1. Background
Gastric cancer is a disease with a poor prognosis and a high mortality rate (1). According to the International Association of Cancer Registries (IACR), gastric cancer is the 5th leading cause of illness after breast, lung, colorectal, and prostate cancer, and the 4th leading cause of death worldwide, following lung (18.0% of the total), colorectal (9.4% of the total), and liver cancers (8.3% of the total) in the global population in 2020. The Global Cancer Observatory (GLOBOCAN) report indicates that more than 1 million new cases (5.6% of the total) of gastric cancer and 769,000 related deaths (7.7% of the total) were registered (2, 3). In Iran, gastric cancer is the most common cancer in men and the second most frequent cancer in women, following breast cancer (1). In 2018, Iran ranked as the 8th country globally in terms of the mortality rate index due to gastric cancer (4). Although incidence and mortality rates of gastric cancer have decreased in most countries, its burden remains high in several regions of Asia, Latin America, and Central and Eastern Europe (5). The incidence of the disease is highly dependent on geography and sex. Geographically, more than half of all gastric cancer cases occur in Asia (6). In Iran, the northern and northwestern regions are considered high-risk areas, while the central and western provinces are at medium risk, and the southern areas are at low risk (7-9). The incidence of gastric cancer has significantly increased in Iran, particularly in northern regions such as Mazandaran province (1, 10, 11). Gastric cancer incidence is 2.2 times higher in men than in women; however, this ratio is 1.83 in developing countries (4). Moreover, it is the most commonly diagnosed and leading cause of cancer-related mortality in men in several countries of South and Central Asia, including Iran (3). According to GLOBOCAN statistics 2020, the age-standardized rates (ASRs) for gastric cancer were 22.4 and 12.5 for men and women in Iran, respectively (12).
2. Objectives
The present study aimed to analyze the incidence trends of gastric cancer in Mazandaran province between 2014 and 2018.
3. Methods
A cross-sectional study was conducted using data from the Mazandaran Cancer Registry Center. The Mazandaran Population-Based Cancer Registry has been a voting member of the IACR since 2019. Data were collected based on a national guideline for population-based cancer registries. According to this guideline, the Mazandaran population-based cancer registry recorded new primary tumors with malignant behavior. Only the initial primary tumors were documented for cases involving metastasis or recurrence, following the multiple primary rule established by the International Agency for Research on Cancer (IARC) (8).
The main sources for data collection included pathology reports from pathology centers, clinical/paraclinical data from hospitals, and the death registry programs. Exclusion criteria included individuals who were not citizens of Mazandaran province. Data on cancer mortality were also obtained from the Mazandaran Death Registry Unit in the Deputy of Health at Mazandaran University of Medical Sciences. Finally, cancer mortality data were linked to the incidence data to identify cases with death certificates only. The code for gastric cancer — C16 — was used according to the 3rd edition of the international classification of diseases for oncology (ICD-O-3) (13). Data processing and quality control were performed based on the national guideline (8).
To minimize bias in the study, the initial data collected from the aforementioned sources were coded by an experienced expert. Additionally, a quality supervisor evaluated the coded data to ensure its integrity and reliability. In cases of doubt or ambiguity regarding the data, consultations with a pathologist and an oncologist were sought to provide further insights and validation.
Using the world standard population as a reference, we estimated crude rates and ASRs of incidence per 100,000 population. Population data for Mazandaran province were obtained from the statistics office of the Deputy of Health at Mazandaran University of Medical Sciences. This approach aimed to identify possible joinpoints, where a significant change in the trend occurred. Trends and average annual percentage change (AAPC) of the incidence rate, with 95% confidence intervals (CI), were calculated using joinpoint regression analyses. The Joinpoint Regression Program (version 4.9.0.0) was used for regression analyses. A P-value of less than 0.05 was considered statistically significant (P < 0.05) for describing the trends. All statistical tests were two-sided. This study was approved by the Ethics Committee of Mazandaran University of Medical Sciences (IR.MAZUMS.REC.1402.11764).
4. Results
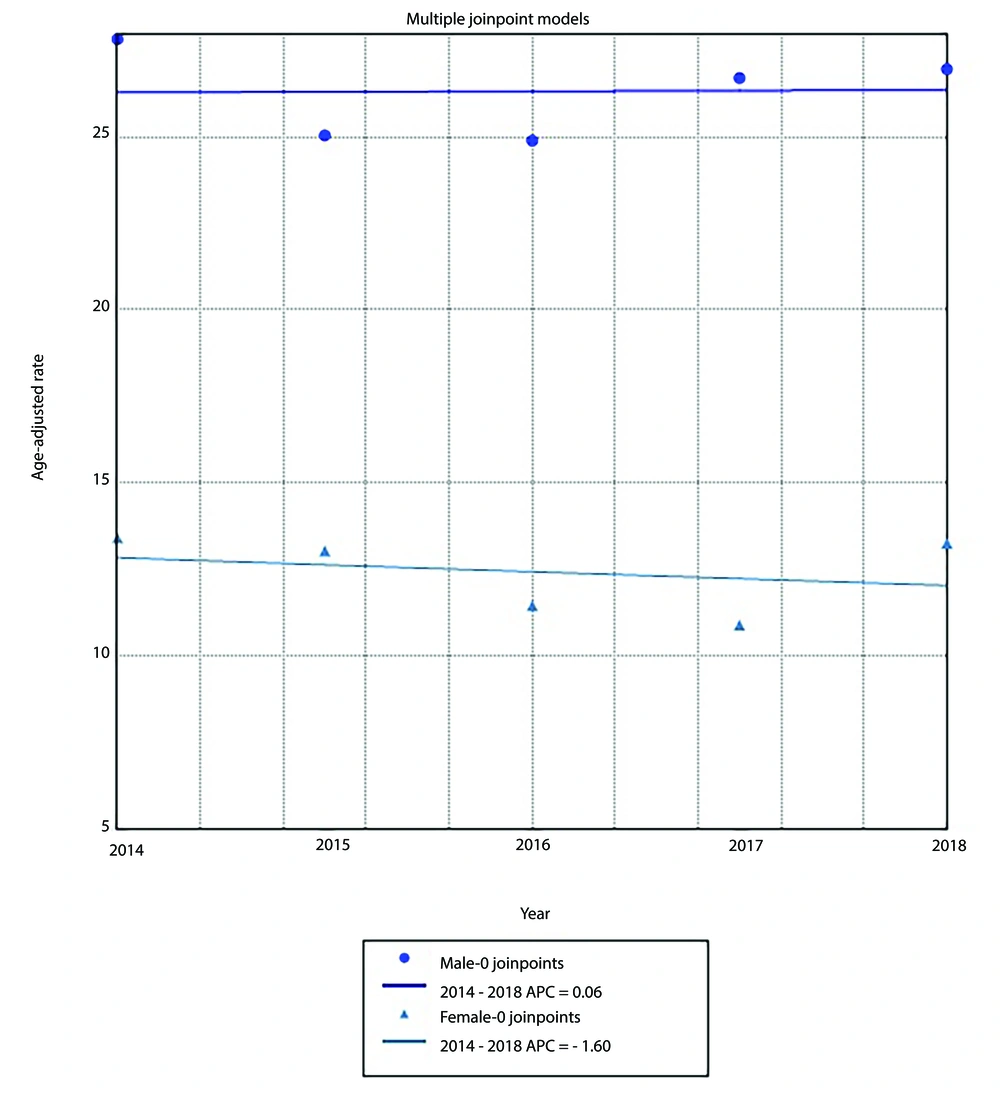
A total of 3,473 new gastric cancer cases were identified from 2014 to 2018 in Mazandaran province, comprising 2,365 males (68%) and 1,108 females (32%), resulting in a male-to-female incidence ratio of 2.13. The mean age of the patients was 68.3 ± 13.9 years, with mean ages of 67.2 ± 14.9 years for female patients and 68.9 ± 13.4 years for male patients (P < 0.001). The number of new gastric cancer cases in males increased from 411 to 525 between 2015 and 2018, with an average of 473 new cases per year, and an average ASR of 26.28. In females, gastric cancer cases ranged from 202 to 260, with an average of 221 new cases per year. The ASRs in females increased from 10.9 to 13.41 between 2014 and 2017. Overall, 1,445 (48.1%) patients resided in rural areas, while 1,560 (51.9%) lived in urban areas. Table 1 presents the number of new cases of gastric cancer, along with crude and age-standardized incidence rates (per 100,000 population) in male and female populations in Mazandaran province from 2014 to 2018, categorized by sex, residential area, and calendar years. Figure 1 illustrates the age-standardized incidence rates of gastric cancer in both sexes in Mazandaran between 2014 and 2018.
| Variables | Female | Male | ||||||
|---|---|---|---|---|---|---|---|---|
| Number | Crude Rate | ASR | 95% CI of ASR | Number | Crude Rate | ASR | 95% CI of ASR | |
| Residence | ||||||||
| Total | 952 | 11.9 | 12.4 | 6.09 - 18.63 | 2053 | 25.0 | 26.3 | 11.62 - 40.98 |
| Rural | 447 | 13.1 | 10.0 | 4.10 - 14.98 | 998 | 28.4 | 22.8 | 10.51 - 35.05 |
| Urban | 505 | 11.0 | 11.3 | 5.38 - 17.26 | 1055 | 22.4 | 23.2 | 9.76 - 36.64 |
| Year | ||||||||
| 2014 | 219 | 14.1 | 13.4 | 6.83 - 20.01 | 458 | 28.7 | 27.8 | 12.50 - 43.18 |
| 2015 | 211 | 13.4 | 13.0 | 5.57 - 20.50 | 411 | 25.3 | 25.1 | 10.51 - 39.59 |
| 2016 | 202 | 12.6 | 11.4 | 5.42 - 17.50 | 445 | 27.0 | 24.9 | 10.84 - 38.96 |
| 2017 | 214 | 13.0 | 10.9 | 5.69 - 16.11 | 524 | 31.4 | 26.7 | 11.84 - 41.54 |
| 2018 | 260 | 15.7 | 13.3 | 6.10 - 20.40 | 525 | 31.2 | 27.0 | 11.84 - 42.10 |
Abbreviation: ASR, age-standardized rate; CI, confidence interval.
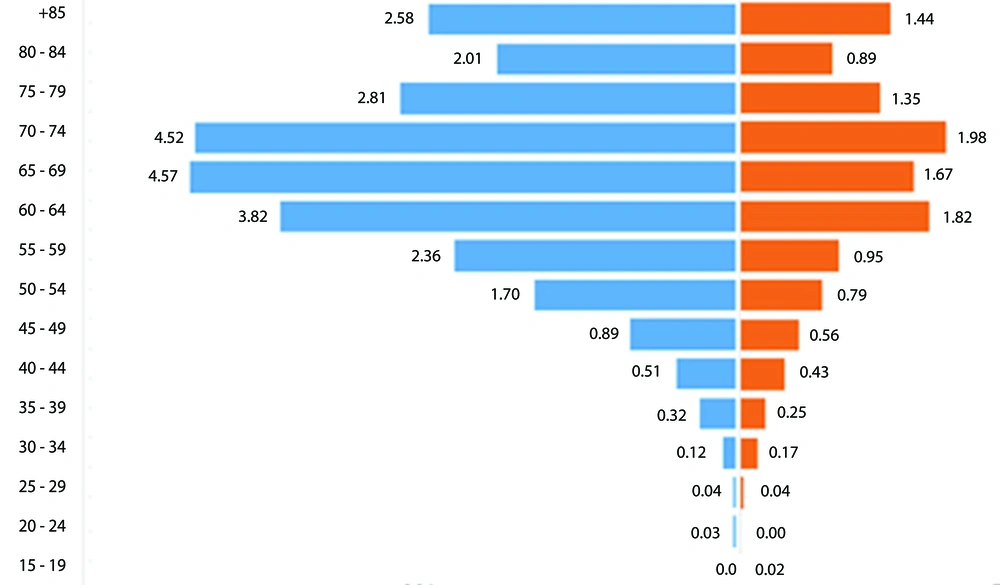
According to the findings, approximately 40% of new cases were registered in the 50 - 69-year age group. Within this group, the frequency of new cases was not significantly higher in males compared to females (39.83% vs. 37.55%; P = 0.2). Overall, 74.2% of patients were over 60 years of age at the time of diagnosis. Conversely, new gastric cancer cases were significantly more frequent among females than males in the 30 - 39-year and 40 - 49-year age groups (Table 2).
| Age-Group | Total | Male | Female | P-Value |
|---|---|---|---|---|
| 0 - 19 | 2 (0.1) | 1 (0.04) | 1 (0.1) | 0.58 |
| 20 - 29 | 11 (0.3) | 7 (0.30) | 4 (0.3) | 0.75 |
| 30 - 39 | 107 (3.1) | 55 (2.33) | 52 (4.7) | 0.0 |
| 40 - 49 | 228 (6.5) | 134 (5.67) | 94 (8.5) | 0.002 |
| 50 - 59 | 549 (15.8) | 382 (16.15) | 167 (15.1) | 0.42 |
| 60 - 69 | 809 (23.3) | 560 (23.68) | 249 (22.5) | 0.43 |
| 70 - 79 | 912 (26.3) | 629 (26.60) | 283 (25.5) | 0.51 |
| + 80 | 855 (24.6) | 597 (25.24) | 258 (23.3) | 0.21 |
| ∑ | 3473 | 2365 | 1108 | - |
a Values are expressed as No. (%).
The ASR of gastric cancer was significantly higher in men (26.28) than in women (12.36) (P < 0.001). Joinpoint regression analysis indicated an insignificant decrease in the incidence trend for both males (AAPC = 0.1%; 95% CI, -5.2 to 5.6; P = 1.0) and females (AAPC = -1.6%; 95% CI, -11.2 to 9.1; P = 1.0) from 2014 to 2018. Figure 2 illustrates the incidence trend based on age-standardized incidence rates in male and female patients in Mazandaran province between 2014 and 2018. The model summary indicates a weak correlation (R = 0.076) between the predictors (ASR in males and females) and the dependent variable (year), with only 0.6% of the variance explained (R2 = 0.006).
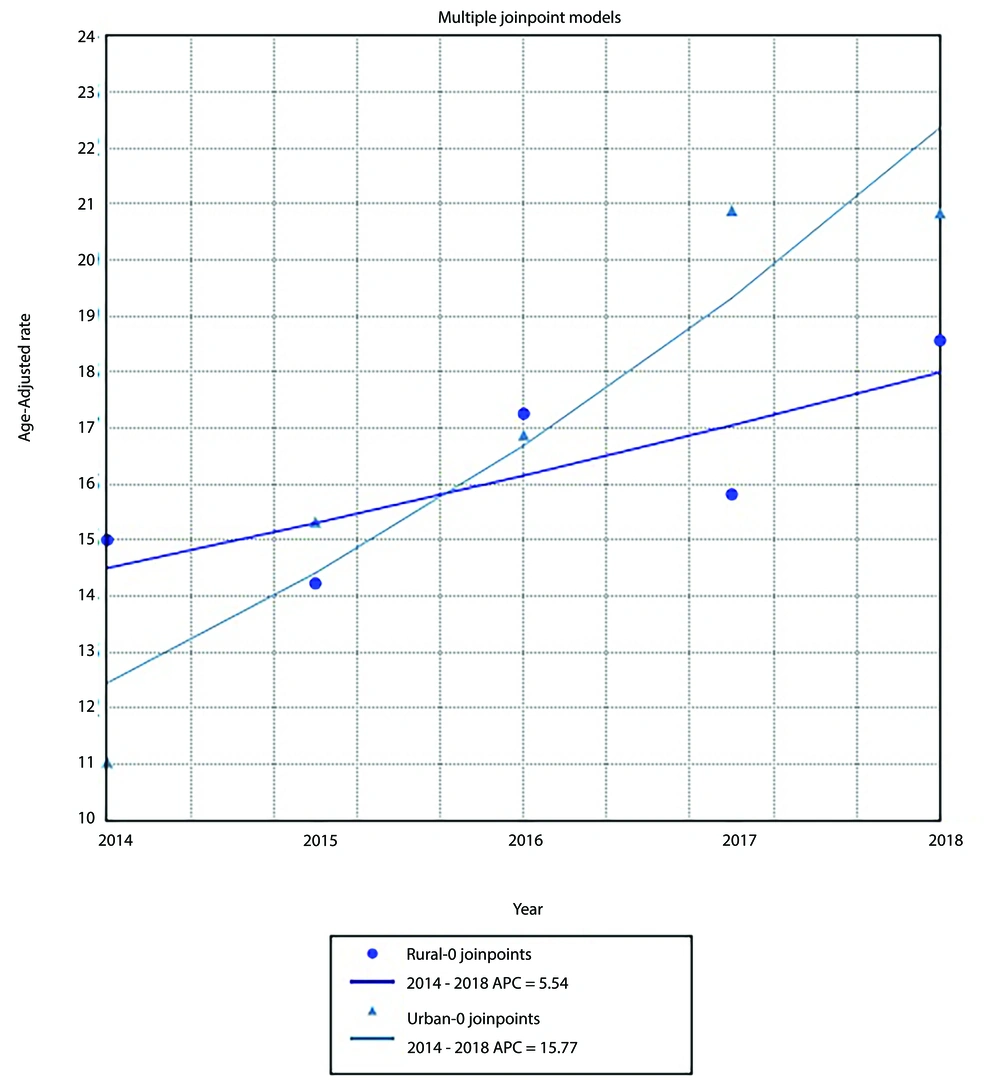
Figure 3 demonstrates a statistically significant increase in the ASR for gastric cancer incidence in urban areas (AAPC = 15.8%; 95% CI, 4.7 to 28.0; P < 0.01). Conversely, a non-significant increase in gastric cancer incidence was observed in rural areas during the study period (AAPC = 5.5%; 95% CI, -2.3 to 14.0; P = 0.1). The model summary indicates a weak correlation (R = 0.287) between the independent variables (ASR in rural and urban areas) and the dependent variable (year), accounting for only 8.2% of the variance (R2 = 0.082).
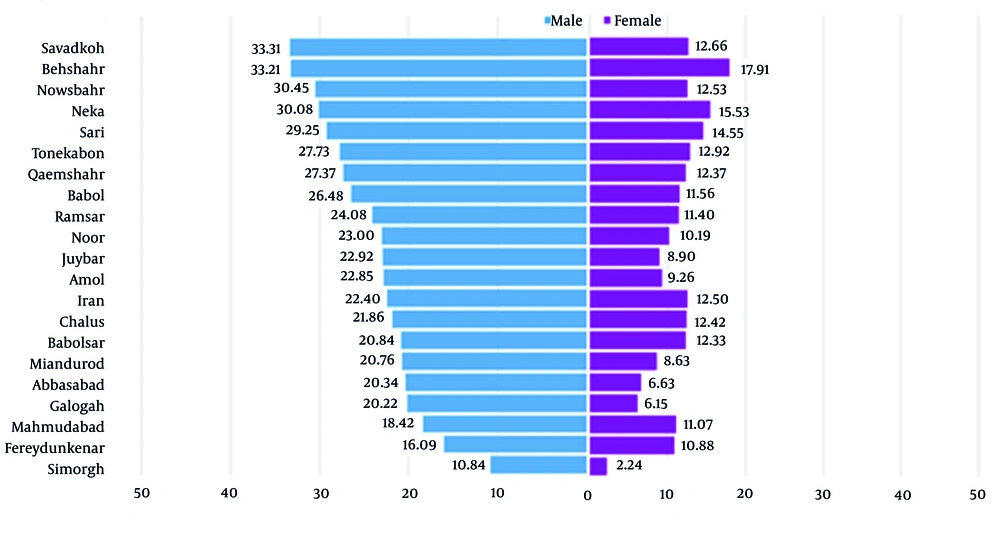
According to Figure 4, the incidence rates of gastric cancer vary across different parts of the province, with higher rates observed in the central and western regions (ASR = 33.31 in men and 12.66 in women) and lower rates in the northern and northwestern areas (ASR = 10.84 in men and 2.24 in women), including Simorgh, Fereydunkenar, and Mahmudabad.
5. Discussion
The 5-year incidence trend of gastric cancer was assessed by age and sex in Mazandaran province, located in northern Iran. The ASRs of gastric cancer were 26.3 in men and 12.4 in women. According to the GLOBOCAN 2020 estimates, the worldwide ASRs of gastric cancer were 15.8 for men and 7.0 for women (3). A slight decrease in gastric cancer incidence has occurred worldwide over time, even in high-risk countries such as Japan and China (14). Factors contributing to this decline include antibiotic treatments, prevention programs, early detection programs, improved medical treatments, and changes in dietary habits, with increased consumption of fresh vegetables and fruits instead of salty, canned, and processed foods (15). Based on the Iranian National Cancer Registry’s report, the ASRs of gastric cancer in Iran were 21.2 in men and 9.4 in women (10), indicating an increase in the incidence of gastric cancer in Iran for both sexes. However, the incidence of gastric cancer varies across different geographical areas of Iran, with low risk in the central and eastern parts and high risk in the north and northwest of the country, including Mazandaran province (10).
Previous studies confirm that Mazandaran province is a high-risk region (11, 16). This may be partly due to the establishment of a cancer registration system in the country, other factors that increase the risk of the disease (17), and Helicobacter pylori infection (18), a significant risk factor for developing gastric cancer (19, 20). Malekzadeh et al. (16) and Kalan Farmanfarma et al. (21) observed a high prevalence of H. pylori infection in Iran. Similarly, Talebi Bezmin Abadi et al. (20, 22, 23) confirmed a high prevalence of this infection in Mazandaran province. Based on Maleki et al. (24) reports, the prevalence of Helicobacter infection was 44.5% in Sari city and its surrounding rural area, 41.3% and 47.8% in urban and rural areas, respectively. Other risk factors include changes in the microbial environment of the stomach, gastroesophageal reflux disease, low socioeconomic status, genetic predisposition, and lifestyle risk factors (smoking, alcohol, and diet) (16, 21, 25). Kalan Farmanfarma et al. (21) reported a direct relationship between gastric cancer and consuming processed red meat, dairy products, fruit juice, smoked and salty fish, strong and hot tea, and salt. Foods such as fish, fruit, fresh vegetables, rice, salted foods, and dairy products are abundant in the dietary patterns of families in Mazandaran (26). In addition, 14% of the Iranian population uses tobacco, with men smoking six times more than women. According to the World Health Organization (WHO), the burden of tobacco-related diseases is rising in developing countries such as Iran (27); Moosazadeh et al. (27) report a high smoking prevalence in men in Mazandaran province. Hence, these risk factors may partially explain the high incidence rate of gastric cancer in this region. Similar to Aghaii et al. (28) and Mousavi et al. (1), who reported sex ratios of 1.99 and 2.15, this study showed that the sex ratio (male to female) was 2.13, and the incidence rates among males were significantly higher than females in all groups. The findings did not identify clear reasons for the higher incidence of gastric cancer in men, but risky behaviors such as occupational exposure to high levels of radiation and toxic substances, smoking, alcohol, and consumption of red and salty meat, especially roasted meat, may play a role. The mean age values of patients in males and females were 68.9 and 67.2 years at the time of diagnosis, respectively, which are consistent with the results of Mousavi et al. (1) (males: 65 vs. females: 63.7 years), Ghasemi-Kebria et al. (10) (males: 65.3, females: 62.6 years), and Nikpour et al. (29) (males: 65.68, females: 64.26 years). Furthermore, this study showed an increasing trend of gastric cancer in the middle-aged population, increasing with age. The most newly registered cases in both sexes were in the age group of 70 to 79. Although gastric cancer is not common in young people, recent reports show that the incidence of the disease increases in people younger than 40, confirmed by Moghimi Dehkordi et al. (30) (46.2 years). These findings align with previous reports, suggesting age is a risk factor for gastric cancer (10, 25). According to our results, the rate of gastric cancer in urban residents has been higher than in rural residents since 2016, which may be partly explained by lifestyle changes, owing to fast food consumption, canned, processed, smoked, and fermented foods, food additives and preservatives, as well as unsafe and unsanitary drinking water, and low physical activities (10). However, these results differ from some data published by Yazdani Charati et al. (31) and Ghasemi-Kebria et al. (10), showing the trends are rising in urban and rural areas. The reasons for this trend in rural areas are not entirely well-understood, yet it could be due to low knowledge of disease preventive practices, low socioeconomic status, drinking un-piped water, exposure to agricultural pesticides, poor hygiene, no access to specialists and modern diagnostics, and other occupational and environmental factors. In addition, due to the high diagnostic and paraclinical costs, rural residents are less likely to recognize the disease in the early phase (10, 31). Further investigations are needed to clarify this matter. The present study showed a diverse geographic variability in incidence rates of gastric cancer in Mazandaran province. The cancer incidence due to environmental factors is not similar in different geographical regions (32). These results are relatively similar to the results of Yazdani Charati et al. (31). The present study reveals that the incidence rate of gastric cancer is high in Savadkoh, Behshahr, and Nowshahr and low in Simorgh, Fereydunkenar, and Mahmudabad. In addition, cultural food habits, climate variety, low temperatures, and rainfall, which result in high levels of nitrate in water and low sunshine duration, may explain these trends (11, 33). However, this issue should be taken into account in future studies. The findings of this study on the incidence trends of gastric cancer in Mazandaran province from 2014 to 2018 have important implications for local healthcare providers, policymakers, and public health officials, particularly in addressing increases in incidence among older populations and urban areas. These results can inform targeted screening and prevention strategies, influence public health policies to enhance early detection and intervention, and guide research and resource allocation to explore contributing factors such as lifestyle and environmental influences. Additionally, the urban-rural disparity in gastric cancer incidence through targeted public health policies and interventions can significantly improve the burden of gastric cancer across rural populations. The findings of this study can be valuable insight for healthcare providers in developing screening programs in other regions that share similar demographic, environmental, healthcare, and cultural characteristics. The most important limitation of this study was the relatively small nature of population-based cancer registry data, as other potential confounding variables such as dietary habits, family history, smoking and waterpipe habit, and environmental factors were not evaluated.
5.1. Conclusions
Our findings confirmed high incidence rates of gastric cancer in Mazandaran province. The incidence of gastric cancer has remained unchanged in men, but it continues to be a predominant disease among them. We observed a slight decline in gastric cancer incidence in women. Gastric cancer was approximately 2.1 times more common in men than in women. Additionally, the study demonstrated that the incidence rates of gastric cancer were considerably higher in the central parts of Mazandaran. Therefore, gastric cancer should be prioritized by local health policymakers in this region. Further studies are needed to identify the most critical risk factors for gastric cancer in Mazandaran.