1. Introduction
Bladder cancer is the tenth most prevalent cancer in the world, with a global incidence of 2.4 cases per 100,000 person-years for women and 9.5 cases per 100,000 person-years for men, according to recent studies. Urothelial carcinoma of the bladder accounts for approximately 90% of all bladder cancers. It is concerning that muscular invasive bladder cancer (MIBC), is now being diagnosed in 30 - 40% of these cases (1, 2).
Radical cystectomy (RC) with urinary diversion is the standard treatment for invasive bladder cancers, including MIBC. However, due to the increased incidence of bladder cancer in older adults and the associated comorbidities, RC surgery can be dangerous in some high-risk cases. In these situations, chemotherapy can be a viable alternative option. However, it's essential to carefully select patients for chemotherapy based on their individual circumstances and to provide them with appropriate pre- and post-treatment care (3).
The main objective of discussing this patient was to clarify the circumstance where they would gain advantages from undergoing orthotopic radical cystectomy surgery, but their physical condition is unfit to withstand the extended duration of the procedure. In this specific case, the patient presented with uncontrollable hematuria. Due to his comorbidities, he was not a good candidate for RC with general anesthesia, which is the standard treatment for MIBC. Instead, a two-stage RC with orthotopic neobladder urinary diversion was performed.
2. Case Presentation
The patient, a 61-year-old heavy smoker, was referred to the emergency department due to severe gross hematuria. Notably, the patient had a history of bladder cancer, having undergone four transurethral resection of bladder tumor (TURBT) procedures in the previous two years. The most recent TURBT specimen revealed tumor invasion into the muscularis propria (at least pT2), as reported by the pathology team.
Written informed consent was taken from the patient in accordance with ethical considerations.
Due to the patient's medical history of chronic obstructive pulmonary disease (COPD) and ischemic heart disease (IHD), he was not a suitable candidate for RC surgery.
During the physical exam, the patient appeared pale, and had an increased heart rate. Blood pressure was normal and no obvious mass was palpated in the abdominal examination. Initial lab results revealed a hemoglobin level of 8 g/dL, creatinine level of 4.2 mg/dL and Prostate-specific antigen (PSA) level was 0.90 ng/mL. The patient had a history of intravesical injections of Bacillus Calmette-Guerin (BCG), and his medications included aspirin, atorvastatin, and Seroflo spray.
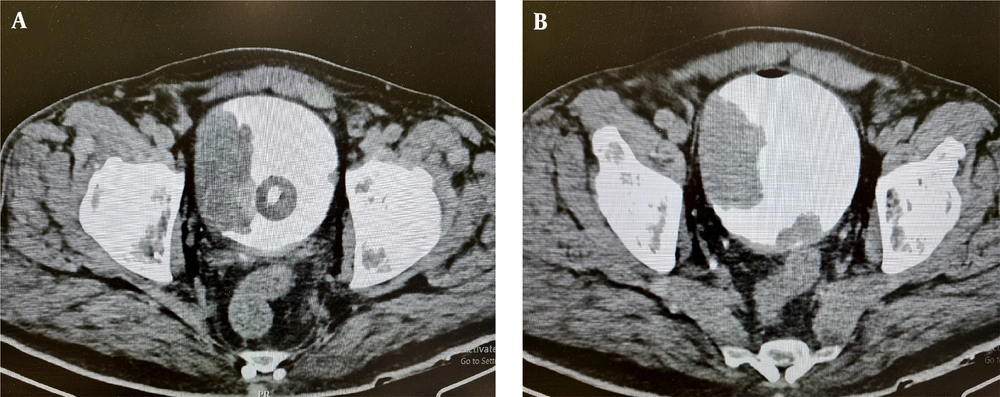
An ultrasound revealed moderate to severe hydroureteronphrosis on both sides. A computed tomography (CT) cystography revealed a substantial bladder tumor extending from the bladder dome to the right lateral wall (Figure 1). Simultaneously, bladder irrigation was performed while infusing one packed cell unit.
During the cystoscopy, a vegetative tumor with dominance on the right lateral bladder wall, extending from the dome of the bladder to the bladder neck while covering both ureteral orifices, was seen. It was not possible to resect it during the procedure. Instead, we fulgurated the tumor in the bleeding areas and inserted bilateral nephrostomy tubes.
After 12 hours, the patient experienced a recurrence of gross hematuria. Four days later, the patient's creatinine level decreased to 1.2 mg/dL. The patient underwent a CT scan of the abdomen and pelvis with both oral and intravenous contrast, as well as a CT scan of the chest. These scans did not reveal any signs of metastasis.
Due to the persistence of hematuria, the healthcare team prepared the patient for a RC procedure. Based on the patient's clinical conditions, it was determined that general anesthesia was not a viable option. As a result, the patient underwent spinal anesthesia for the extraperitoneal RC surgery. Additionally, bilateral cutaneous ureterostomies were performed. After five days, the patient was discharged from the hospital. The pathology report of the patient after surgery was pT2N0M0. The patient was advised to undergo adjuvant chemotherapy. However, despite the recommendation he chose not to proceed with the treatment.
He was referred to a cardiologist and underwent coronary angioplasty. The healthcare team scheduled the second stage of the surgery for one year after the patient completed the anticoagulant treatment.
After the patient's cardiac and pulmonary conditions were stabilized, he was candidate for second surgery. During the procedure, we created an orthotopic pouch using a section of the patient's ileum. The ureters were then anastomosed to the neobladder. During one-year follow-up of the patient, there were no evidences in favor of recurrence or metastasis.
3. Discussion
Marshall and Whitmore were pioneers in defining the surgical principles of radical cystectomy (RC) in the 1940s, although the first documented cases of RC can be traced back to the early 1900s (2). Today, RC is a critical component in managing high-grade bladder cancers, known as MIBC. Despite advancements in technology and patient care, open RC (ORC) still carries significant rates of perioperative complications and mortality, with population studies reporting a 90-day mortality rate ranging from 5.1% to 8.1%. Elderly patients with multiple comorbidities are at a higher risk of complications following surgery (3, 4).
In 2015, a randomized controlled trial by Bochner et al. compared the outcomes of robot-assisted radical cystectomy (RARC) with those of standard ORC and found that there was no significant difference in terms of major complications or pathological outcomes between the two techniques (5). It is noteworthy that not all medical centers have the necessary resources to perform RARC, which may limit its widespread adoption.
In this case report, we presented a patient who was not a suitable candidate for orthotopic neobladder RC due to comorbidities. As bladder preservation was not a feasible option (due to the size of the bladder tumor and uncontrollable bleeding), we decided to perform RC in two stages to avoid the complications of general anesthesia and shorten the operation time. This approach allowed for the construction of an orthotopic neobladder during the second stage, which provided the patient with the benefits of this type of urinary diversion, such as avoiding the long-term complications of cutaneous ureterostomy and improving his quality of life. It is worth mentioning that the studied patient declared his satisfaction with the result of the surgery with a one-year follow-up period.
The strength of this study lies in its novelty and the fact that it hasn't been done in other studies. However, its limitation is the inability to perform it in some patients due to the formation of adhesion bands after the initial surgery.
The key takeaway from this study is that if a patient is a candidate for radical orthotopic cystectomy surgery but cannot tolerate it for an extended period due to their physical condition, the surgery can be conducted in two stages. In general, it seems that performing RC in two stages can help to decrease surgical complications while still allowing the patient to benefit from urinary diversion using an orthotopic neobladder.