend patients and their families in the process of delivering bad news. The results of a study show that patients' need for information and support goes beyond the delivery of bad news and that nurses who spend more time caring for patients actively support this process (8). The important point is that paying attention to the emotional needs of patients and caregivers is an essential part of the role of nurses. Additionally, treatment planning not only helps patients live fulfilling lives but also assists families in accepting difficult news (13). The critical point is that the patient and the family express emotional support as their most crucial need in conveying bad news (22). Nurses prioritize the emotional needs of patients and strive to fulfill their role with higher quality (53). Nurses play a crucial role in discussing the end of drug treatment and establishing plans for supportive and palliative treatments (10, 54). Emotional support and helping patients express their emotions and feelings were among nurses' important activities in delivering bad news (17). Nurses can assist patients with new cancer diagnoses by connecting them with palliative care and pain service providers, while also incorporating their religious or spiritual beliefs for support (20). Nurses can assist patients with spiritual care, psychosocial needs, and family presence in the inpatient setting, identifying and addressing the unique needs of each patient (55). In the study of Mitchell, nurses must control patients' and families' expectations and react suitably to their emotional outbursts (56).
In this study, nurses played a vital role in facilitating the delivery of bad news. Studies have listed various tasks for nurses' facilitation roles that nurses must perform when BBN to patients, including providing and clarifying information and helping patients understand (57, 58). In this process, nurses explain the doctor's words to the patient in simple language. Dennis and Slevin emphasized the need for the nurse to be with the patient who receives bad news (34). Yazdanparast et al. has highlighted the crucial role of nurses in providing information in a simple and understandable language (59). McCulloch's study found that 90% of patients rate the presence of a clinical nurse as the most valuable person when receiving bad news (10). Patients and families often turn to nurses for additional information or to restate bad news (60). Nurses facilitate by ensuring the patient's psychological well-being and evaluating their medical history along with doctors (12). Patients always look to nurses for clarification on questions from doctors, as they may not fully understand the situation or require immediate clarification (8). Matthews et al. have emphasized that nurses play a facilitating role in establishing effective interpersonal communication and ensuring the accurate transfer of information (61). After patients receive bad news, nurses improve communication between patients and their families to ensure that the correct diagnosis, prognosis, and treatment options are made available (62). Nurses play a crucial role in facilitating cultural aspects that are vital for effective patient communication. Additionally, nurses can emphasize the cultural norms that influence a patient's comprehension of disclosure.
One of the other important roles of nurses in this study was to educate the patient and their families about the disease condition and care pathways. This education helped them make informed decisions regarding their current conditions. Nurses are essential in informing patients and families about diseases, prognosis, treatment, and care pathways, assessing educational needs, and providing vital information. The nurse is legally obligated to educate the team responsible for delivering bad news, quality improvement, evidence-based care, and patient safety (63), which was similar to the results of this study. Nurses can enhance mental health care by addressing patients' concerns, identifying their information needs, and responding appropriately to help those with clinical depression or anxiety (64). Nurses can effectively utilize their knowledge to educate patients about potential health issues (65). Because of the specific and unpredictable clinical conditions, they have numerous opportunities to communicate with patients and assess their needs (16). Nurses are the primary care providers, having immediate access to patient information and the most time and contact with patients (12). Nurses' role in patient education during disclosure is significantly related to their satisfaction with care. Therefore, the role of education in promoting patient independence, informed decision-making, and respect for their position is crucial.
Nurses play a crucial role in delivering bad news, but they face numerous challenges in their process (13). Over one-third of nurses express a lack of awareness and knowledge to effectively deliver bad news, despite their positive attitude (66). Most of the nurses express dissatisfaction with the presentation of bad news, which indicates the need for training courses and interventions to support them (67). Shomoossi et al.'s study revealed that 71.2% of nurses did not receive training, 28% acquired it experimentally, and 99% were unaware of the standard strategy for announcing bad news (23). Most of the nurses behave tastefully based on their mentality, which can create challenges in interacting with patients from different social and cultural backgrounds (16) that delivering bad news is a crucial clinical skill for health system employees, particularly doctors and nurses (68). Ignoring this leads to a decrease in the quality of care and a lack of trust in medical staff when delivering bad news (38). Meanwhile, the role of nurses should be adjusted to align with patient preferences and values to minimize ethical gaps in delivering bad news, enhance the quality of care, and foster trust (20). When having difficult conversations, nurses can make sure they cover all the bases by using a framework (56).
4.1. Conclusions
Nurses play an important role in the process of delivering bad news, acting as educators, facilitators, supporters, and managers in their interactions with patients and their families. Despite the numerous challenges that nurses encounter, acknowledging and enhancing their role can promote ethical care and alignment with patients' preferences and values. Nurses require diverse skills, specialized knowledge, professional communication, and standardized guidelines to mitigate the adverse effects of delivering bad news.
4.2. Strength and Limitation
The results of this study highlighted the various roles of nurses in the process of delivering difficult news. However, there were limitations to this study. It was limited to English and Persian, which may have resulted in the exclusion of other relevant articles. Additionally, a qualitative analysis was conducted on the aforementioned desired outcomes.
4.3. Recommendation
- Healthcare organizations should prioritize the training of nurses clearly define their duties and provide legal and psychological support to prevent the complications of BBN.
- Nurses must manage patients' emotions and establish interpersonal interactions. To overcome obstacles and deliver bad news with confidence, they can use tactics such as training, communication skills, support resources, and standard protocols. All of this equips nurses to better serve patients and families.
- This study provides valuable insights for designing clinical guidelines, defining job descriptions, and making sound decisions for health policymakers. It can be used in future studies.
- The results of the present study highlight the need for support and training among nurses. This will enable them to utilize the most effective methods and strategies in this process, and adequately prepare themselves to face such situations.