1. Introduction
Breast cancer, one of the most common malignant tumors in women, has a relatively low incidence in developing countries. However, with socio-economic development, the incidence of BC is increasing, and the mortality rate remains persistently high. According to the latest data from 2020, BC accounted for 2.26 million new cases worldwide, surpassing lung cancer (2.2 million cases) to become the most commonly diagnosed cancer globally (1, 2). In the evaluation of the quality of life during the recovery period of BC, the quality of sexual life is one of the indicators to measure the recovery after treatment, and the recovery of sexual function also reflects the recovery of the whole body condition (3). Therefore, sexual health has become an urgent concern for patients with BC after surgery. The traditional intervention model, to some extent, caused effects on sexual life. Especially in the early stages of the disease, fear, anxiety, depression, and other emotions can strike sexual desire, thus reducing the quality of sexual life in patients with BC (4). An increasing number of researchers have begun to focus on this issue. Cognitive behavioral therapy and mindfulness reduction methods are currently non drug intervention methods to improve sexual dysfunction after BC surgery, aiming to improve the sexual psychology of patients through psychotherapy and other methods (5). A meta-analysis found that approximately 68% of patients with BC lack sexual knowledge, and about 87.6% of patients desire to learn about sexual health. However, only around 26.9% of healthcare providers actively offer sexual guidance to patients. Sexual care counseling and health education can effectively reduce the occurrence of sexual dysfunction (6).Therefore, clinical evidence suggests that educational interventions and sexual health nursing consultation model can alleviate doubts about this aspect of sexual life among patients with BC, reassure them about the impact of sexual activity on their quality of life after treatment, and ultimately enhance their sexual well-being (7).
2. Objectives
There are few studies on the sexual life of patients with BC. The aforementioned research is relatively limited, as it conducted a meta-analysis on the factors influencing sexual dysfunction in patients with BC but did not provide a comprehensive discussion on sexual health education. The present study aimed to supplement that aspect. This meta-analysis also aimed at analyzing the impact of sexual counseling and educational intervention on the sexual function of patients with BC from the indicators of orgasm, sexual function, sexual arousal, sexual desire, sexual intercourse difficulty, sexual satisfaction. Through this meta-analysis of sexual care counseling and education for patients with BC, the importance and necessity of applying sexual care counseling and education models to improve the sexual quality of life for patients with BC have been recognized. It also provides direction and inspiration for healthcare professionals and researchers to offer higher-quality sexual health education guidance.
3. Methods
A meta-analysis was prepared according to the CRD guidelines, and based on MOOS guidelines reports, the selection process for included studies was based on the PRISMA-P checklist.
3.1. Sources and Searches
A comprehensive literature search was conducted for nearly three years up to March 2023 for research questions (8). A comprehensive literature search was conducted in PubMed, CNKI, and Web of Science using the keywords "sexual function", "breast cancer", "RCT" and "sexual function". The search strategy included variations in spelling (e.g., American vs. British English), plural forms, and relevant prefixes and suffixes to ensure broad coverage across databases.
In retrieving the CNKI database, the search consisted of the following word combinations "breast cancer" AND "sexual function". The search term of PubMed was "breast cancer" OR "sexual function". Web of Science’s search term was "breast cancer" AND "sexual function" (9).
To make the document retrieval more effective, PubMed and Web of Science were subject to date restrictions (2020 - 2023.3). In PubMed, the article type was limited to randomized controlled trials (RCTs), while in Web of Science, only articles classified as 'papers' were included. All selected studies were downloaded directly from the original websites.
The CNKI was subject to a time limit from 2020 to 2023. The download source was direct download through the intranet of Hangzhou City University Library. During the initial screening, articles were selected for analysis if the terms "sexual function" and "breast cancer" appeared in the title or abstract.
This process allowed for the initial selection of relevant literature. Subsequently, manual searches were conducted to identify additional studies, with secondary searches performed based on the titles and content of previously retrieved articles across the three major databases to ensure comprehensive coverage. The source of downloads remained consistent with the methods described above (10).
In PubMed, the search terms "sexual function" and "cancer" were used for preliminary screening. Articles were first assessed based on their relevance to cancer surgery and whether the study type was a randomized controlled trial (RCT). To ensure accuracy, a two-step screening process was conducted, reviewing the literature for the presence of the keywords "sexual function", "cancer", and "RCT", and confirming that the studies were classified as RCTs. Finally, the remaining articles were reviewed in full, and the final selections were made based on the predefined inclusion and exclusion criteria.
3.2. Study Selection
Articles were initially selected independently by two researchers and subsequently evaluated jointly based on full-text content and quality. Decisions regarding inclusion or exclusion were made through discussion and consensus, and when necessary, in consultation with a senior author or supervisor (11).
Eligibility criteria based on participants, exposures, outcomes and study design (PEOS) elements (12) were as follows.
3.2.1. Study Inclusion Criteria
(1) Studies included participants who met the clinical diagnostic criteria for BC based on standard guidelines in obstetrics and gynecology (13).
(2) Eligible studies were prospective in nature, including single-arm clinical trials or RCTs.
(4) Studies that implemented different intervention modalities — especially counseling-based approaches — were considered, provided the interventions were deemed effective and relevant to the study’s objectives.
(5) Studies were required to present outcome values in formats such as mean and standard deviation (SD), 95% confidence intervals (CI), standard error, or P < 0.05. Availability of a t-value for the calculation of SD was also acceptable.
(6) Studies that their reports values were presented as mean and SD or 95% CI, standard error, or P < 0.05. T-value was available to calculate the mean ± SD.
3.2.2. Study Exclusion Criteria
(1) Descriptive studies, retrospective studies, and case-control studies, as well as studies without full-text availability, conference abstracts, and review articles (as outlined in Figure 1 supporting the study selection process).
(2) Studies in which the outcome measures focused solely on anxiety, depression, or surgical effects, without evaluating sexual function.
3.3. Data Extraction
Data extraction and analysis were independently conducted by two investigators using standardized forms. The process followed the guidelines outlined in Table 7.3a of the Cochrane Handbook for Systematic Reviews of Interventions (14), which lists essential items for data collection, and Section 11.3a, which details the information required for generating forest plots. Key data collected included sample size (number of participants), means, and SDs (Figure 2).
For each article meeting the inclusion criteria, the following information was extracted: First author, year of publication, purpose of the study, cohort/study name, study design, target population and sample size, follow-up data, participant age, corresponding mean ± SD or 95% CI for each relevant parameter (FSFI) extracted from the results table, P-value and t-value for patients with different BC standard errors, types of interventions, outcome measures, and measurement instruments. This information was used to assess eligibility based on the study’s inclusion and exclusion criteria (15).
Any missing or incomplete data has been excluded from the extracted data and were resolved perfectly by discussion with the senior author.
3.4. Quality Assessment
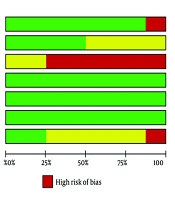
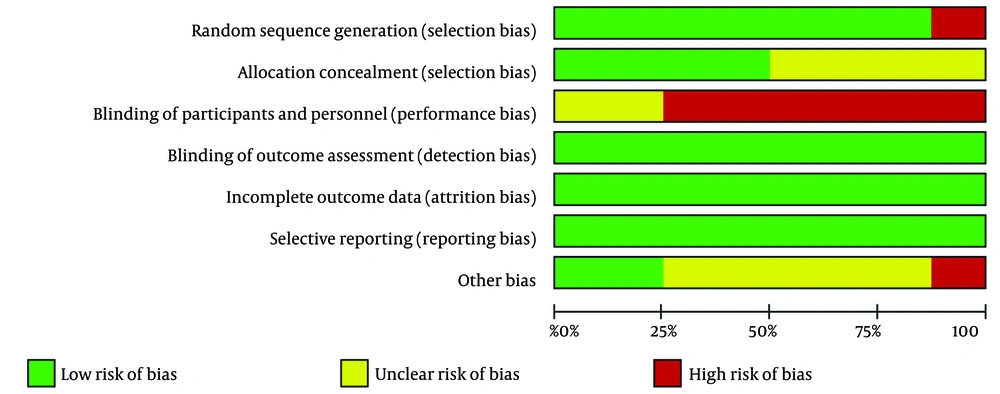
As shown in Figure 3, the quality assessment of the included articles was performed by the Software Review Manager 5.4.1 (16) and 7 items were assessed:
(1) Random sequence generation (selection bias)
(2) Allocation concealment (selection bias)
(3) Blinding of participants and personnel (performance bias)
(4) Blinding of outcome assessment (detection bias)
(5) Incomplete outcome data (attrition bias)
(6) Selective reporting (reporting bias)
(7) Other bias
The quality of the studies was independently assessed by two investigators (ZH Shou and ZC Lin) to ensure accuracy and reliability.
To assess methodological quality, we analyzed each article based on several criteria. The first criterion involved evaluating the method of randomization, including whether random tables, computer generators, flip coins, cards, and draw lots were used. The second criterion focused on allocation concealment such as central randomization (telephone, network, pharmacy control randomization) and envelope. The third criterion was based on blinding — specifically, whether participants, researchers, or outcome assessors were aware of the group assignments or interventions, categorized as single-blind, double-blind, or triple-blind. According to the result measurement method: Questionnaire form, follow-up data analysis, and research result analysis, we assessed the final remaining standard (17, 18).
Any differences in the quality of the included studies were resolved by discussion, if required, in consultation with the senior author.
3.5. Statistical Analysis
3.5.1. Exposure Assessment
Sexual function, the main exposure factor in this study, was defined as the physiological, psychological and other responses of humans at different stages of the sexual response cycle (19). Table 1 summarizes the nursing consultation and educational treatments, lectures, video conversations, and psychological interventions delivered under consultation modes for patients with BC. These methods can help alleviate sexual distress, reduce anxiety, and improve self-image awareness in patients. Sexual function indicators were assessed with libido, sexual arousal, vaginal lubrication, orgasm, sexual satisfaction, dyspareunia.
| Authors and Publication Year | Study Design | Participants | Sample Size | Intervention | Outcome Measure | Age at Baseline (y) |
|---|---|---|---|---|---|---|
| Reese et al. (20), 2021 | 2-month follow-up | BC patients | 144 women | Multimedia intervention | FSFI | 55.8 ± 11.2 |
| 56.1 ± 10.9 | ||||||
| Liu (21), 2022 | 3-month follow-up | BC patients | 70 patients | WeChat continuous nursing | FSFI | 35.42 ± 3.16 |
| 35.49 ± 3.27 | ||||||
| Bokaie et al. (22), 2022 | Eight 90-min sessions | BC patients | 32 women | Group problem-solving therapy | FSFI | 39.81 ± 7.54 |
| Hamidi et al. (23), 2021 | Eight 45-min intervention | BC patients | 316 women | FSFI | 40.23 ± 5.87 | |
| 40.50 ± 6.28 | ||||||
| Kang et al. (24), 2022 | 6-months follow-up | BC patients | 109 women | Mind and body education | FSFI | 35.3 ± 3.9 |
| 36.1 ± 3.6 | ||||||
| Olcer and Oskay (25), 2022 | 1-months follow-up | BC patients | 60 women | BETTER model | FSFI | 40.6 ± 4.7 |
| BCS | 40.0 ± 4.4 | |||||
| de Almeida et al. (26), 2020 | 3-months follow-up | BC patients | 18 women | PLISSIT model | FSFI | 54.58 ± 7.14 |
| Keshavarz et al. (27), 2021 | 4-week follow-up | BC patients | 65 women | PLISSIT model | FSFI | 43.4 ± 5.6 |
Characteristics of Included Trials on Sex Function for Breast Cancer Patients
3.5.2. Outcome Assessment
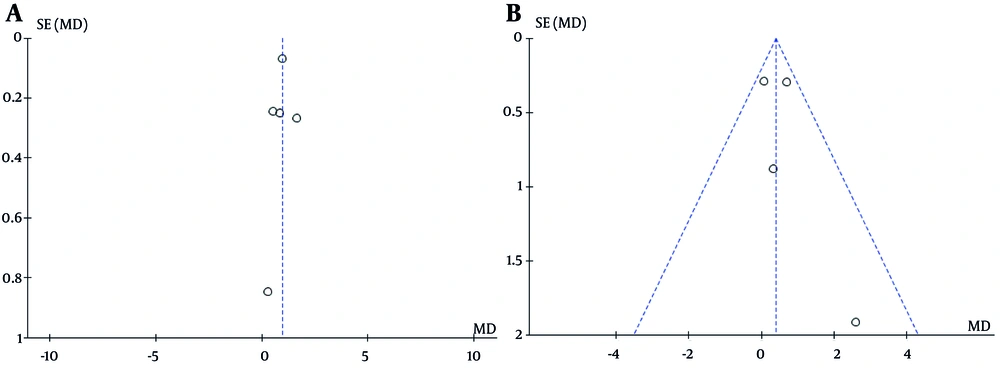
RevMan 5.4.1 software was used to analyze the extracted data. Continuous outcomes were analyzed by standardized mean difference (SMD). Hazard-ratios were calculated for the two groups of outcomes. Point estimates 95% CIs, and P-value were used to report the results. A P < 0.05 was considered statistically significant. The I2 test was used to determine whether there was heterogeneity across studies. P-value > 0.05 or I2 > 50% was interpreted as high heterogeneity, and the random effects model was used for analysis. Funnel plots were used for different surgical effects. Funnel plot is the most commonly used method to identify publication bias in meta-analysis, which reflects the estimated intervention effect of a single study under a certain sample size or accuracy. We assessed publication bias in the included studies by observing funnel plot images. As shown in Figure 3A and B the midpoint of the image is clustered into an inverted funnel shape, which shows that the publication bias of the included studies is small. Sensitivity analyses examined the robustness and reliability of the pooled results by excluding each study in turn (28).
4. Results
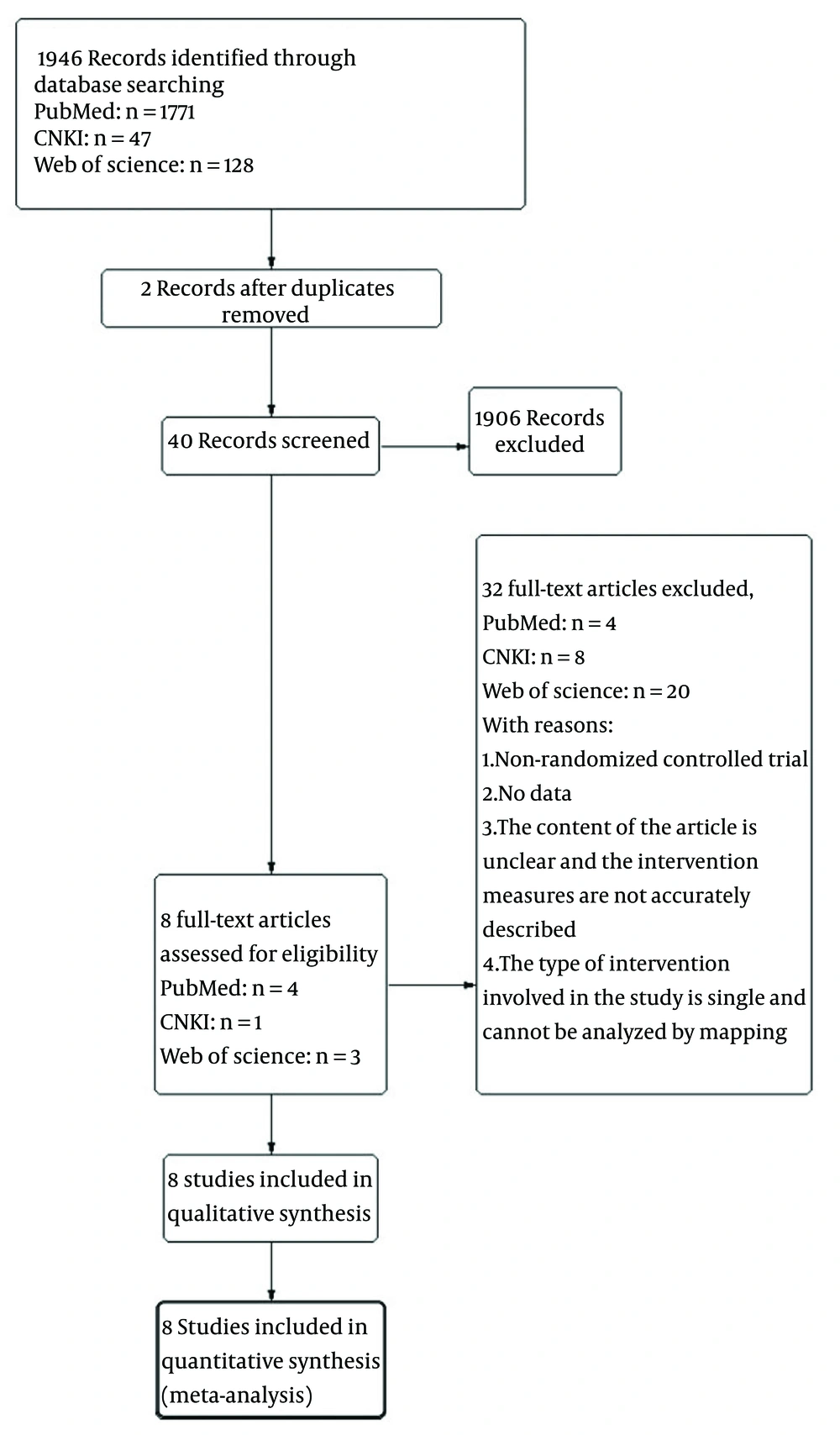
The research selection process and literature search results are shown in Figure 1, using the PRISMA flowchart. After removing the duplicate documents, a total of 1771 records were identified in the initial document retrieval. After screening the title, theme and abstract, and carefully reviewing the full text, eight eligible studies were included, which met the inclusion criteria and were all RCTs. A total of 814 independent participants were all female with BC after treatment in an average age of 27 to 45 years. The follow-up period was one week to six months. Forest plots were produced using Rev Man 5.4.1.
4.1. Quality of Sexual Life
Sexual nursing consultation and education could improve the quality of sexual life in patients with cancer. Quality of sexual life was divided into sexual desire, sexual arousal, vaginal lubrication, orgasm, dyspareunia and sexual satisfaction. According to which we conducted a research analysis.
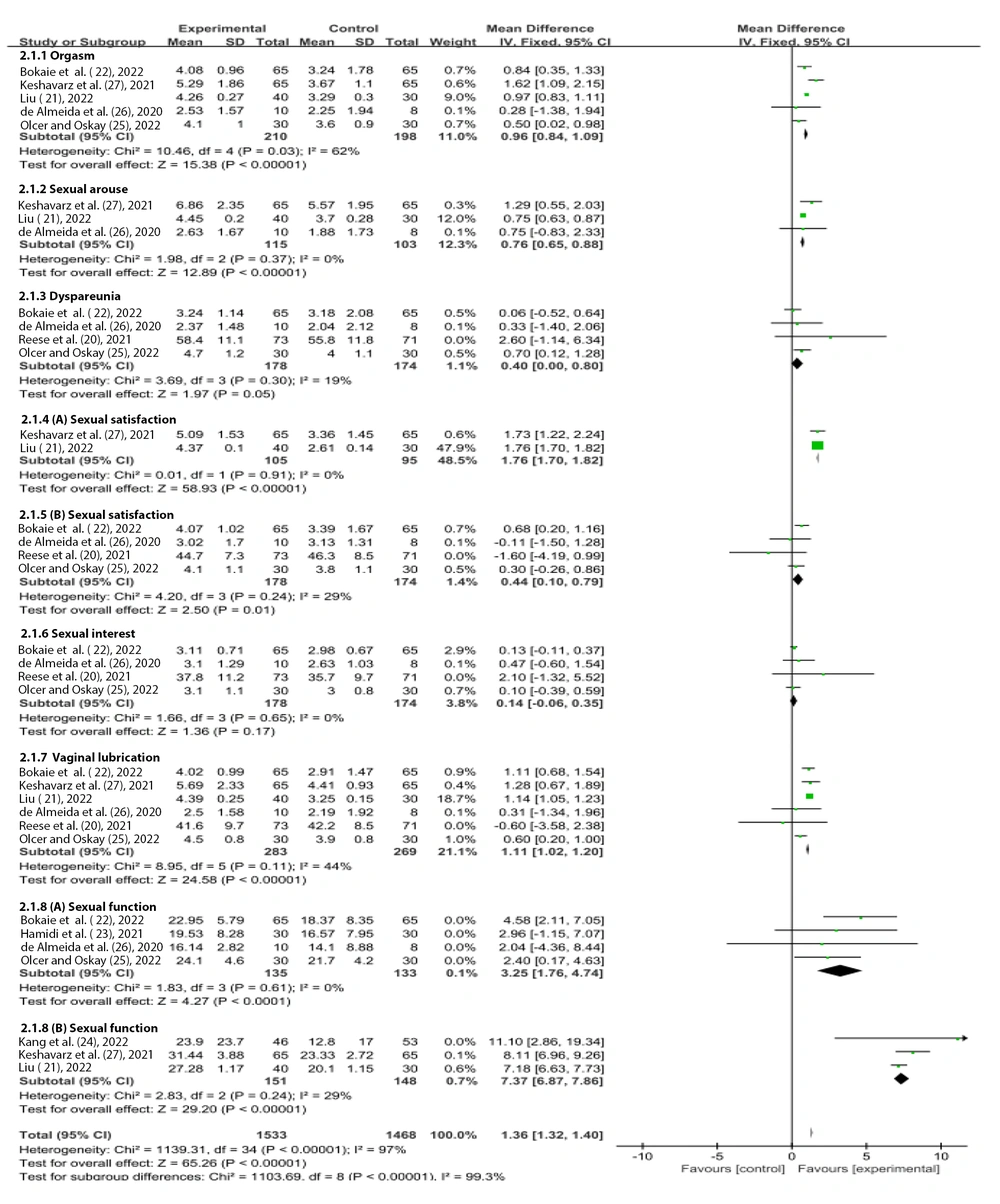
4.1.1. Orgasm
Orgasm in patients with BC (20, 21, 24-27) can be improved by sexual counseling and education. Figure 4 shows that the SMD of the post-intervention values was 0.95 (95% CI = 0.61 - 1.28), Z = 5.56, P < 0.00001, I2 = 62%. From the above data, it is evident that there is high heterogeneity among studies, which was demonstrated by using a random effects model, but also suggests a statistically significant difference in outcomes between the intervention and control groups. This trial can significantly impact the culminating experience of post-treatment experience of patients with BC after sexual nursing consultation and psychoeducation.
4.1.2. Sexual Arousal
Figure 4 also illustrates that WeChat continuity care and PLISSIT consultation mode had a positive effect on sexual arousal in BC patients (21, 24, 27). The SMD of its prognostic change value was 0.76 (95% CI = 0.65 to 0.88), Z = 12.89, P < 0.00001. The pooled effect size was statistically significant, with no observed heterogeneity among studies, indicating that the intervention had a significant effect on post-treatment sexual arousal in BC patients.
4.1.3. Dyspareunia
The multimedia intervention, group discussion therapy, and the PLISSIT counseling model also had a positive effect on patients’ existing dyspareunia after BC treatment. Figure 4 shows that the SMD of their prognostic change value was 0.4 (95% CI =1.97 - 0.8), Z = 1.97, P = 0.05. I2 = 19%, considered the included studies to have low heterogeneity. There was a significant difference between the intervention group and the control group. Concluded that multimedia intervention, group discussion therapy, and other interventions for patients after BC treatment can significantly improve patients’ dyspareunia.
4.1.4. Sexual Life Satisfaction
WeChat continuity care, the PLISSIT counseling model had a positive effect on sexual life satisfaction, existing post-treatment in patients with BC (20, 22, 25, 26). Figure 4 shows that the SMD of prognostic change value was 1.76 (95% CI = 1.7 - 1.82), Z = 58.93, P < 0.00001. P = 0.91, I2 = 0%), there was no heterogeneity among the above studies.
Group problem solving therapy, delivered as a multimedia intervention, demonstrated a same positive significance on post-treatment sexual life satisfaction in patients with BC with the SMD of 0.44 (95% CI = 0.1 - 0.79) (21, 27). The change in prognosis Z = 2.5, P = 0.01. In Figure 4, P = 0.25, I2 = 29%, there was moderate heterogeneity among the studies mentioned above. WeChat continuity of care, group solving therapy, and other interventions for patients after BC treatment can significantly improve their sexual satisfaction.
4.1.5. Libido
Group problem-solving therapy, multimedia intervention, and the PLISSIT model showed no notable effect on libido in BC patients after treatment.
4.1.6. Sexual Interest
According to Figure 4, the SMD for the value of change in prognosis was 0.14 (95% CI = -0.06 - 0.35), Z = 1.36, P = 0.17, P = 0.65, I2 = 0%, there is no heterogeneity between studies, the findings are not statistically significant, indicating that nursing consultation or other interventions may not be effective in addressing ongoing sexual interest among post-treatment patients with BC (20, 22, 25, 26).
4.1.7. Vaginal Lubrication
WeChat continuous care, group problem solving therapy, multimedia intervention, and PLISSIT counseling model had positive significance for vaginal lubrication in post-treatment BC patients. Figure 4 illustrates that the SMD value of their prognostic change was 1.11 (95% CI = 1.02 - 1.20), Z = 24.58, P < 0.00001 (20, 22, 25, 26). Data analysis showed an I2 = 44%, moderate heterogeneity between studies. Nursing consultation intervention, continuing care or other interventions were significantly effective in addressing vaginal lubrication problems present in patients after BC surgery, and the findings were statistically significant.
4.2. Sexual Function
The overall analysis found that WeChat continuing care, mind body education, and PLISSIT counseling model had a positive effect on the sexual function of post-treatment patients with BC (20-22, 25-27). Based on Figure 4 , the SMD of prognostic change value was 7.37 (95% CI = 6.87 - 7.86), Z = 29.20, P < 0.00001. P = 0.61, I2 = 0%), suggested that there were no differences among the studies. Group problem-solving therapy, the Whatsapp intervention also had a positive effect on sexual function in post-treatment patients with BC.
Figure 4 shows that the SMD of prognostic change value was 3.25 (95% CI = 1.76 - 4.74), Z = 4.27, P < 0.0001. P = 0.37, I2 = 0%, indicating that there was no difference between the studies (20, 22, 25, 26).
Combined with the above data analysis, the above interventions had a significant effect on the sexual function of post-treatment BC patients with statistical significance. Sexual nursing consultation and psychoeducational interventions can improve the quality of sexual life of patients after BC treatment.
4.3. Publication Bias
As shown in Figure 3A, the points were all scattered on the top, and were relatively symmetrical, the included studies were considered to free of publication bias. Figure 3B illustrates the effect of sexual counseling and psychoeducation on vaginal lubricity in patients after BC treatment, the graph midpoint was relatively symmetrical and within the 95% interval of the effect size, articles were considered free of publication bias (21, 24, 27).
5. Discussion
The results of the present study demonstrate- that sexual nursing consultation and psychoeducation have a significant impact on the sexual function of patients after BC treatment. The specific intervention types include multimedia intervention, WeChat continuity care, group problem-solving therapy, WhatsApp counseling, mind body education, counseling under the PLISSIT or the BETTER model.
Multimedia intervention (20) focuses on clinical communication about the sexual health of patients after active treatment of BC. By distributing intervention materials to subjects, the intervention materials contained 20min video slide (explained by mobile phone or computer), five pages of work manual on how to communicate and skills training on sexual issues, and two pages of resource guide on information about menopause and sexual health institutions and external resources. The physician-led focus group educates patients about the sexual knowledge, emphasizing that the patient is encouraged to establish self-efficacy and improve the result expectation by learning the skills of effective health.
WeChat continuous nursing (29) mainly intervenes in patients after modified radical mastectomy, establishes professional nursing teams, allows nurses to follow up on WeChat, and ensures that participants are online for one hour a day. It also carries out popular science on BC and postoperative sexual life knowledge through the WeChat platform, and carries out knowledge lectures, psychology expert lectures, and BC rehabilitation exercises. Patients and their spouses are encouraged to engage, speak out, and listen to real feelings and concerns, while caregivers address their questions and provide appropriate responses.
The problem-solving therapy group (22) corrects their misconceptions and improves their depression through sexual counseling and carries out in eight 90-minute counseling sessions for patients after mastectomy within 1 - 5 years.
Counseling (23) aims at improving patient sexual self-concept after BC treatment. Researchers gave themselves personal account number to participants, communicated with patients in the WhatsApp platform, and the activities were conducted in the application. It was conducted in eight sessions of 45 min twice a week. By explaining the anatomy and sexual cycle of men and women, providing corrections after wrong concepts, enhancing self-esteem with confidence in patients’ sexual intercourse, teaching sensory concentration skills and methods, and encouraging patients to evaluate themselves, express feelings about sexual behavior, and also train problem-solving skills and accept supportive relationships.
PLISSIT model (26, 27) begins by addressing patients’ sexual concerns and lack of knowledge. Through sexual psychoeducation and individualized responses to sexual issues, it aims to enhance patients’ comprehensive understanding of sexuality, correct misconceptions, and ultimately improve sexual confidence and satisfaction with sexual life. Whereas in the BETTER model (25), psychological counseling is carried out by issuing counseling manuals and CDs, interviewing participants in appropriate places, and conducting psychological counseling.
Mind body education (25) aimed to improve the quality of life of patients, the intervention was conducted from both the spirit and appearance aspects, a group consultation meeting composed of oncology nursing experts and clinical psychology experts, using nine type personality as a tool for self-comprehension and development, to conduct research guidance and body image education, and to encourage patients to share their mood and think about the future. Aesthetic specialists explained the skin condition, health care, cosmetic techniques, and hair care and encouraged patients to practice the techniques. This intervention focuses on the patient’s spirit and appearance, improving the patient’s mood of depression and anxiety. Therefore, sexual function due to these emotions was also improved.
Under the application of the aforementioned sexual counseling and education models, there is a positive impact on the sexual quality of life (including sexual arousal, orgasm, dyspareunia, and vaginal lubrication) of patients with BC, while the effects on sexual desire, sexual interest, and sexual satisfaction are inconsistent. This may be related to different surgical methods. Mastectomy is prone to alter the patient’s body image, making them feel as though they have lost a part of their feminine identity, leading to tension, anxiety, and feelings of helplessness, which can affect their partner’s sexual life. Chemotherapy is likely to induce menopausal symptoms in women, such as decreased libido and sexual difficulties. Endocrine therapy can lead to vaginal atrophy and dryness (30). Regardless of the treatment method, there is a certain degree of physical and psychological damage to the patient, causing resistance to sexual intercourse and leading to marital discord. It is possible that these educational models cannot eliminate the fear and resistance that arise during sexual intercourse. Additionally, the focus of sexual counseling and education models varies, and the types of patients facing education differ (including age, level of sexual education knowledge, openness to sexuality, confidence, self-esteem and other factors). Therefore, in the analysis of results, patients’ sexual desire, sexual interest and sexual satisfaction cannot fully return to pre-treatment levels when undergoing various sexual counseling and education models, as they do not completely accept sexual intercourse, nor do they generate sexual desire and interest as before.
These methods of sexual counseling and psychological education discussed in this study provide inspiration for clinical practice. Nurses should pay more attention to the dynamic psychological process of female patients. Due to the change of appearance, women would think that they lose their female identity, their body image is damaged, and they lack sexual attraction. We should affect their self-esteem about sex. Nurses should give patients the anatomy and physiological structure of their genitals, encourage patients to express emotions, establish a good sexual self-concept, and correct sexual misconceptions. Appropriate education should be given to patients with BC after discharge to improve sexual life treatment. In addition, the reaction of their sexual partners to the patients after treatment should also be considered, and the family members should receive common science education to enable the patients to obtain family support (31, 32).
5.1. Conclusions
A total of eight studies involving 814 female patients were included in this meta-analysis. The impact of sexual nursing consultation and education mode on the quality of sexual life of BC patients (including patients undergoing mastectomy, chemotherapy and radiotherapy, and hormone therapy) was comprehensively evaluated, and the positive significance of improvement was concluded.
According to the above results and discussion, sexual problems have been deeply rooted among patients with BC. Researchers, society, medical staff, patients and their families often escape from this problem due to emotional factors such as shame, and etc. If this issue remains unresolved, BC patients may experience a range of post-treatment challenges, including decreased sexual satisfaction and marital discord, which can ultimately contribute to reduced satisfaction with sexual function.
Research showed that the application of sexual nursing consultation and education mode can alleviate the above phenomenon. It also warns medical staff and hospital leaders from the side to pay attention to psychological nursing and policy support for sexual problems of patients with BC before and after treatment; researchers should explore how to alleviate or improve the obstacles of solving sexual problems of BC patients, and the society should also publicize the knowledge content of BC treatment to improve the harsh environment of BC patients due to stereotypes before and after treatment.
5.2. Strengths and Limitations
In the context of the times, doctors, nurses and patients themselves have neglected to pay attention to sexual life after sexual operation (33). After receiving cancer treatment, women’s body image disorder or other pain will cause psychological problems, which will affect their sexual function (34). In the past three years, few articles have been published to study the impact of postoperative sexual function of cancer patients. The latest research direction is the meta-analysis of exercise intervention on the quality of life of patients with BC. Our research points are different from them (35). This meta-analysis studied the impact of sexual counseling and psychological education on the quality of sexual life of patients with cancer after treatment. In addition, it summarizes various forms of counseling models, which affect the sexual function of patients with cancer after treatment through psychological counseling, question-and-answer, sexual psychoeducation, sexual practice, establishment of sexual self-concept, change of self-image, and systematically analyzes the above intervention methods.
The main limitations of this study include insufficient and mismatched data across studies, as well as inconsistent outcome measures. Additionally, the limited number of available articles on post-treatment sexual function in BC patients resulted in a relatively small sample size. Moreover, the diversity of intervention types was minimal, which further constrained the scope of the analysis.
The above limitations of this study may result in some impact on the outcome analysis. The limited diversity in disease types and interventions, along with an insufficient sample size, contributed to the lack of comprehensiveness in this study’s analysis. Furthermore, the small number of relevant articles resulted in inadequate subgroup formation, making corresponding data analysis challenging.
5.3. Future Research
Recommendations for future research in this area are as follows:
The scope of study designs should be expanded to include retrospective studies, case-control studies, uncontrolled before-and-after studies, and double-arm clinical trials. Future studies should aim to increase sample sizes by extracting and analyzing data from a broader range of studies to enhance the statistical power and supplement the findings of this study. Additional influencing factors — such as the role of sexual partners, patients’ self-perception, changes in physical appearance, and psychological changes — should be taken into consideration, as they may significantly affect sexual function in BC patients. Expanding in these directions will help make future research more comprehensive, rigorous, and clinically meaningful.