1. Introduction
Ganglioneuroma (GN) is a rare, benign neurogenic tumor that can grow to a large size without causing symptoms (1). It develops from cells in the sympathetic nervous system and is a specific type of peripheral neuroblastoma that its histological characteristics can identify. The incidence of GN is reported to be one per million population, often occurring sporadically but with a familial predisposition (2). Ganglioneuromas are typically benign tumors that grow slowly and can occur at any age, with a higher frequency in children over the age of 10 (3).
Ganglioneuroma can occur in any location where peripheral autonomic ganglion cells are present, but it is most commonly found in the posterior mediastinum and retroperitoneum (4, 5). Less common locations include visceral and cranial nerve ganglia, parapharyngeal and retropharyngeal regions, and the adrenal medulla (6).
Although ganglioneuroma is more common in children, its retroperitoneal form has been reported in adults. This type typically has a slow growth and a good prognosis, and is treated with surgery (7). Ganglioneuroma is usually discovered incidentally, but sometimes it develops following the treatment of neuroblastoma with chemotherapy and radiotherapy (8).
Several studies have mentioned that ganglioneuroma can release catecholamines, which can cause a sudden increase in blood pressure during surgery due to the release of catecholamines into the bloodstream (9).
It should be noted that although ganglioneuroma does not have a distinctive appearance in imaging, it is difficult to distinguish it from other tumors, and a definitive diagnosis is only possible with the pathology of the tumor after surgery and removal of the mass (10, 11).
There is a lack of comprehensive reports detailing the clinical, radiological, and pathological characteristics of GNs. This study aimed to raise awareness among clinicians about the possibility of these tumors occurring in unusual locations. We presented a case involving a 12-year-old boy who experienced dyspnea and had thoracoabdominal involvement due to a ganglioneuroma. A significant aspect of this case is the simultaneous involvement of both the chest and abdomen, as well as the size of the mass.
2. Case Presentation
The 12-year-old boy was referred to Abouzar Hospital in Ahvaz with complaints of cough, cold, and shortness of breath. His family history was negative. Hematological and biochemical laboratory tests were within normal limits. Additionally, alpha-fetoprotein, beta human chorionic gonadotropin (HCG), lactate dehydrogenase (LDH), Metanephrine levels in serum and urine were checked before surgery, and all parameters were normal. The study adhered to ethical guidelines by acquiring informed consent from the parents of each participant.
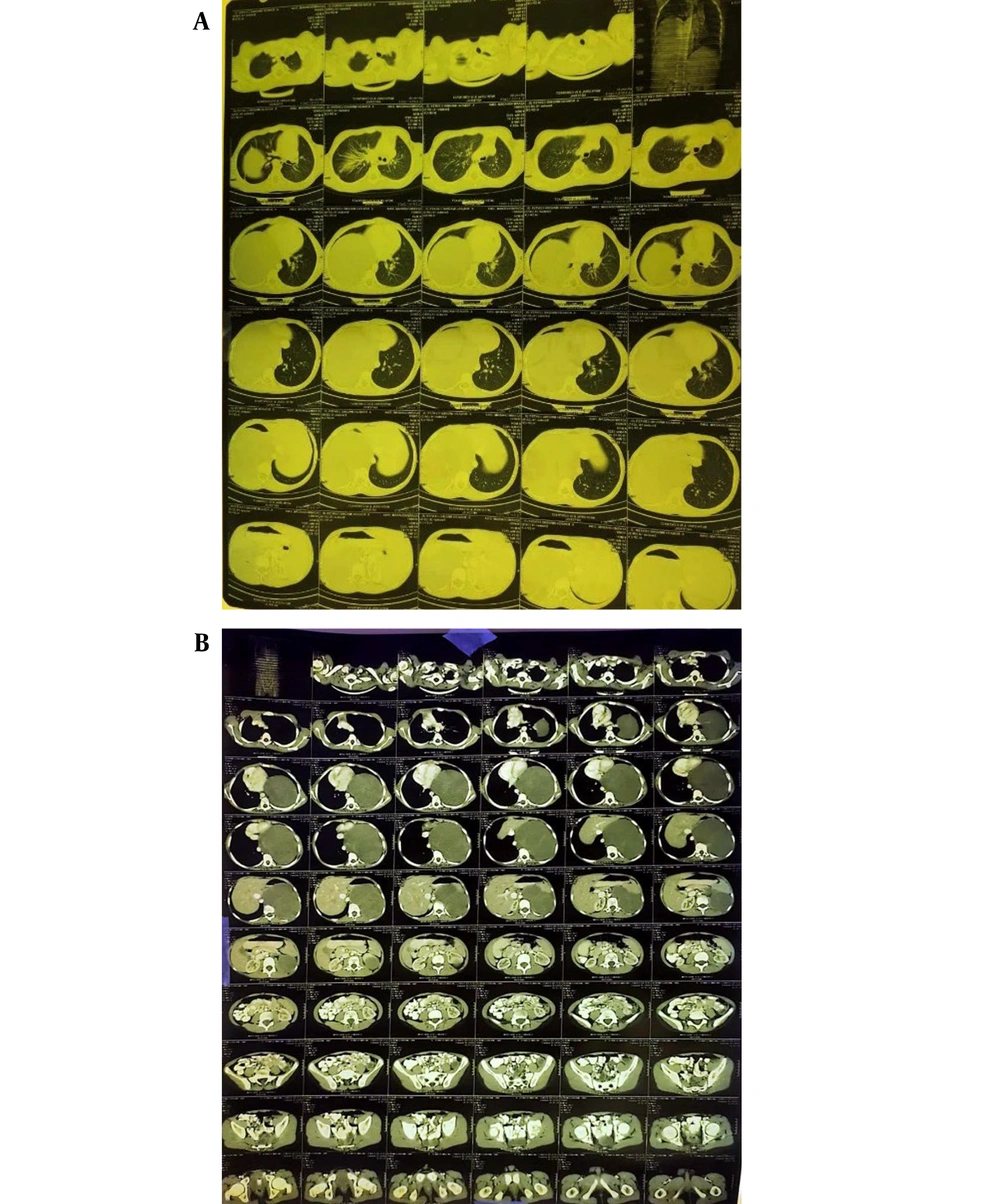
The patient underwent chest radiography which revealed a huge mass on the left side of the chest, causing the heart to shift to the right side. Echocardiography and Spiral Chest CT scan were performed for further investigation (Figure 1A). Additionally, abdominal and pelvic CT scans showed a heterogeneous hypodense mass measuring approximately 135 × 105 mm in the left upper region. This mass caused severe deviation of the heart and mediastinum to the right side, elevation of the left hemidiaphragm, and downward displacement of the left kidney (Figure 1B). The mass was suspected to be a benign lesion of adrenal origin. Ultrasounds of both testicles showed normal size and position.
Samples were sent to the laboratory for pathology examination. The biopsy report indicated a large heterogeneous area in the left half of the abdomen and thorax, extending near the upper part of the left hemithorax. A core needle biopsy confirmed a diagnosis of ganglioneuroma (it was performed by a radiologist). The mass was located in the retroperitoneum and did not move with breathing. The patient had not received chemotherapy or radiotherapy administered before the operation.
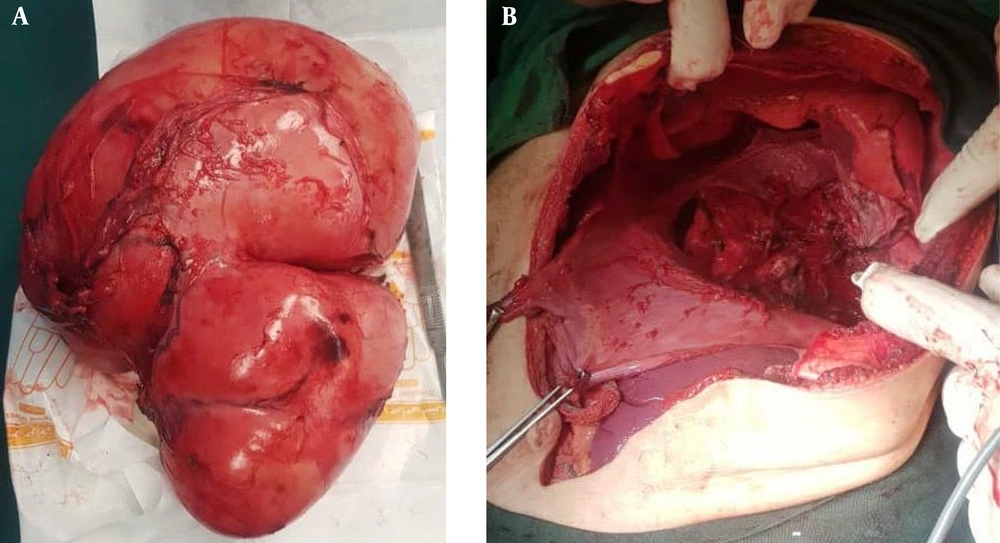
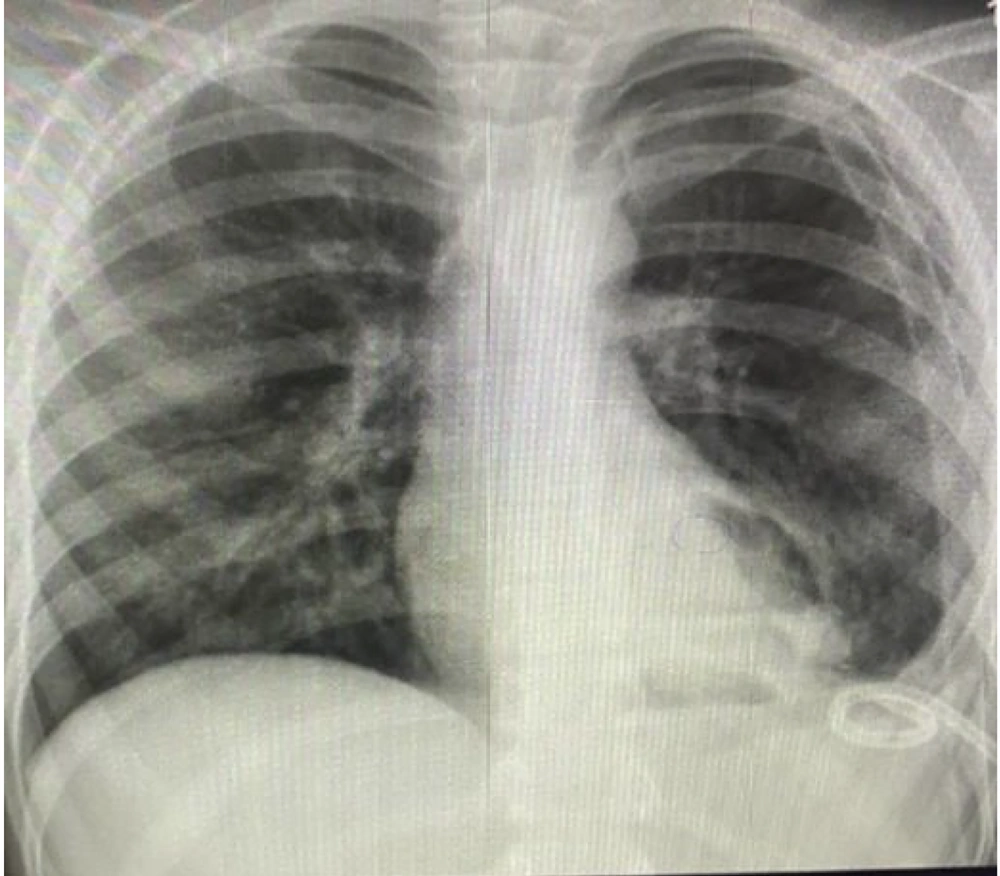
The patient then underwent surgery performed by a pediatric surgeon, a thoracoabdominal incision was Initially made, starting at the sternum and extending to the left fourth intercostal space. Most of the mass was located in the thorax, putting pressure on the diaphragm. The mass was strongly attached to the pericardium, parietal pleura, and spine. It was carefully separated from these structures, including the pericardium, thoracic, and abdominal vertebrae, and then resected (Figure 2). Following successful treatment, the patient was discharged in good overall condition (Figure 3). The patient was followed up in the first week and month following the operation with chest X-rays, and in the third and sixth months with a CT scan of the chest, which showed normal results.
3. Discussion
Ganglioneuroma is a benign tumor with slow growth that originates from nerve cells, including sympathetic ganglia. This tumor is composed of ganglion cells, neurons, Schwann cells, and fibrous tissue (12). Ganglioneuroma is usually asymptomatic; however, in cases where the tumor is large, retroperitoneal ganglioneuroma can cause the abdominal pain, palpation of the mass during abdominal examination, and compressive effects on the surrounding organs (9). This tumor is typically non-secreting, but in some cases, it can cause the secretion of substances such as catecholamines, leading to a hypertensive crisis during surgery (10).
In a study by Nugraha and Hernowo a case of mediastinal ganglioneuroma was reported in a 3-year-old child who presented with shortness of breath (1). Kizildag et al. reported a 19-year-old female with ganglioneuroma of the right posterior mediastinum. She presented with lower back pain and dyspnea (13).
In the study by Haghighi et al., a five-year-old boy with retroperitoneal ganglioneuroma complained of abdominal pain (9). Additionally, Singh et al. reported a case of retroperitoneal ganglioneuroma in a patient who presented with painless swelling in the left upper abdomen (8).
Among the various imaging methods for detecting abdominal and retroperitoneal masses, CT scan and MRI are considered the most effective. In sonography, the lesion typically appears as a homogeneous and hypoechoic mass (14). While the visual appearance of ganglioneuroma may not be as distinctive in MRI as it is in CT scans (15), in our case, a heterogeneous hypodense mass measuring approximately 135 × 105 mm was observed in the left upper region based on abdominal and pelvic CT scans. Singh et al. also utilized CT scan and sonography to diagnose ganglioneuroma, with the ultrasound scan revealing a hypoechoic ganglioneuroma and the CT scan showing a hypodense lobular mass (8). Similarly, in the case described in Haghighi's study, the retroperitoneal mass was diagnosed using CT scan and sonography (9).
CT scan is commonly employed for evaluating tumors, as it can show the extent of the tumor, regional invasion, vascular encasement, adenopathy, and calcification (2).
According to studies, over 30% of patients with ganglioneuroma experience an increase in urinary and plasma catecholamines, but only a few exhibit symptoms of this elevation in vasoactive amines (1), which was not the case with our patients. Similar to our situation, studies by Paasch et al. and Haghighi et al. did not report any increases in catecholamines (5, 9).
However, some patients with ganglioneuroma do have higher levels of catecholamines, such as vanillylmandelic acid or homovanillic acid (2). For a definitive diagnosis of ganglioneuroma, needle aspiration is typically used (2). Similar to the study by Haghighi et al. (9), needle aspiration was also used for the definitive diagnosis in our case. Surgical removal of the tumor is the standard treatment for ganglioneuroma, if possible. Chemotherapy or radiation therapy before or after surgery is usually unnecessary unless ganglioneuroma is associated with ganglioneuroblastoma subtypes (8). The prognosis for ganglioneuroma is generally good, as it rarely becomes malignant or spreads. While local recurrence is uncommon, it is still recommended to undergo radiologic surveillance after resection (1).
In the case reported by Haghighi et al., definitive treatment was performed with laparotomy surgery, and a definitive diagnosis was also made through pathology. During follow-up, there were no signs of tumor recurrence (9). Additionally, Paasch et al. utilized the laparotomy method to treat a patient with retroperitoneal ganglioneuroma (5).
Ganglioneuroma is a benign tumor originating from ganglion cells, typically found in the posterior mediastinum and retroperitoneal area. It is often asymptomatic. This report details a patient presenting with shortness of breath who was diagnosed with mediastinal ganglioneuroma. The preferred treatment for ganglioneuroma is surgical removal of the mass. Following complete removal, chemotherapy and radiotherapy are not typically necessary. This study underscores the importance of imaging in evaluating ganglioneuroma as a posterior mediastinal tumor.