1. Background
Cancer remains a major cause of death in children, even with medical progress and higher survival rates, as affected children still face a range of symptoms in various aspects due to the disease and its treatment repercussions (1). This not only diminishes the child's quality of life but also significantly impacts the entire family, who are often the primary caregivers (2). While childhood cancer is rarer than adult cancer, its influence on families and the healthcare system is profound (3).
Pediatric Palliative Care (PPC) seeks to enhance the quality of life for young patients and their families who are confronting life-threatening conditions by preventing and alleviating suffering through the identification and management of pain and other physical, psychosocial, or spiritual symptoms (4, 5). Pediatric Palliative Care also caters to the diverse developmental stages of children—from infancy to adolescence—acknowledging their growth. The complexity of children's understanding of illness and the essential role of parental involvement in care planning and decision-making heighten the PC professionals' task of delivering family-centered care (6).
In 2017, it was estimated that around 4 million children require palliative care (PC) globally, with over 97% residing in Low and Middle-Income Countries (LMICs) (7). However, only a small fraction of these children can access such services. Children with cancer who receive PC experience numerous benefits, including improved physical and mental symptoms, more frequent and earlier discussions about end-of-life care, and enhanced quality of life (8, 9).
Despite these benefits, delivering palliative care presents several challenges, with one of the most significant being the absence of standard guidelines and service packages (10, 11).
Quality care can be enhanced by offering cost-effective service packages tailored to the economic, social, cultural, and political landscape of the community. These prioritized sets of services aim to reform health systems thoughtfully, ensuring equitable access to health services and reducing overall costs (12). A basic PC package should be integrated into the healthcare system to support Universal Health Coverage (UHC) and reduce hospital stays and associated expenses. The Lancet Commission underscores the value of such packages in providing essential services affordably, especially in resource-limited settings, thereby addressing significant health disparities (13).
The draft national action plan for palliative care in Iran acknowledges the importance of enhancing palliative care services and referral systems (14). However, children with illnesses and their families continue to have limited access to resources, resulting in a low quality of life.
Thus, there is an urgent need to develop a PC package for children with cancer in Iran that aligns with the country's conditions, ensuring family satisfaction, which is a key indicator of service quality (2).
This study was conducted to develop an essential PC service package for children with cancer in Iran, guided by the WHO's PPC guideline.
1.1. Conceptual Framework
The package comprises a selection of safe, effective, low-cost drugs, basic equipment, and essential social support to alleviate various forms of distress. It also outlines the necessary human resources for the provision of effective and safe services, and ensuring support for patients and their families throughout the illness. The package is structured around two main INPUT and INTERVENTIONs components. INPUT includes four key dimensions such as essential medicine, human resources, equipment, and social support which form the foundation for the INTERVENTION component.
2. Objectives
The INTERVENTION aspect focuses on four dimensions aimed at preventing and mitigating physical, psychological, social, and spiritual symptoms (15).
3. Methods
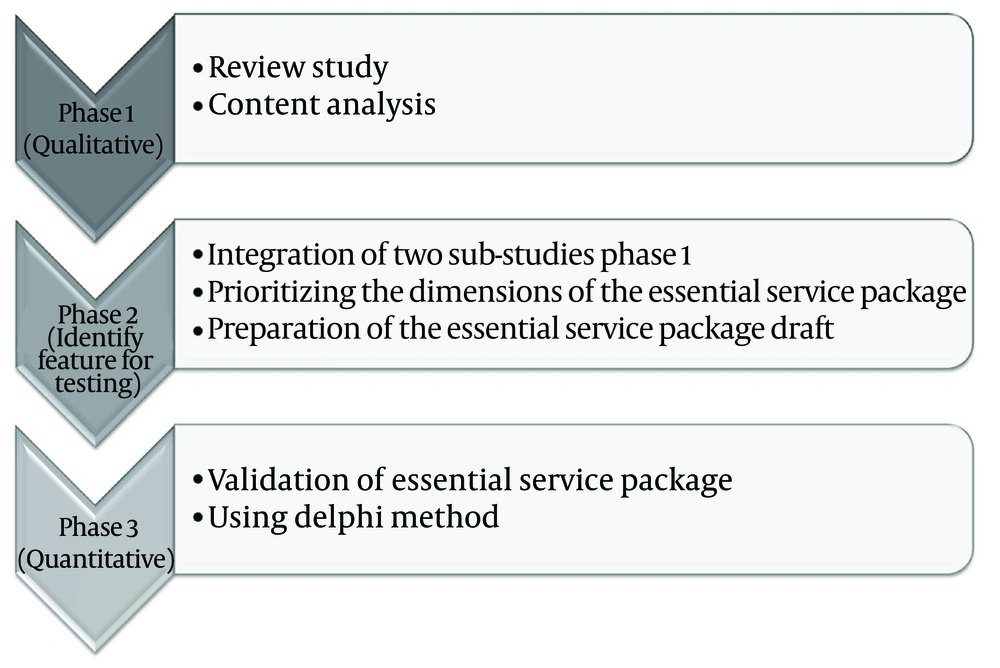
The current study utilized a Health System Research approach, employing an exploratory mixed-method design across three stages (Figure 1).
3.1. First Phase
The initial phase aimed to identify the fundamental PC needs of children with cancer. This was achieved through a review study and qualitative content analysis.
In the review section, searches were conducted using MeSH keywords such as terminal care, hospice, end of life, supportive, medicine, palliative, care, service package, therapy, child, children, pediatrics, oncology, and guidelines. These searches were performed both individually and in combination with special characters across various databases and search engines—national (SID, Magiran, Iran Medex) and international (Scopus, PubMed, Web of Sciences, ProQuest, CINAHL, Medline Plus, EMBASE, Cochrane Library, Google Scholar). Additionally, significant specialized journals in pediatric cancer care, scientific and administrative documents, reports from the WHO, clinical guidelines and protocols, government websites, and other authoritative sources were reviewed from 2014 to 2023.
The search encompassed article titles, abstracts, full texts, and other relevant texts. To ensure search comprehensiveness, reference lists of related studies were examined for additional sources. Documents in English and Farsi focusing on PPC services were imported into EndNote software. The initial software screening excluded studies with duplicate titles. Subsequently, the research team reviewed titles and abstracts to eliminate irrelevant studies.
Two researchers independently scrutinized the original texts of all documents and articles included in the study. Data extraction was targeted to include only information pertinent to the WHO framework (15). The extracted key findings were reviewed by the research team and categorized within the framework.
To incorporate stakeholder perspectives, the results of the previously conducted content analysis were used. A detailed explanation of this process is available in previously published articles (2, 16, 17).
3.2. Second Phase
During this phase, the findings from the first phase were synthesized to identify key components for “prioritizing the essential needs of PC for children with cancer.” These components were formulated into a 113-item questionnaire across 10 dimensions for expert evaluation using the Delphi technique.
Delphi members were selected through purposive and snowball sampling among health system policymakers, faculty members, nurses, physicians, and other health care professionals experienced in PPC.
Notably, some experts were also affiliated with non-governmental organizations, charities, and health insurance bodies. In line with similar studies (18) and considering the subject’s breadth and available resources, 12 experts agreed to participate. They received the questionnaire either in person or via email. Experts were asked to rank each item based on importance from 4 to 1. An open-ended question at the end of the questionnaire allowed them to provide additional insights. Since the Delphi questionnaire was developed by the research team and based on the findings, Delphi was conducted in one round and lasted one month.
The Delphi method was decision-making oriented with a quantitative approach. Fowle recommended ten steps (19, 20) were employed for implementation. Given the variety of symptoms and the necessity to prioritize them, a focus group was established to address the prioritization of physical symptoms. This group included four pediatric oncology doctors, three pediatric oncology nursing professors, and two nurses from the oncology department.
Data analysis involved SPSS software for descriptive statistics to determine each item’s mean and standard deviation. Following a similar research approach (21), items averaging 3 or above were selected. The research team analyzed and consolidated these opinions to develop an essential PPC service package.
3.3. Third Phase
The final phase aimed to assess the importance, scientific acceptability, and operational feasibility (validation) of the proposed package. This was achieved by soliciting feedback from professors and experts via the Delphi technique. Since this phase is similar to the second round of the Delphi process and involves the same participants, previous details about panelist characteristics are omitted here.
A refined questionnaire with 54 items—excluding those averaging below 3 from the prior phase—spanning 9 dimensions was distributed to experts. To evaluate each item, they were requested to rate each criterion for every index on a scale ranging from low (1) to high (3).
After receiving feedback and implementing suggestions, the service package was finalized. Descriptive statistics and SPSS software facilitated the analysis of questionnaire responses.
4. Results
In the initial review phase, 165 papers were identified. After excluding duplicates, studies focusing on specific interventions, redundant studies, those with inaccessible full texts, or insufficient information for inclusion in the study’s analytical framework, 73 papers remained. This collection included 32 journal articles, 8 conference abstracts, 7 book chapters, 7 doctoral dissertations, 10 government documents, and 9 guidelines that passed the title and abstract screening criteria.
Subsequent full-text evaluations resulted in the exclusion of 48 papers. Ultimately, data from 25 papers were utilized. The information from these selected articles, combined with data from qualitative interviews, were analyzed using directed content analysis. This process yielded 113 items aligned with WHO guidelines. These items were categorized into two primary components according to the conceptual model: ‘INPUT’ with five subcategories and ‘INTERVENTION’ with five subcategories.
In the second step, the draft of the service package was developed and distributed to experts in the form of a Delphi. After data analysis, the average scores ranged from 3.8 ± 0.4 to 2.1 ± 0.59. Items scoring an average of 3 or less were eliminated, and the remaining items were prioritized according to their scores for inclusion in the PPC package. As per expert recommendations, the dimension of social support has been removed, and its components have been integrated into the dimension of social interventions due to overlap. The final draft of the care package included 9 dimensions with 54 items (Table 1).
| Dimensions and Requirements | Mean ± SD |
|---|---|
| Access to services | |
| General and specialized services | 3.21 ± 0.9 |
| Specific service delivery path | 3.23 ± 1 |
| Universal coverage | 3.53 ± 0.3 |
| Clear job descriptions | 3.85 ± 0.7 |
| Providing care at community levels (community health centers, clinics, home) | 3.80 ± 0.3 |
| Equipment | |
| Pressure-reducing mattresses | 3.57 ± 0.6 |
| Gastrointestinal feeding tubes | 3.23 ± 0.8 |
| Urinary catheters | 3.71 ± 0.6 |
| Opioid locked boxes | 3.76 ± 0.4 |
| Flashlights with rechargeable batteries | 3.76 ± 0.4 |
| wheelchair | 3.71 ± 0.6 |
| oxygen | 3.92 ± 1 |
| Portable pulse oximeter | 3.64 ± 0.6 |
| Toys and teaching aids | 3.15 ± 0.8 |
| Human resources | |
| Pediatrician | 3.35 ± 0.8 |
| Trained general practitioner | 3.64 ± 0.6 |
| General nurse/trained specialist | 3.57 ± 0.7 |
| Trained clinical psychologist/psychiatrist | 3.50 ± 1 |
| Trained volunteers | 3.15 ± 1 |
| Caregivers | 3.41 ± 0.7 |
| Medications and narcotic compounds required | |
| Access to essential medications for children's palliative care based on WHO | 3.41 ± 0.7 |
| Social support | |
| Economic support of the patient and family | 3.23 ± 0.7 |
| Management of pain and physical symptoms | |
| Pain assessment | 3.57 ± 0.6 |
| Clinical guidelines for pain management | 3.64 ± 0.6 |
| Access to oral and injectable drugs | 3.71 ± 0.6 |
| Access to non-opioid painkillers | 3.78 ± 0.5 |
| Medicinal and non-medicinal methods of pain control/relief | 3.64 ± 0.5 |
| Assessment of physical symptoms with general tools | 3.64 ± 0.7 |
| Evaluation of physical symptoms with specific tools | 3.50 ± 1 |
| Management of physical symptoms | 3.64 ± 1 |
| Access to oral and injectable forms of required drugs | 3.64 ± 0.6 |
| Access to equipment | 3.41 ± 0.7 |
| Education and empowerment of the child and family in care | 3.21 ± 0.9 |
| Management of psychological symptoms | |
| Assessment of psychological symptoms | 3.84 ± 0.3 |
| Communicating with the child and family | 3.78 ± 0.4 |
| Identifying psychological needs | 3.69 ± 0.4 |
| Preserving the dignity of the cook and family | 3.28 ± 0.7 |
| Using coping strategies | 3.57 ± 0.6 |
| Access to a psychiatrist | 3.85 ± 0.3 |
| Access to a psychologist for counseling | 3.28 ± 0.7 |
| Access to medication | 3.85 ± 0.3 |
| Social symptom management | |
| Educational and educational services (facilitating the child's attendance at school) | 3.41 ± 1 |
| Counseling and identification of parental social disorders, including role conflict | 3.64 ± 0.6 |
| Access to social support networks for children and families | 3.41 ± 0.7 |
| Donor support | 3.21 ± 1 |
| Management of spiritual symptoms | |
| Assessment of spiritual distress | 3.85 ± 0.3 |
| Using spiritual coping strategies | 3.5 ± 0.7 |
| Respecting the religious rituals of the family | 3.20 ± 0.8 |
| Attention to the cultural and religious background of the family | 3.53 ± 0.8 |
| Access to spiritual consultant | 3.50 ± 0.9 |
| Access to the clergyman | 3.85 ± 0.3 |
| Growth and development | |
| Social activities | 3.57 ± 0.6 |
| Assessment of developmental stages | 3.71 ± 0.6 |
| Play | 3.64 ± 0.5 |
Following a focus group session on physical symptoms, key symptoms such as pain, nausea and vomiting, diarrhea and constipation, mucositis, fatigue, anorexia and cachexia, fever and neutropenia, shortness of breath, bleeding, and seizures were identified as priorities.
In the third phase, experts evaluated the 9 dimensions and 54 items to determine the significance, scientific validity, and operational feasibility of the designed package. After data analysis, components with an average score of 2 or less were removed. Ultimately, the essential PPC package was finalized with two main components: INPUT—encompassing medicine, human resources, equipment, and service delivery setting; and INTERVENTION—covering management of physical symptoms, psychological support, social care, spiritual care, and growth and development needs with 44 items (Table 2).
| INTERVENTION | INPUT | |||
|---|---|---|---|---|
| Medicine | Equipment | Human Resource | Service Delivery | |
| Management of physical symptoms | Oral amitriptyline, oral bisacodyl, oral and injectable dexamethasone, oral and injectable diazepam, oral and injectable diphenhydramine, oral and injectable dimenhydrinate, oral fluconazole, oral fluoxetine, oral sertraline or citalopram for ages over 8 years, oral and injectable furosemide, oral and injectable haloperidol, oral and injectable hyoscine butyl bromide, ibuprofen (naproxen, diclofenac or meloxicam for ages over 3 months), oral lactulose (sorbitol or polyethylene glycol), oral loperamide, oral and injectable metoclopramide for ages over 1 month, oral metronidazole, oral morphine (for ages over one month), immediate-acting injectable naloxone, oral omeprazole, oral and injectable ondansetron, oxygen, oral paracetamol, petroleum jelly | Pressure-reducing mattresses, gastrointestinal feeding tubes, urinary catheters, opioid lock boxes, flashlights with rechargeable batteries, diapers or cotton and plastic, wheelchairs and cane, oxygen portable pulse oximeter | Pediatrician, General Practitioner Nurse | Urban Community Health Centre, general clinics, home care services |
| Management of psychological symptoms | Oral amitriptyline, oral and injectable dexamethasone, oral and injectable diazepam, oral and injectable diphenhydramine, oral fluoxetine, oral sertraline or citalopram, oral and injectable haloperidol | Trained psychologist; Trained volunteers | Urban Community Health Centre, general clinics, home care services | |
| Social symptom management | Teaching aids, toys | Social worker, school nurse, volunteers | Charities | |
| Management of spiritual symptoms | Trained Spiritual Counselor; Trained nurse or psychologist | |||
| Growth and development | Playroom, toys, teaching aids | Urban Community Health Centre, general clinics, home care services | ||
5. Discussion
The PPC package aims to provide essential PC services for the child with cancer. According to the WHO, community-based PC services are crucial in lLMICs. In this study, a PPC package based on the WHO guideline was developed which is focusing on two components with 9 dimensions.
Regarding INPUT while the WHO guideline includes only four dimensions for INPUT (15), in this study, expanded to address the unique context in Iran. Since PC services are not yet integrated at the primary levels of the health system (2), we added a separate dimension for service delivery settings based on stakeholder input. This includes settings from hospitals to community (home) care (13).
Additionally, the dimension of "social support" with the aim of economic support was removed due to significant overlap with the dimension of social interventions. Within this package, one of the services in the dimension of social symptom management includes economic support provided by social workers and charities, which aligns with WHO recommendations.
The WHO emphasizes four dimensions of intervention needs. However, this study also considered growth and development as a dimension of care. Meeting growth and development needs aligns with global standards and is essential for children with cancer. In fact, the 2022 standards of care for these children recognize this dimension (22).
Interventions to manage symptoms and address the needs of children and their families are fundamental in PC. Developing a standard care plan involves a comprehensive history-taking and detailed clinical examination of the child. Clinical tools play a crucial role in this process, either by broadly assessing multiple needs or by providing specific tools for individual signs (23).
In this PPC essential package, the PaPaS Scale (Pediatric Palliative Screening Scale) is introduced as a general tool that evaluates the impact of the disease on the child and their family which considers five dimensions including course of the disease, impact on daily activities, expected treatment outcomes related to the disease, symptom burden, and preferences of the patient, parent, or healthcare professional (24).
The specific tools for each symptom are listed in Table 3.
| Symptoms and Tools |
| Pain |
| PIPP (Premature Infant Pain Profile) for preterm and full-term babies |
| FLACC (Face, Legs, Activity, Cry, CONSOL ability) for children aged 2 months to 7 years |
| Pain Word Scale for children aged 3 - 7 years |
| FACES for children aged 5 - 12 years |
| NCCPC (Non-Communicating Children’s Pain Checklist) for non-verbal children aged 18 months and older |
| Nausea |
| 10-cm self-report Visual Analog Scale Nause |
| Pediatric Nausea Assessment Tool |
| Constipation |
| Constipation Assessment Scale |
| Mucositis |
| Children’s International Mucositis Evaluation Scale |
| Oral Mucositis Daily |
| Fatigue |
| Fatigue Scale-Adolescents |
| Fatigue Scale-Children |
| Anxiety and Depression |
| 10-cm Self-Report Visual Analog Scale Anxiety |
| Children’s Depression Inventory |
| Revised Children’s Manifest Anxiety Scale |
| Children’s Depression Inventory |
| Spirituality |
| Functional Assessment of Chronic Illness Therapy Spiritual Well-Being |
| Spirituality Sensitivity Scale for Children |
| Attitudes Toward God Scale |
5.1. Physical Symptoms Management
The most common reason for children to seek PC centers is physical symptoms, with pain being a significant concern, especially during the end stages of life. For children, pain is an unpleasant experience, while parents and professional staff find it distressing (3).
Effective pain management in PPC involves several key components which availability of specific pain assessment tools is one of them (Table 3).
The other component is applying painkillers. The most common method is the WHO's pain ladder. Based on this, the use of basic analgesia including acetaminophen and combination with non-steroidal anti-inflammatory drugs (NSAID) such as ibuprofen is recommended. In the later stages, opioids or Adjuvant Analgesia are recommended (25). In this package, the prescription of drugs for pain relief is based on the laws of the country, so it poses a challenge to the use of drugs. Additionally, the lack of access to oral morphine has also aggravated this challenge (26).
Drug prescription in different countries follows specific procedures. For example, in well-developed countries, a nurse can prescribe the pain killers, but in countries like Iran, prescription is the sole responsibility of a doctor (17). Therefore, despite WHO's recommendation for emergency medicines for PPC, its enforceability is different in countries (15).
According to the participants, gastrointestinal symptoms, fever, neutropenia, fatigue, and respiratory symptoms are other symptoms that lead to visiting a doctor or being hospitalized. However, since the side effects of chemotherapy appear with different severity based on the type of cancer and treatment protocols (23), it is possible that there are differences in the prevalence of symptoms. For example, the World Atlas of PC has reported fatigue as the second most common symptom in children at the end of life after pain (27) which is not in line with our findings.
5.2. Psychological Symptoms Management
Dealing with cancer is seen as a source of stress for both the child and the family. Hence, employing supportive methods to aid in the adaptation of children and families is crucial when providing PC (7). Research conducted in Iran highlighted the importance of assistance for mothers of children with cancer which is overlooked (11, 16). Therefore, it is advisable to develop compassionate and successful communication with the child and family within this package to recognize their emotional needs. Establishing communication built on trust and adjusted to the child's developmental stage is a key factor in enabling the delivery of PC (28). The medical staff's communication and support for the child and family evoke feelings of peace and inner strength, diminishing fears and anxiety while enhancing symptoms and overall well-being (16, 29). According to this package, nurses assess the psychological needs of the child and family through communication and using specific tools, referring them to a psychologist when needed. Psychologists should prioritize addressing the needs of family members, such as parents and siblings, in addition to those of a child with cancer. It is crucial to teach children and family members coping strategies, resilience, emotional management, and other necessary strategies (9).
5.3. Social Symptoms Management
Children with cancer are usually unable to participate in normal daily and social activities like going to school and playing with friends because they require intensive care and treatment, leading to feelings of loneliness, fear, anger, and discomfort (30). Additionally, the parents are dedicated to caring for the child with cancer, leading them to feel inadequate in fulfilling their other responsibilities like parental roles to other children (29).
Several studies have demonstrated that caregivers who have a higher level of social support tend to employ more effective coping strategies (31, 32). As per the advice of the Lancet commission, it is crucial to include social workers and social support programs in these care packages (13). Often, patients and their families are overlooked and require financial and non-financial assistance in children's PC (15). Fortunately, the Ministry of Health in Iran has developed and published a guideline for the use of social workers’ services in primary healthcare and PC.
Additionally, utilizing volunteers as family mediators and service providers for PC is widespread globally and remains cost-effective in low-resource countries (33). In Iran, volunteers offer psychological, economic, and social assistance to different organizations. However, they do not receive formal training (11).
5.4. Spiritual Symptoms Management
Dealing with cancer potentially leads to spiritual distress. Spiritual distress results in diminished energy, hostility, hopelessness, isolation, and powerlessness (34). Conversely, this distress has the potential to result in positive outcomes like strengthening faith and finding spiritual direction, developing resilience, and fostering a sense of optimism which tracks the child and family's development in spirituality (35). Experts should be involved in addressing common spiritual and existential issues for children and their families to manage spiritual distress. Continuously exploring spiritual concerns, identifying backgrounds, providing support from spiritual communities, and being sensitive to religious symbols are all important (36). When caring for children with cancer, it is important to consider the standards of care and address the spiritual needs (22).
These needs are typically assessed by healthcare professionals specialized in spirituality such as nurses or psychologists. If possible, it can be beneficial to consult with clergy or individuals knowledgeable in matters of spirituality (24).
5.5. Management of Growth and Development Needs
The constraints linked to the disease and the changes that occur affect the ability and opportunities of children and adolescents in their developmental and transitional phases (22). The requirements for development, such as play, social abilities, physical skills, and daily tasks, differ for different age ranges, resulting in the creation of targeted interventions for each group (25). This package offers interventions to track development in young children, along with games and social activities led by volunteers and social workers, in line with the standard of care for children with cancer.
5.6. Equipment
One of the dimensions of this care package is providing equipment to reduce the child's pain and suffering while improving the quality of services. This equipment should be simple to use, affordable, and readily available. It serves to meet the child's essential needs and can be provided either by the family or the service center (15).
5.7. Human Resources
Human resources are another dimension of this care package, and the most critical factor in providing human resources is the type of service delivery setting. Human resources can vary from general doctors, nurses, or experienced midwives to specialized team members. Additionally, the composition of the team depends on the specific setting, ranging from community-level care to specialized hospitals (13, 15).
The minimum required human resources include pediatricians, general practitioners, nurses, psychologists, social workers, volunteers, and, if feasible, spiritual therapists. According to WHO, the key team members providing PC services are doctors, nurses, psychologists, and social workers.
5.8. Settings of Service Provision in Palliative Care
One crucial dimension added to this package is the settings for service provision. In Iran, PC remains a relatively new concept and is currently available only in tertiary-level or specialized health system settings (11). However, stakeholders recognize the importance of expanding these services to PHC (37).
Within this package, the focus is on ensuring easy access to services and meeting the needs of children and families at the community level. As a result, comprehensive urban health centers, general clinics, and home-based care are introduced as the most critical settings. The WHO emphasizes providing PC services at the community level, especially in low-income countries with limited resources (15).
5.9. Conclusions
Using an integrated approach in the current study, a service package was developed that combines WHO recommendations, a literature review, and local insights. This helped identify different aspects related to the basic needs of children with cancer and their families in terms of INPUT and INTERVENTION. This essential service package, customized for Iran's social and cultural context, offers safe, efficient, convenient, and affordable services in appropriate settings. It can be integrated into primary care by physicians and nurses with primary training, emphasizing the need for PC.