1. Background
Lung cancer continues to be the leading cause of cancer-related mortality worldwide, with a staggering 1.8 million fatalities annually (1). Lobectomy is established as the gold standard treatment for early-stage non-small cell lung cancer (2). Despite the procedural advancements, lobectomy is fraught with significant risks, with studies indicating complication rates as high as 20 - 40% (3-9). These complications range from minor, such as prolonged air leak (occurring in up to 18% of cases) (6, 10, 11), to major cardiopulmonary complications occurred (7), which significantly impact patient morbidity and mortality (8).
The postoperative period following a lobectomy surgery is critical, with reported complication rates significantly affecting patient outcomes and healthcare costs (9). Studies have shown that the hospital readmission rate within 30 days post-lobectomy for lung cancer patients is approximately 12 - 15% (9, 10, 12). These readmissions are primarily due to complications related to the surgery (9, 13), emphasizing the importance of comprehensive postoperative care. Moreover, the unsettling variability in readmission rates reaching as high as 20% in certain institutions (14), highlights gaps in current practices and the need for standardized protocols to mitigate these risks and optimize patient outcomes.
The introduction of the enhanced recovery after surgery (ERAS) program emphasizes a multimodal approach that integrates various interventions from pre-operative patient counseling to post-discharge follow-up. This comprehensive approach has effectively mitigated surgical risks and significantly reduced adverse outcomes (15-17). Preliminary data suggest that implementing ERAS protocols can decrease complication rates by up to 50% and reduce readmission rates to below 10% (5, 16, 18).
To prepare for the implementation of the ERAS program, the aim of this research was to evaluate the postoperative complications and 30-day readmission rate along with related factors among patients with lung cancer undergoing lobectomy. By analyzing pre-intervention data, this study seeks to identify key factors that could be addressed through the ERAS program, ultimately aiming to enhance patient recovery, reduce complications and readmissions, and elevate the standard of care for lung cancer surgery patients. This study is part of a larger project, with previous publications from the same dataset focusing on different outcomes, specifically the length of postoperative hospital stay.
2. Methods
2.1. Study Design and Setting
This retrospective analysis was conducted at the University Medical Center Ho Chi Minh City, focusing on patients who underwent lobectomy for lung cancer from January 2018 to December 2021, prior to the ERAS program's implementation. This study is part of a comprehensive project evaluating various aspects of surgical outcomes for lung cancer patients. Previous publications from this project have examined different outcomes using the same dataset.
2.2. Participants
The study included patients diagnosed with lung cancer through pathological examination who underwent anatomical lung lobectomy. Patients who did not comply with follow-up examinations after discharge and those who were transferred to another hospital for postoperative care were excluded from the study.
2.3. Data Collection
Patient data were systematically extracted from electronic health records, including demographic information [age, gender, Body Mass Index (BMI)], preoperative clinical assessments [American Society of Anesthesiologists (ASA) classification, smoking history, comorbidity profile], surgical details (operative approach, operative time, intraoperative blood loss), and postoperative outcomes (complications classified using the Clavien-Dindo classification and 30-day readmission rates). This dataset overlaps with the one used in previous studies from the same project but focuses on different specific outcomes.
2.4. Outcome Measures
The primary objective of this study was to evaluate the incidence of postoperative complications as classified by the Clavien-Dindo classification system and the hospital readmission rates within 30 days post-discharge.
2.5. Statistical Analysis
Data were analyzed using STATA software, applying descriptive statistics to outline patient demographics and clinical features by frequency and rate. The chi-square test or Fisher's exact test was used to analyze the association between categorical variables. An independent t-test (or Mann-Whitney test) was used to explore the association between two quantitative variables, and multivariable logistic regression models were developed to identify independent predictors of postoperative complications and hospital readmissions. A P-value of < 0.05 was considered statistically significant.
3. Results
A retrospective study was conducted to investigate the factors associated with postoperative complications and readmission in 99 patients who underwent lobectomy for lung cancer at the University Medical Center Ho Chi Minh City. The dataset used for this study was also utilized in a previous publication that focused on different outcome measures.
3.1. Patient Demographics and Clinical Characteristics
The study included 99 patients, with 53 (53.5%) males and 46 (46.5%) females. The majority (83.3%) of patients were over 60 years old. The postoperative complication rate was 19.2% (19 patients), and the 30-day readmission rate was 13.1% (13 patients). The most common complications were Clavien-Dindo II (9.1%), followed by Clavien-Dindo I (4.1%), Clavien-Dindo IIIa (4.0%), and Clavien-Dindo IIIb (2.0%) (Table 1).
| Variables | Frequency (%) |
|---|---|
| Complication | 19 (19.2) |
| Clavien-Dindo I | 4 (4.1) |
| Clavien-Dindo II | 9 (9.1) |
| Clavien-Dindo IIIa | 4 (4.0) |
| Clavien-Dindo IIIb | 2 (2.0) |
| 30-day readmission | 13 (13.1) |
3.2. Complications and Readmissions
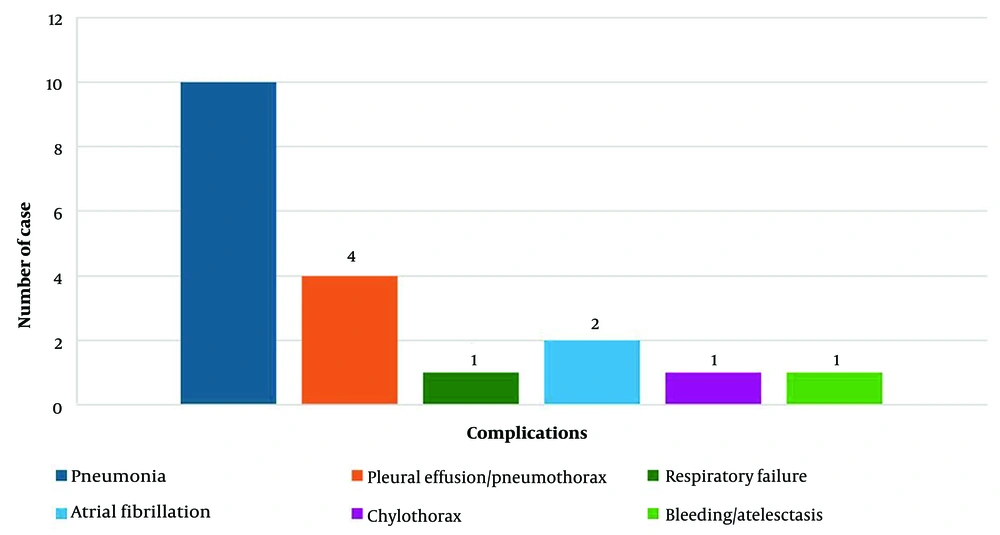
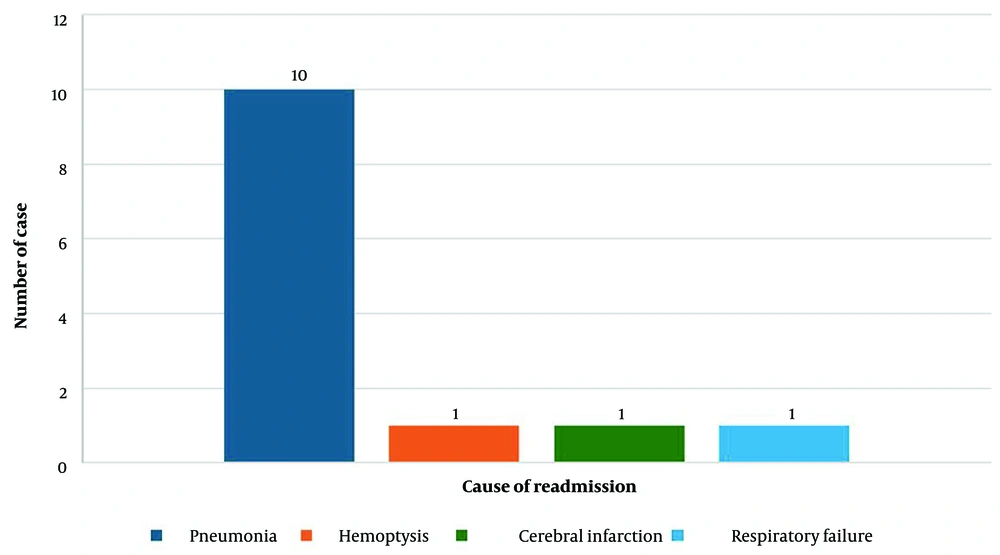
The specific postoperative complications are detailed in Figure 1, with pneumonia being the most common complication and the leading cause of hospital readmission. Figure 2 shows the causes of readmission.
3.3. Association with Patient Characteristics
Table 2 presents the association between complications, 30-day readmission rates, and patient characteristics. Most general patient characteristics were not significantly associated with postoperative complications and readmission. However, there was a significant association between complications and cell differentiation, with poorer cell differentiation associated with a higher risk of complications (P = 0.045). The readmission rate was also significantly higher in current smokers compared to former smokers and never-smokers (P = 0.04).
| Variables | Complications | P-Value b | Readmission | P-Value b | ||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||
| Gender | 0.154 | 0.231 | ||||
| Male | 13 (24.5) | 40 (75.5) | 9 (17) | 44 (83) | ||
| Female | 6 (13.0) | 40 (87.0) | 4 (8.7) | 42 (91.3) | ||
| Age group | 0.138 | 0.510 | ||||
| < 60 | 2 (8.3) | 22 (91.7) | 4 (16.7) | 20 (83.3) | ||
| ≥ 60 | 17 (22.7) | 58 (77.3) | 9 (12) | 66 (88) | ||
| BMI classification | 0.175 | 0.873 | ||||
| < 18.5 | 4 (50.0) | 4 (50.0) | 1 (12.5) | 7 (87.5) | ||
| 18.5 - 22.9 | 8 (16.0) | 42 (84.0) | 7 (14) | 43 (86) | ||
| ≥ 23 | 7 (17.1) | 34 (82.9) | 5 (12.2) | 36 (87.8) | ||
| ASA classification | 0.319 | 0.069 | ||||
| I | 2 (50.0) | 2 (50.0) | 0 (0) | 4 (100) | ||
| II | 11 (13.9) | 68 (86.1) | 8 (10.1) | 71 (89.9) | ||
| III | 6 (37.5) | 10 (62.5) | 5 (31.2) | 11 (68.8) | ||
| Cigerette smoking status | 0.454 | 0.040 | ||||
| Never cigerette smokers | 8 (12.9) | 54 (87.1) | 4 (6.5) | 58 (93.5) | ||
| Former cigerette smokers | 0 (0) | 10 (100) | 7 (25.9) | 20 (74.1) | ||
| Current cigerette smokers | 11 (40.7) | 16 (59.3) | 2 (20.0) | 8 (80.0) | ||
| Tumor location | 0.622 | 0.344 | ||||
| Left-upper lobe | 4 (14.8) | 23 (85.2) | 1 (3.7) | 26 (96.3) | ||
| Left-lower lobe | 2 (16.7) | 10 (83.3) | 1 (8.3) | 11 (91.7) | ||
| Right-upper lobe | 6 (20.0) | 24 (80.0) | 5 (16.7) | 25 (83.3) | ||
| Right-lower lobe | 6 (33.3) | 12 (66.7) | 4 (22.2) | 14 (77.8) | ||
| Right-center lobe | 1 (8.3) | 11 (91.7) | 2 (16.7) | 10 (83.3) | ||
| TNM stage | 0.349 c | 0.059 | ||||
| IA | 0 (0) | 1 (100) | 0 (0) | 12 (100) | ||
| IB | 4 (14.8) | 23 (85.2) | 2 (7.4) | 25 (92.6) | ||
| IIA | 6 (24.0) | 19 (76.0) | 4 (16) | 21 (84) | ||
| IIB | 7 (28.0) | 18 (72.0) | 3 (12) | 22 (88) | ||
| IIIA | 2 (22.2) | 7 (77.8) | 3 (33.3) | 6 (66.7) | ||
| IIIB | 0 (0) | 1 (100) | 1 (100) | 0 (0) | ||
| Lung cancer cell types | 0.803 c | 0.113 | ||||
| Adenocarcinoma | 16 (20.5) | 62 (79.5) | 9 (11.5) | 69 (88.5) | ||
| Squamous cell carcinoma | 3 (15) | 17 (85) | 3 (15) | 17 (85) | ||
| Large cell carcinoma | 0 (0) | 1 (100) | 1 (100) | 0 (0) | ||
| Cell differentiation | 0.045 c | 0.429 | ||||
| Well differentiated | 0 (0) | 4 (100) | 1 (25) | 3 (75) | ||
| Moderately differentiated | 15 (17.1) | 73 (82.9) | 12 (13.6) | 76 (86.4) | ||
| Poorly differentiated | 4 (57.1) | 3 (42.9) | 0 (0) | 7 (100) | ||
Abbreviations: BMI, Body Mass Index; ASA American Society of Anesthesiologists.
a Values are expressed as No. (%).
b Logistic regression.
c Fisher’s exact test.
3.4. Association with Treatment Characteristics
Table 3 describes the relationship between complications, 30-day readmission rates, and treatment characteristics. There was a statistically significant difference in complication rates between the open surgery group (42.9%), thoracoscopic surgery converted to open (20%), and thoracoscopic surgery (11.8%) (P = 0.026). Increased complication rates were observed in patients who did not receive muscle relaxation and early extubation (P = 0.01). The complication rate was significantly reduced in patients who received multimodal analgesia (P = 0.001) and physical therapy before surgery (P = 0.021). Conversely, preoperative opioid use increased the complication rate (P = 0.042). Early postoperative physiotherapy reduced both complication (P = 0.007) and readmission rates (P = 0.031).
| Variables | Complications | P-Value b | Readmission | P-Value b | ||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | |||
| Operation method | 0.026 | 0.068 c | ||||
| Open surgery | 9 (42.9) | 12 (57.1) | 6 (28.6) | 15 (71.4) | ||
| Thoracoscopic surgery | 8 (11.8) | 60 (88.2) | 6 (8.8) | 62 (91.2) | ||
| Thoracoscopic surgery convert to open | 2 (20) | 8 (80) | 1 (10) | 9 (90) | ||
| Muscle relaxation and early extubation | 0.010 c | 0.064 c | ||||
| Yes | 0 (0) | 21 (100) | 0 (0) | 21 (100) | ||
| No | 19 (24.4) | 59 (75.6) | 13 (16.7) | 65 (83.3) | ||
| Multimodal pain relief | 0.001 | 0.191 | ||||
| Yes | 3 (5.5) | 52 (94.5) | 5 (9.1) | 50 (90.9) | ||
| No | 16 (36.4) | 28 (63.6) | 8 (18.2) | 36 (81.8) | ||
| Physical therapy before surgery | 0.021 | 0.008 c | ||||
| Yes | 1 (3.1) | 31 (96.9) | 0 (0) | 32 (100) | ||
| No | 18 (26.9) | 49 (73.1) | 13 (19.4) | 54 (80.6) | ||
| Using opioid before surgery | 0.042 c | 0.068 c | ||||
| Yes | 4 (50) | 4 (50) | 3 (37.5) | 5 (62.5) | ||
| No | 15 (16.5) | 76 (83.5) | 10 (11) | 81 (89) | ||
| Physical therapy at recovery unit | 0.007 | 0.031 | ||||
| Yes | 1 (2.5) | 39 (97.5) | 1 (2.5) | 39 (97.5) | ||
| No | 18 (30.5) | 41 (69.5) | 12 (20.3) | 47 (79.7) | ||
| Physical therapy after surgery | 0.237 c | 0.001 c | ||||
| Yes | 15 (17.2) | 72 (82.8) | 7 (8.1) | 80 (91.9) | ||
| No | 4 (33.3) | 8 (66.7) | 6 (50) | 6 (50) | ||
| Vomiting after surgery | 0.008 c | 0.208 c | ||||
| Yes | 7 (46.7) | 8 (53.3) | 0 (0) | 15 (100) | ||
| No | 12 (14.3) | 72 (85.7) | 13 (15.5) | 71 (84.5) | ||
| Variables | OR (CI 95%) | P-Value | OR (CI 95%) | P-Value | ||
| Amount of blood loss (mL) | 1.007 (1.002 - 1.012) | 0.004 | 1.005 (0.996 - 1.010) | 0.068 | ||
| Operation time (min) | 1.00 (0.99 - 1.01) | 0.723 | 0.997 (0.985 - 1.008) | 0.587 | ||
| Duration of endotracheal retention (h) | 1.266 (1.069 - 1.5) | 0.006 | 1.101 (0.975 - 1.244) | 0.121 | ||
| Duration of post-anesthesia care unit (h) | 1.056 (1.016 - 1.097) | 0.005 | 1.019 (0.983 - 1.057) | 0.302 | ||
| Duration of thoracic drainage (days) | 2.111 (1.423 - 3.132) | < 0.001 | 1.146 (0.912 - 1.440) | 0.244 | ||
| Preoperative fasting time (h) | 1.113 (0.934 - 1.326) | 0.230 | 1.060 (0.868 - 1.295) | 0.568 | ||
| Postoperative fasting time (h) | 1.217 (1.068 - 1.387) | 0.003 | 1.001 (0.873 - 1.149) | 0.986 | ||
| Urinary catheter retention time (h) | 1.000 (0.955 - 1.047) | 0.974 | 0.982 (0.923 - 1.044) | 0.559 | ||
a Values are expressed as No. (%).
b Logistic regression.
c Fisher’s exact test.
Losing 1 mL of blood increased the complication rate by 0.7% (P = 0.004). Each additional hour of endotracheal retention increased the complication rate by 26.6% (P = 0.006), and each additional hour in the Post-Anesthesia Care Unit (PACU) was associated with a 5.6% rise in complication rate (P = 0.005). Prolonged thoracic drainage per day increased the complication rate by 2.11-fold (P < 0.001). Furthermore, longer post-operative fasting time per hour increased the complication rate by 21.7% (P = 0.003).
5. Discussion
Lobectomy is a preferred treatment option for lung cancer (19, 20). However, the invasive nature of surgery inevitably carries inherent risks, particularly complications leading to readmission (12, 21). Our study conducted at the UMC on 99 patients provides insightful pre-ERAS program data on complications and hospital readmission rates post-lobectomy for lung cancer treatment.
The general results emphasize a significant association between patient characteristics and treatment factors with postoperative outcomes. According to the study of Brunelli et al. (22), which emphasized the role of patient-specific factors in postoperative complications, our result highlights the influence of factors such as age, BMI, and ASA classification on postoperative recovery and complications. This survey helps identify current issues in the treatment and care process, thereby planning to develop appropriate ERAS programs.
Postoperative complication rates serve as a crucial index in our center, employed to evaluate treatment efficacy and patient care quality. Within this study, we observed a postoperative complication rate of 19.2% (19 patients). This aligns with Al-Githmi et al.'s findings in video-assisted thoracoscopic surgery (VATS) patients, where the complication rate was 19.4% (4). A systematic review by Fiore reported complication rates ranging from 14% to 46% (9). These findings suggest that while our complication rates are within the reported range, there is significant room for improvement, particularly through the implementation of enhanced postoperative care protocols and treatment optimization strategies.
There was a statistically significant association between complication rates and the type of surgery performed. Patients undergoing traditional open surgery had a higher complication rate (42.9%) compared to those undergoing VATS (11.8%, P = 0.026). Systematic reviews and meta-analyses, such as Li et al. (17), have also reported higher complication rates for open surgery, with Rogers's (8) study demonstrating a complication rate of up to 37.6%. This highlights the potential benefits of minimally invasive techniques in reducing postoperative complications. Furthermore, the effectiveness of multimodal analgesia, preoperative physiotherapy, and rehabilitation physiotherapy in reducing postoperative complications by 30.9% (P = 0.001), 23.8% (P = 0.021), and 28% (P = 0.007), respectively, aligns with the principles of the ERAS program (23, 24). Effective pain control is crucial not only for improving patient comfort but also for minimizing the physiological stress response to surgery, which can exacerbate or lead to complications. Thus, ERAS emphasizes a multimodal approach to optimize postoperative recovery to minimize the risk of complications.
Pneumonia was the most common postoperative complication and the leading cause of hospital readmission in our study. This finding emphasizes the importance of perioperative physiotherapy and rehabilitation in reducing the incidence of pneumonia and subsequent readmissions. These findings highlight the efficacy of improving patients' physical status before, during, and after surgery. Rodriguez-Larrad et al. (25) in a comprehensive review and meta-analysis, noted multiple studies reporting the benefits of perioperative physical therapy for lung cancer resection patients, demonstrating its effectiveness in reducing the occurrence of complications that often lead to readmissions.
Our study found a 30-day readmission rate of 13.1%, which is lower than previous reports. In Seely's study, the rate was 17%, with prolonged air leaks being a major complication leading to readmission (10). The readmission rate within 30 days provides an important metric for evaluating the effectiveness of both primary and post-surgical care. Notably, a significant reduction in readmission rates was associated with physical therapy before surgery (19%, P = 0.008), physical therapy early at the recovery unit (17.8%, P = 0.031), and physical therapy after surgery (41.9%, P = 0.001). These findings highlight the efficacy of improving a patient's physical status before, during, and after surgery. Rodriguez-Larrad et al. (25), in a comprehensive review and meta-analysis, noted multiple studies reporting the benefits of peri-operative physical therapy for lung cancer resection patients, demonstrating its effectiveness in reducing the occurrence of complications that often lead to readmissions. Pre-, intra-, and postoperative physiotherapy efforts support the widespread adoption of ERAS protocols. By systematically implementing practices such as minimally invasive surgical techniques, advanced pain management protocols, and preoperative physical therapy, healthcare institutions can achieve better patient outcomes. These improvements not only reduce the rates of complications and readmissions but also lower overall healthcare costs and enhance patient satisfaction (23).
However, this study's limitations, including its retrospective design and the potential for selection bias, necessitate a cautious interpretation of the findings. Despite these constraints, the study offers valuable pre-ERAS implementation insights, laying a foundation for subsequent ERAS program development. By identifying key factors contributing to complications and readmissions, our research paves the way for targeted interventions within the ERAS framework, aimed at improving surgical outcomes and patient experiences in lung cancer treatment.
5.1. Conclusions
In conclusion, our study not only contributes to the growing body of evidence supporting the ERAS program's effectiveness but also highlights critical areas for its application and development in lung cancer surgery. Future research, leveraging prospective designs and broader datasets, will be crucial in validating these findings and further refining ERAS protocols for lung cancer patients undergoing lobectomy.