1. Background
Breast cancer (BC) is a common and potentially life-threatening disease that have affected millions of people worldwide (1). Breast cancer is a multifaceted disease with complex causes and different manifestations, which makes it a major global health concern (2, 3). In 2022, BC caused 670 000 deaths worldwide and 2.3 million women diagnosed (4).
There are different reports about the incidence rates of BC in Iran. According to the national databases, age-standardized incidence rate (ASIR) for BC in 2012 was 33.21 per 100,000 (5). Another study in 2016 reported an ASIR of 40.72 per 100,000 women (6). The study of the national and subnational burden of breast cancer in women and men in Iran from 1990 to 2019 showed that the ASIR among women in 2019 was 34.0 (30.7 - 37.9)/100,000 and from 0.2/100,000 (0.2 - 0.3) to 0.3/100,000 (0.3 - 0.4) among men (7).
Previous studies indicated an improvement in the overall survival rate of these patients in recent years (the 5-year survival rate increased from 71% in 2011 to 80% in 2019) (8). Despite significant advances in BC research and treatment, several challenges remain. These challenges include late-stage diagnosis in low-income countries, limited access to health care and screening facilities, and high treatment costs (9-13). However, ongoing research efforts are expanding our understanding of BC and paving the way for innovative approaches to prevention, diagnosis, and treatment.
Measuring and monitoring health system costs will help health system policy makers in choosing appropriate policies to support patients. The amount of out-of-pocket (OOP) payments by households and the consequent catastrophic health expenditure are two important factors that must always be taken into account in the calculations related to the planning and policy making of health services (14). The financing of the health system in Iran is based on a multiple model including public budget, social, private and supplementary insurances, and a large share of health expenses is provided through direct household payments (15). The statistics of the National Health Accounts indicated that 55% of the resources of the health sector are provided in the form of direct payments during illness, and about 3.3% of the country's families are facing catastrophic health expenditure (16).
Out-of-pocket is one of the methods of financing the health system in both developed and developing countries. This method is the most inefficient method of financing the health system and is an incomplete mechanism for risk pooling (17). According to the latest data from the World Health Organization (WHO), the percentage of out-of-pocket expenditure as a fraction of the current health expenditure (CHE) in Iran decreased by 23% over 10 years, from 58% in 2011 to 35% in 2021 (18). The financial costs caused by BC and the effects of these costs on the financial status of the family may be one of the adverse consequences of this disease. Even if patients with breast cancer do not pay OOP for doctor's visits or surgical and auxiliary treatments received in the hospital due to having basic or supplementary insurance, they still have to bear the costs of transportation, treatments and follow-up visits, accommodation, purchase of equipment, prostheses, consultation with different doctors such as physiotherapists, and household help. Paying these expenses poses a challenge for many families and can lead to catastrophic expenses and impoverishment.
2. Objectives
Additionally, various factors affect the OOP payments of the families and patients with BC. Considering the importance of OOP payment and its continuous evaluation in order to monitor justice in the financing of the health system, we decided to conduct a study with the aim of investigating the OOP payment and the factors affecting it in patients with BC in Shahid Jalil Hospital, Yasuj University of Medical Sciences, Iran.
3. Methods
3.1. Design
This descriptive-analytical cross-sectional study was conducted in Shahid Jalil Hospital affiliated to Yasuj University of Medical Sciences in Iran. The target population of this study included all patients with breast cancer covered by the Iran Health Insurance Organization (IHIO) who had at least one hospitalization history in 2022.
3.2. Sampling
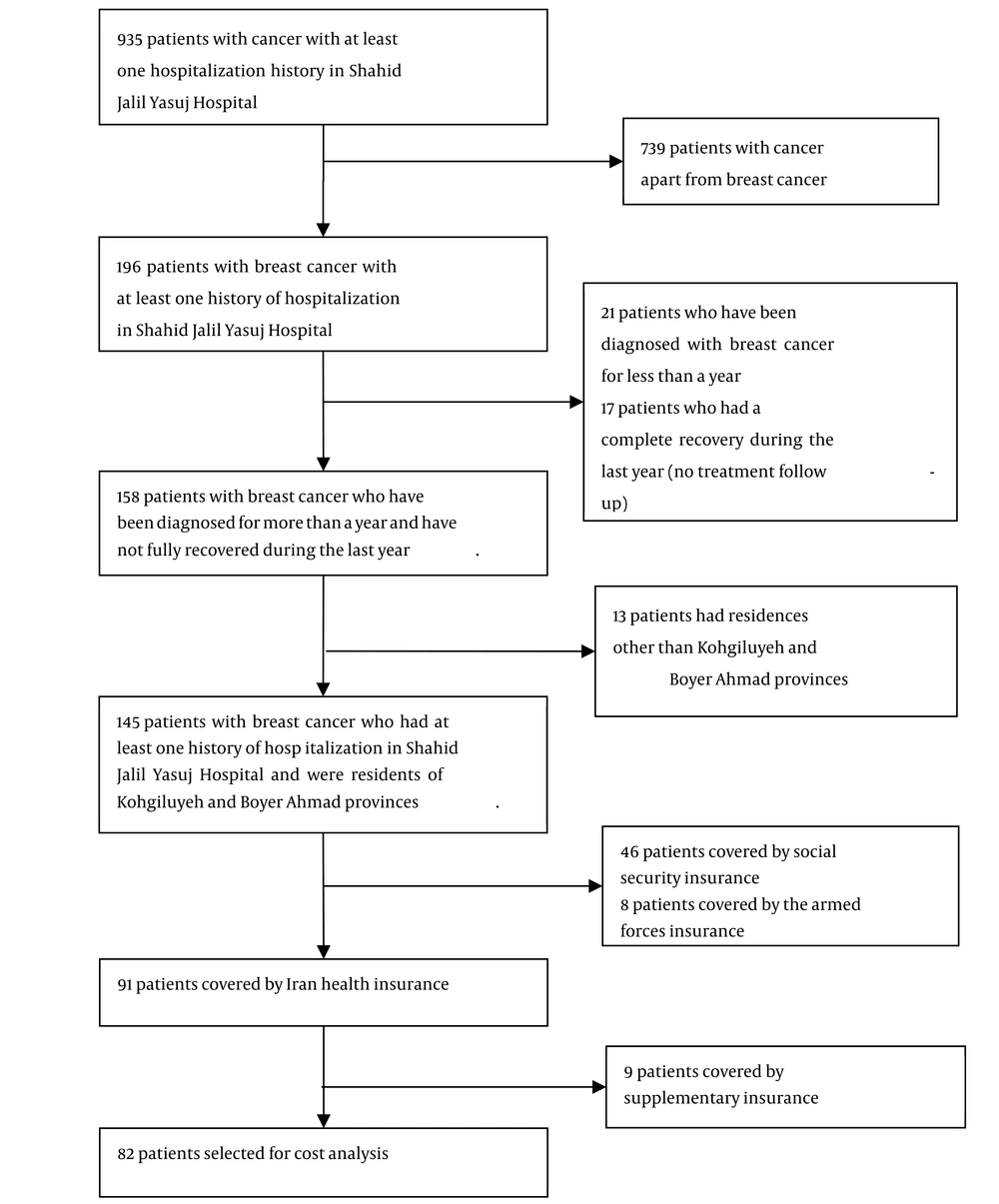
To determine the number of samples, firstly, the characteristics of all patients with cancer who had at least one hospitalization history in 2022 (N = 935) were collected. Then, patients with BC were separated from other patients, and 739 patients with cancer other than BC were excluded from the study. Out of 196 patients with BC who have been admitted to Shahid Jalil Yasuj Hospital at least once, 21 patients were excluded because less than a year has passed since their BC diagnosis, 17 due to complete recovery in the past year, 13 patients lived outside Kohgiluyeh and Boyer Ahmad provinces, 46 patients were covered by social security insurance, 8 were covered by armed forces insurance, and 9 were covered by supplementary insurance. Finally, 82 patients who were covered by the IHIO were selected to investigate OOP health expenditures (Figure 1).
3.3. Data Collection
The data collection tool in this study was a researcher-made checklist and the financial statement of patients in the hospital and the data of inpatients and outpatients of IHIO. The checklist made by the researcher included demographic characteristics and cost of treatment. Treatment costs are in the form of separate official (hospital bill) and unofficial payments for inpatient care, outpatient care, diagnostic tests, and treatment costs caused by illness for a period of a year was collected. This checklist was used after validating it by experts.
First, by referring to the discharge department of the hospital and checking the bill of patients' files in the IHIO, the cost data related to each patient was collected, and then to complete the checklist by calling the patient or the supervisor or a relative of the patient who responded. If the phone is inquiring, this form is completed. In this way, all OOP costs related to inpatient care, outpatient care, diagnostic tests, and drug costs due to illness were estimated for one year in the province. In this study, patients' OOP payments included two parts: Official payment (hospital bill and data from IHIO) and unofficial payment (fee paid by patients to receive services outside the insurance system), the total of which is as the amount of payment was taken OOP. The percentage of expenses paid by insurance organizations and the amount of expenses covered by government subsidies were also separately calculated for different hospital services.
3.4. Statistical Analysis
The data were analyzed using descriptive statistics methods including frequency, percentage, mean and standard deviation and multiple linear regression to investigate the effect of variables on the amount of OOP payments in SPSS 21 software. The dependent variable in the regression analysis of OOP payment and its independent variables were age, marital status, job, education, residence, household income, social coverage, and Housing situation.
4. Results
In this study, 82 patients with BC who had at least one hospitalization in Shahid Jalil Hospital were selected. The average age of the patients included in the study was 49.42 ± 9.59 years (min = 29; max = 77). Table 1 shows the demographic characteristics of the patients. Among the participants, 82.9% were married, 85.5% lived in the village, 92.7% were housewife, 46.3% received education at the elementary, middle, or high school level, 63.4% have a household income of less than 100 million Riyal, 54.9% were not covered by a social support organization, and 82% owned their personal belongings.
| Variables | No. (%) |
|---|---|
| Marital status | |
| Single | 3 (3.7) |
| Married | 68 (82.9) |
| Divorced | 4 (4.9) |
| Widow | 7 (8.5) |
| Residence | |
| Urban | 34 (41.5) |
| Rural | 48 (58.5) |
| Job | |
| Housewife | 76 (92.7) |
| Employee | 2 (2.4) |
| Free | 4 (4.9) |
| Education | |
| Illiterate | 27 (32.9) |
| Elementary, middle, high school | 38 (46.3) |
| Diploma | 11 (13.4) |
| Bachelor's degree | 5 (6.1) |
| Master’s degree and higher | 1 (1.2) |
| Household income (monthly) | |
| Under 100 million Rials | 52 (63.4) |
| Between 100 and 200 million Rials | 24 (29.3) |
| Above 200 million Rials | 6 (7.3) |
| Social coverage | |
| Lack of coverage | 45 (54.9) |
| Imam Khomeini Relief Committee | 28 (34.1) |
| State Welfare Organization of Iran | 9 (11) |
| Housing situation | |
| Rental | 22 (26.8) |
| Personal owner | 59 (72) |
| Organizational | 1 (1.2) |
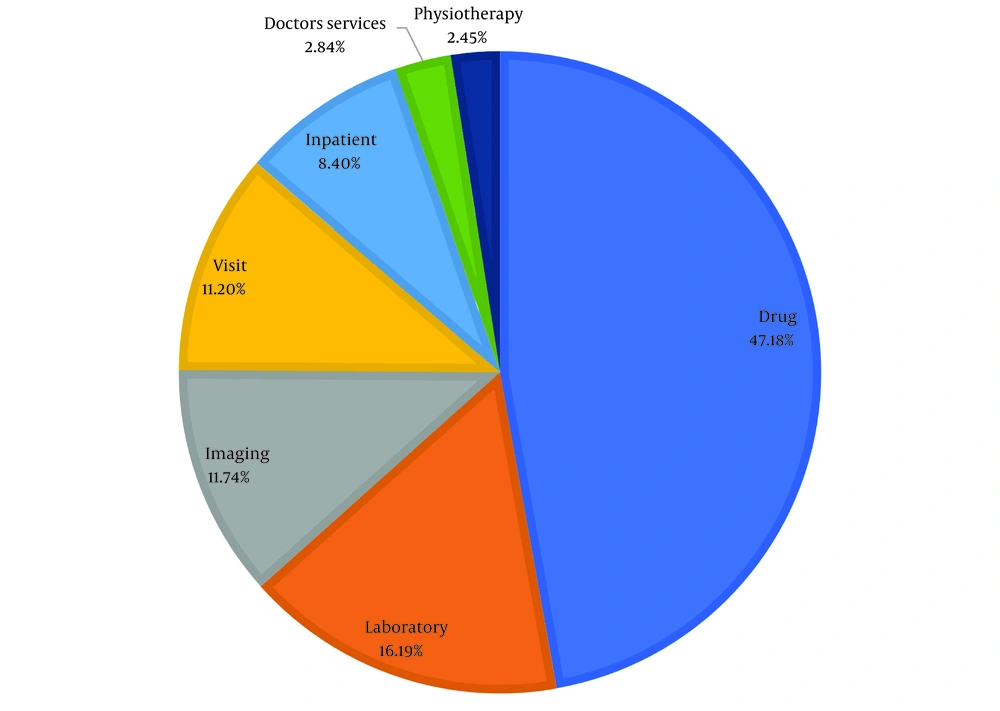
In Figure 2, the chart illustrates the breakdown of each service (outpatient and inpatient) as a percentage of the insurance coinsurance that patients pay. Of the out-of-pocket (OOP) costs, 47.18% were attributed to drug costs, 16.19% to laboratory costs, 11.74% to imaging costs, 11.20% to visit costs, 8.40% to hospitalization costs, 2.84% to doctor’s services costs, and 2.45% to physiotherapy costs.
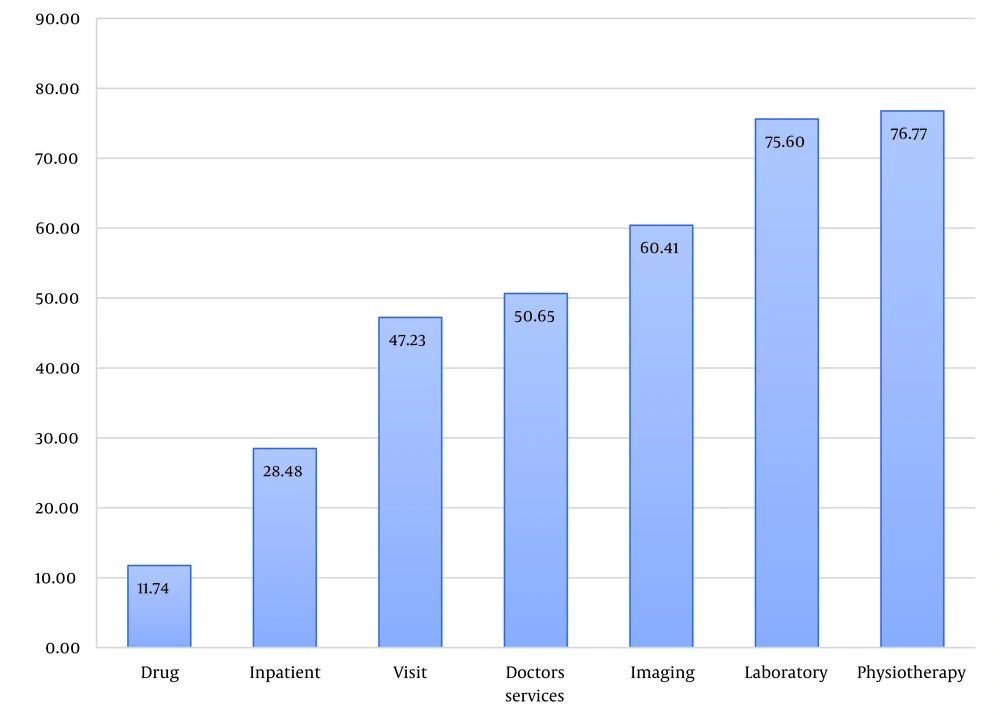
Figure 3 illustrates the percentage of costs paid by BC patients for each service, with IHIO covering other expenses.
The largest share of OOP of BC patients from the costs of each service was related to physiotherapy services at %76.77, laboratory costs %75.6, imaging %60.41, doctors' services %50.65, visits %47.23, Inpatient %28.48, and drug was %11.74.
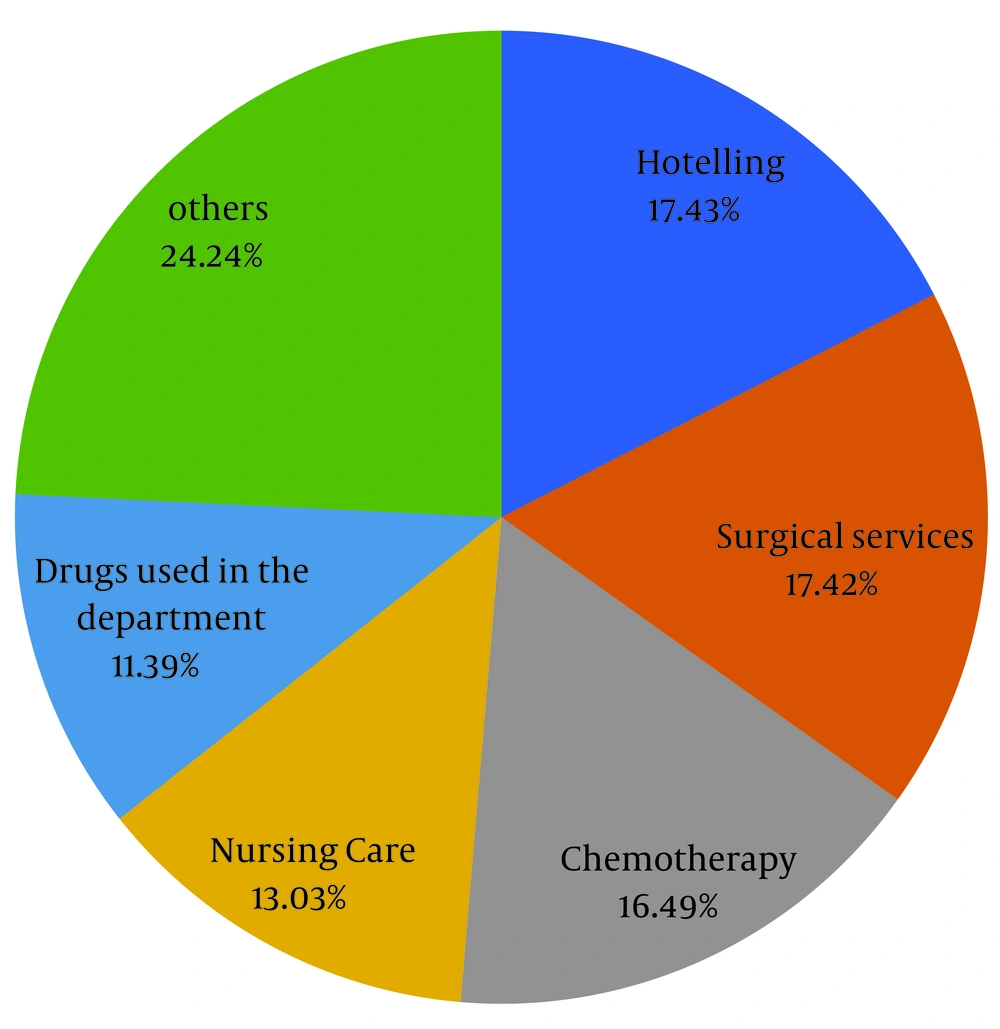
In Figure 4, the breakdown of inpatient costs by service is as follows: Hoteling costs accounted for 18%, surgical services for 17%, chemotherapy for 17%, nursing care for 13%, drugs used in the ward for 11%, and other expenses for 24%.
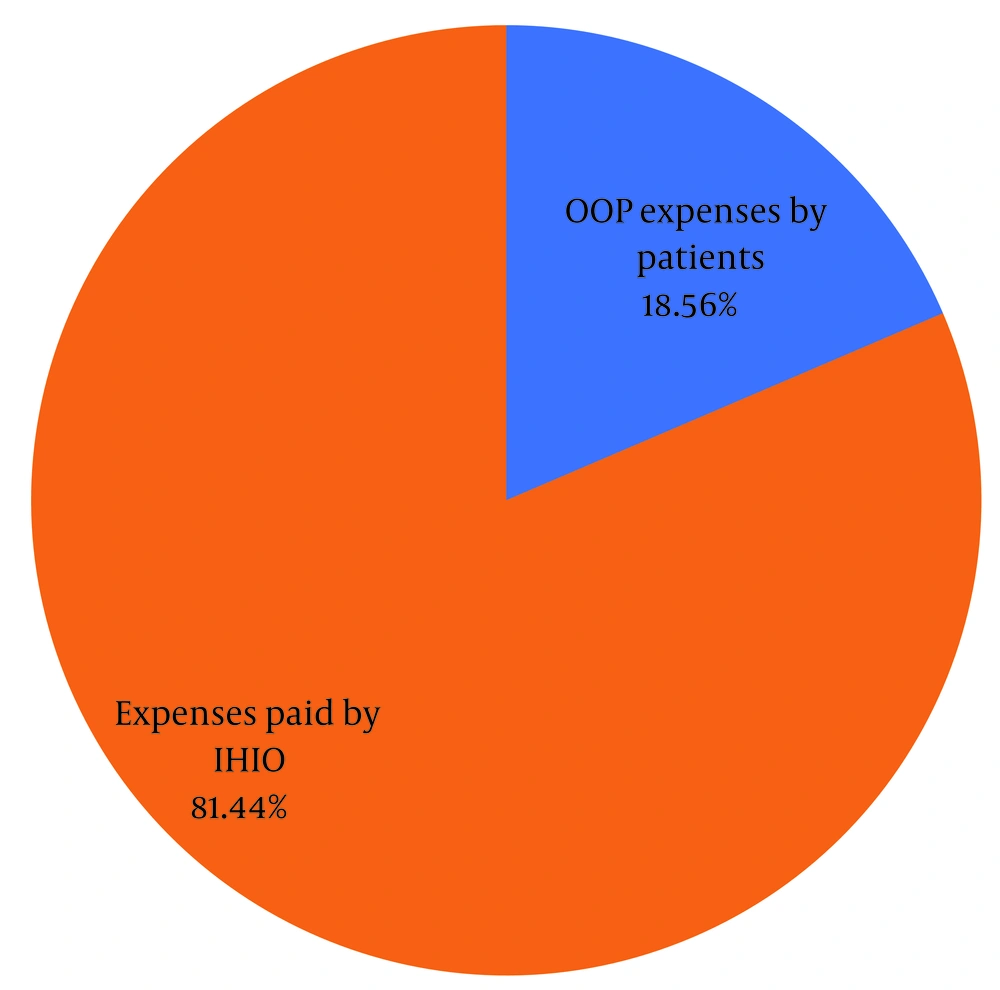
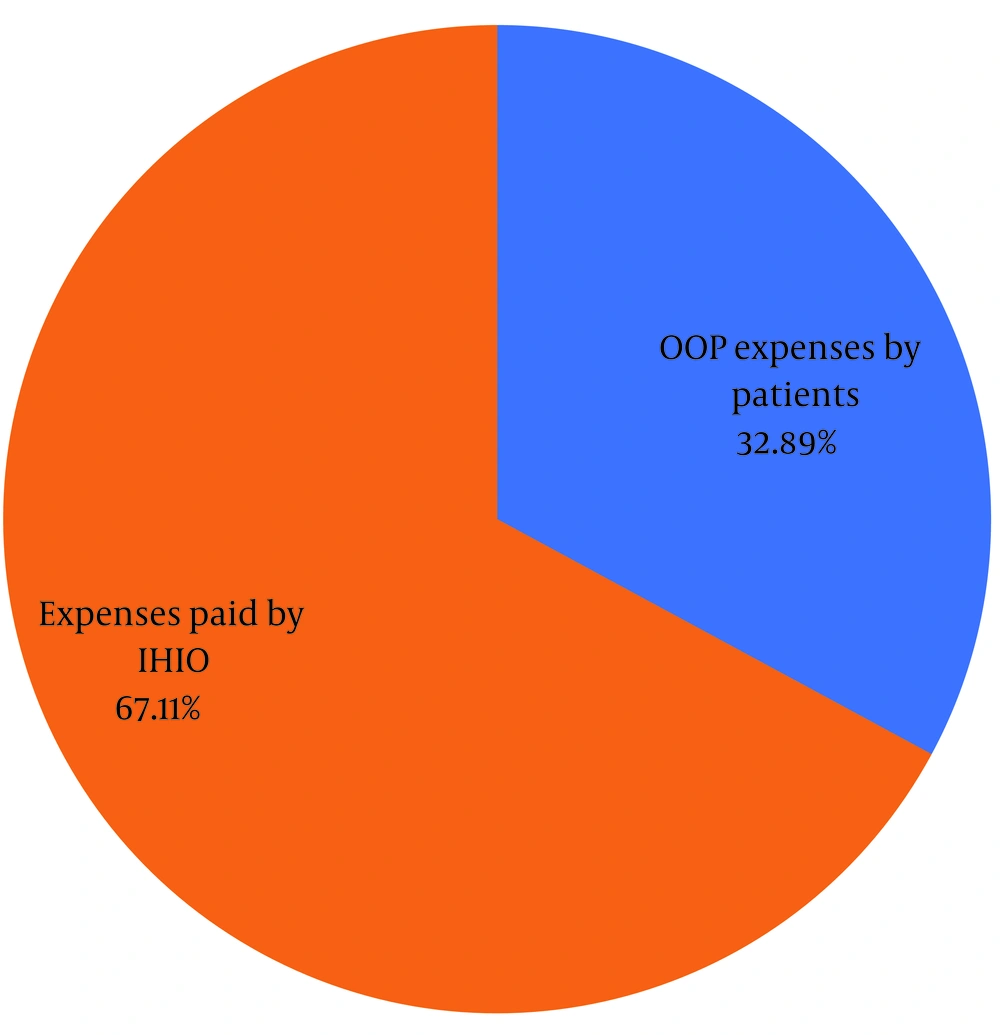
Figure 5 shows the share of OOP payments by patients from the total insurance costs based on the data registered by patients in IHIO and Shahid Jalil Hospital.
The share of OOP by patients from the total insurance expenses was 18.56%. Also, the IHIO has paid 81.44% of the total expenses of the patients.
Table 2 shows the expenses spent by IHIO, OOP (based on the data of Health Insurance Organization and Shahid Jalil Hospital), and expenses spent by patients out of the insurance coverage or indirect (based on the claimed data of the patients).
| Expenses | Amount (Rials) | Percent | Sum (%) |
|---|---|---|---|
| Expenses spent by IHIO | 26,203,102,351 | 67.11 | 67.11 |
| Expenses OOP by patients (based on the data of IHIO and Shahid Jalil Hospital) | 5,972,578,391 | 15.30 | 32.89 |
| Expenses spent by patients out of the insurance coverage or indirect | 6,867,854,985 | 17.59 | |
| Total | 39,043,535,727 | 100 | 100 |
Figure 6 shows the share of OOP expenses by patients from the total direct and indirect medical expenses of BC patients in Kohgiluyeh and Boyar Ahmad provinces in the year 2022. The share of OOP by patients from the total direct and indirect medical expenses was 32.89%.
Table 3 shows the estimation coefficients of the factors affecting the OOP payment of patients for direct and indirect medical expenses that are not covered by insurance (based on the patients' claimed data). According to Table 3, these costs include 17.59% of the total costs. Factors such as age, place of residence, job, education, and household income were among the factors that significantly affected OOP payments. In such a way that as the age increases, the OOP payment has decreased significantly (P = 0.030). The OOP payment of patients whose residences were urban was significantly higher (P = 0.032) than that of patients whose residences were rural. The OOP payment of patients who were self-employed was significantly higher (P = 0.008) than women who were housewives. Out-of-pocket payment of patients with higher education was significantly higher (P = 0.007) than women with lower education. Out-of-pocket payment of patients who had higher income was significantly higher (P = 0.001) than women who had lower income. Marital status, social coverage (relief and welfare committee coverage), and housing situation (rental, personal owner, organization) had no significant effect on patients' OOP payments (P < 0.05).
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | |
|---|---|---|---|---|---|
| B | Std. Error | Beta | |||
| Constant a | 153674000.993 | 300886517.362 | 0.511 | 0.611 | |
| Age | -8884756.118 | 4012924.894 | -0.258 | -2.214 | 0.030 b |
| Marital status | 18232940.519 | 55768255.278 | 0.034 | 0.327 | 0.745 |
| Residence | -153665002.154 | 70309216.876 | -0.239 | -2.186 | 0.032 b |
| Job | 193740235.609 | 70631807.394 | 0.280 | 2.743 | 0.008 c |
| Education | -152415941.745 | 54330629.112 | -0.435 | -2.805 | 0.007 c |
| Household income | 247459407.786 | 68144630.456 | 0.492 | 3.631 | 0.001 c |
| Social coverage | -45442118.334 | 50242320.167 | -0.098 | -0.904 | 0.369 |
| Housing situation | 96320307.893 | 76461047.877 | 0.140 | 1.260 | 0.212 |
a Dependent Variable: OOP.
b Correlation is significant at the 0.05 level (2-tailed).
c Correlation is significant at the 0.01 level (2-tailed).
5. Discussion
Breast cancer is a major health problem for Iranian women. Considering the costs of prevention, diagnosis, and treatment of BC, its management imposes a heavy burden on the economy of the household, which increases significantly with the advanced stages of the disease. The findings of our study showed that the contribution of OOP by patients to the total direct and indirect medical expenses was 32.89%. Therefore, many households are faced with impoverishment or catastrophic expenditure by paying these costs.
A significant portion OOP costs is associated with drug expenses. The study found that 47.18% of OOP costs are attributed to drug expenses, 16.19% to laboratory costs, 11.74% to imaging costs, 11.20% to visit costs, 8.40% to hospitalization costs, 2.84% to doctor's services costs, and 2.45% to physiotherapy costs. The results of Parnian et al.'s study showed that the average OOP payment including the cost of the drug with a rate of $37.99 ± 45.31 was the highest direct medical cost (19). A study conducted in India revealed that direct medical costs represented 56.3% of the total out-of-pocket expenses. Within the direct medical costs, systemic treatment accounted for 19.7%, radiotherapy for 12.97%, and surgical costs for 9.71%. Approximately 74.4% of patients availed government financial assistance, while 8% received full reimbursement (20). A study in Saudi Arabia showed that drug costs included 67% of the total medication costs. Of these costs, trastuzumab alone accounts for 94% (21). In Iran, as in other countries, drug costs constitute the largest share of cancer treatment costs. During the past years, due to international sanctions and the rise of the currency, the government has tried to cover a part of these costs, but the patients still pay a large part of the costs in the form of OOP.
BC affects the quality and quantity of life, as well as the economic well-being of affected patients and their families. The results of this study showed that with increasing income, patients had more OOP. Panahi et al.'s study showed that income has a positive and significant effect on OOP expenses (22). Pisu et al.'s study showed that the lower income of patients is effective in increasing OOP costs and OOP burden (23). It can be analyzed that patients with higher income are more referred to private hospitals, and tend to pay more OOP.
This study demonstrated that the out-of-pocket costs decreased as patients age. This could be attributed to younger or middle-aged patients having higher life expectancies and being more willing to pay for their treatment. Pisu et al.'s study showed that younger age is effective in increasing OOP costs and OOP burden (23). A study by Bygrave et al. in 2021 showed that patients with younger age (≤ 65 years) are at increased risk of having financial problems due to OOP costs (24). Compared to younger patients with BC, older patients were shown to incur lower costs (25). Another study showed that costs of care decreased with increasing age at most stages of BC diagnosis (26). These findings indicate that older patients receive less treatment.
The results of this study showed that people who were covered by support institutions had less OOP payments, but it had no significant effect on patients' OOP payments (P < 0.05). Pisu et al.'s study showed that the use of supportive services is effective in increasing OOP costs and OOP burden (23).
People who live in rural areas are more vulnerable to BC than people who live in urban areas, according to their income level. For this reason, they are mostly covered by a social support organization. The results of our study showed that people living in rural areas have lower OOP costs. Due to the fact that the willingness to pay is less in rural areas, another reason is that follow-up treatment and access to private hospitals and private doctors' offices are less in rural areas. Additionally, most people living in rural areas were covered by a social support organization. Other studies have shown that younger and lower-income rural patients were most burdened by breast cancer costs.
Prevention and early detection play an important role in reducing BC costs. A study showed that early detection and targeted treatment of cancer can save up to 11.35% of total cancer costs (27). Breast cancer is usually diagnosed in late stages in countries with limited resources. Early detection can shorten the stage of diagnosis, potentially improve the chances of survival and cure, and enable simpler and more cost-effective treatment.
Among the strengths of this study, it can be highlighted that data related to OOP was collected from three sources, which is in contrast to previous studies. The data of this study provide a detailed picture of OOP. In addition, our study contained comprehensive information on socio-economic characteristics, which allows us to introduce a wide range of factors influencing OOP.
The limitations of this study included the patient's recall error in stating the costs incurred during the past year. The authors attempted to validate the patient-reported costs by comparing the costs received from the patient records from the hospital and the costs paid by the IHIO. Another limitation was under-the-table or informal costs that patients were afraid to disclose. Before asking questions related to direct and indirect OOP costs, we tried to gain the trust of patients.
5.1. Conclusions
Despite comprehensive health care and support from social and depriving organizations in Iran, OOP can be significantly high for some patients. Breast cancer patients incur many expenses, and about 32.89% of these expenses are OOP payments. In order to support BC patients, insurance organizations need to increase their coverage. Additionally, there is a need for more government support in providing the necessary medicine and medical items.