1. Context
Breast cancer (BC) is the most prevalent type of cancer and the cause of most BC-related deaths among women (1). According to the Global Cancer Observatory (GCO) in 2022, BC will be the most prevalent cancer among total new cancers (2). In Iran, new cases of BC are reportedly 11.35% among various types of cancer. Moreover, this cancer comprises 25.5% of total cancers among the Iranian female population and accounts for the first rank (3).
Cancer diagnosis is often a profoundly distressing experience (4), as cancer is commonly associated with death and incurability in many cultures, leading to significant uncertainty about the future (5). Death anxiety (DA) is a common psychological reaction experienced by most patients with cancer, including BC-affected women (6). Death is an inevitable aspect of human life; however, it often evokes fear due to its ambiguous and uncontrollable nature (7). The DA is a complicated and multifaceted concept that can be defined as a fundamental fear and unpleasant feeling toward one’s or others’ death. Templar believes that DA is manifested with the death of a person or one of the relatives, or when a person dies suddenly (8). Although a certain level of DA is considered necessary to engage with and find meaning in life (9), its intensity tends to increase in the context of life-threatening illnesses such as cancer (10). Most patients with advanced cancers are held at a crossroads between enjoying life and being aware of their imminent death (11), leading to psychological disorders such as anxiety, depression, and reduced quality of life. This anxiety adds to patients’ distress and acts as a barrier to end-of-life care provision (12, 13). On the other hand, the principles of palliative care emphasize quality death (14, 15). Therefore, anxiety relief is an important strategy in the management of these patients.
A study on DA in patients with cancer revealed that they experienced a moderate level of DA; however, women with BC showed more significant levels of DA than those with other cancers. In other words, the results indicated that gender and cancer type were associated with the DA level as a common psychological reaction in many BC women (4, 16). In an Iranian study, DA was experienced in about 80% of patients with BC (17). Another study indicated that the female gender was a negative predictor for DA (5). In Palestine, an investigation disclosed that moderate and high DA were experienced by half of women with cancer (18), and various factors could be effective in aggravating their DA, including BC women’s post-diagnosis awareness followed by treatment consequences, such as pain and physical symptom, and even after treatment completion due to fear of disease recurrence and progress and fear of the future (19).
Systematic review studies on DA were conducted for all types of cancer, and no specific study is available for estimating DA in BC. As a negative emotional reaction to death, DA can harm the psychological health of women with BC and result in psychological disorders, thereby reducing their quality of life. Therefore, the first step in managing DA is to identify the status of this phenomenon in patients with BC to be controlled through psychological measures and effective strategies.
2. Objectives
Given the high prevalence of BC and the fact that its estimation is absent in this population, the aim of the current study was to estimate DA in BC patients through a systematic review and meta-analysis approach.
3. Methods
The present study conducted a systematic review of the existing research literature on the mean of DA in patients with BC by following the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (20). This study was based on the population, intervention, comparison, outcomes (PICO) framework: Studies on BC, irrespective of disease stage, time since diagnosis or treatment modality (P); studies without intervention or control groups (I, C); studies reporting the DA BC (O).
This study was previously registered in PROSPERO (CRD4224556558). Also, ethics approval was obtained from The Research Ethics Committee of Shahid Beheshti School of Nursing and Pharmacy with the code IR.SBMU.PHARMACY.REC.1403.116.
3.1. Search Strategy
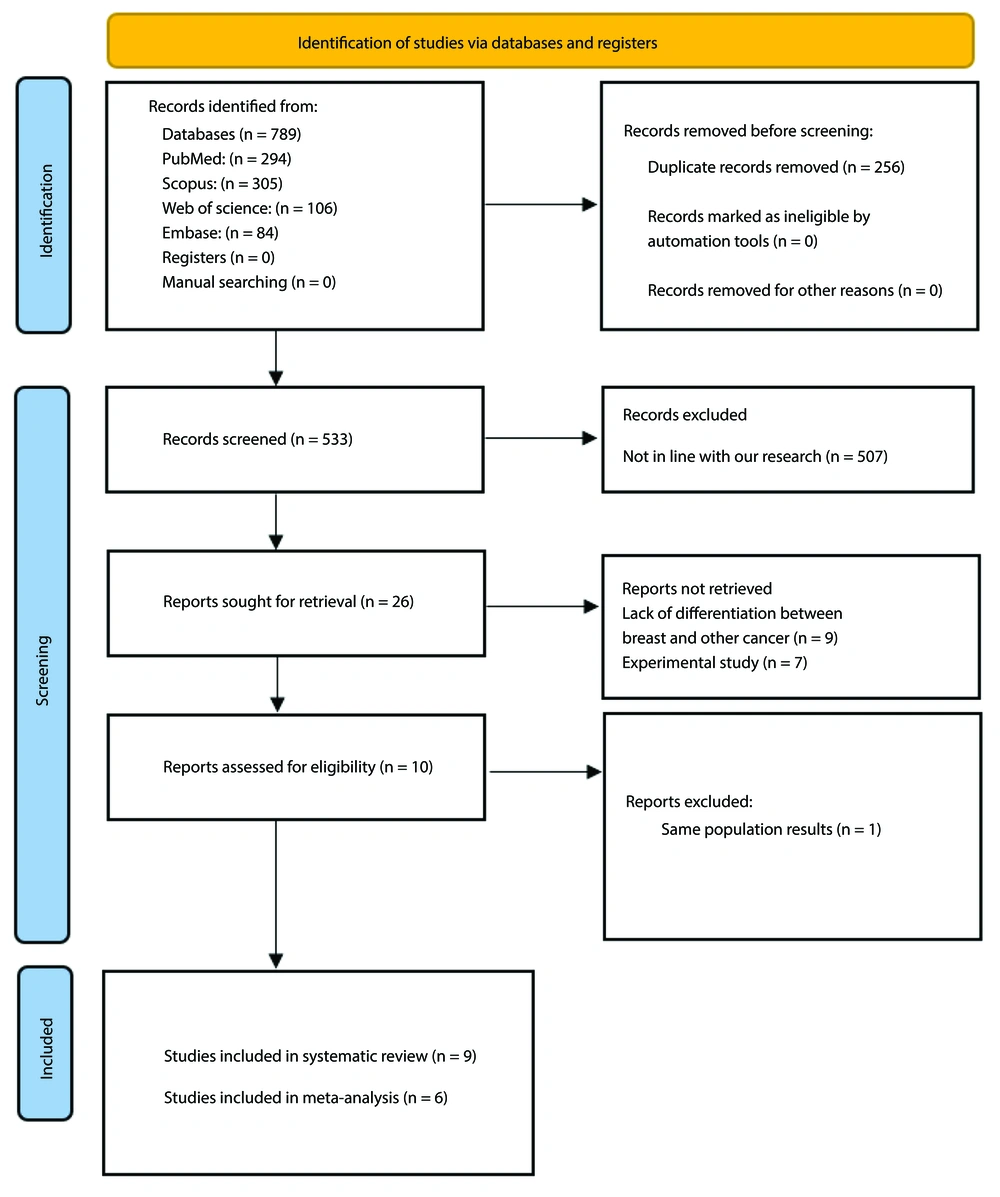
An extensive search was conducted in the English electronic databases, including PubMed, Web of Science (WOS), Scopus, and Embase. In the literature search, keywords obtained from Medical Subject Headings (MeSH) such as "Breast Cancer" and "Death Anxiety" were used along with their combinations using Boolean operators "AND" and "OR". The details of the search strategy are presented in Table 1. The search was performed from inception to December 31, 2024. To avoid missing relevant articles, the lists of references and citations of the included studies were manually searched. All the search steps were performed with the participation of two researchers independently (N.D. and M.K.). A PRISMA Flow diagram of the study selection process was provided in Figure 1 (20).
| Databases | Keywords | Results |
|---|---|---|
| PubMed | (["breast neoplasms"(MeSH Terms) OR "Breast cancer"(Title/Abstract) OR "breast neoplasm*"(Title/Abstract) OR "breast malignanc*"(Title/Abstract) OR "breast tumor*"(Title/Abstract)] AND ["Attitude to Death"(MeSH Terms) OR "Death Anxiety"(Title/Abstract) OR "fear of death"(Title/Abstract) OR "Attitude to Death"(Title/Abstract)] OR "death depression"(Title/Abstract) OR "dying anxiety"(Title/Abstract) | 294 |
| Scopus | [TITLE-ABS-KEY (“breast neoplasm*”) OR TITLE-ABS-KEY (“Breast cancer”) OR TITLE-ABS-KEY (“breast malignanc*”) OR TITLE-ABS-KEY (“breast tumor*”) AND TITLE-ABS-KEY (“Death Anxiety”) OR TITLE-ABS-KEY (“fear of death”) OR TITLE-ABS-KEY (“Attitude to Death”) OR TITLE-ABS-KEY (“Attitude to Death”) OR TITLE-ABS-KEY (“death depression”) OR TITLE-ABS-KEY (“dying anxiety”)] | 305 |
| WOS | TS = ("breast neoplasm*") OR TS = ("breast cancer") OR TS = ("breast malignanc*") OR TS = ('breast tumor*') AND TS = ("death anxiety") OR TS = ("fear of death") OR TS = ("Attitude to Death") OR TS = ("death depression") OR TS = ("dying anxiety") | 106 |
| Embase | [(“breast neoplasm*”: ab, ti OR “breast cancer”: ab, ti OR “breast malignanc*”: ab, ti OR “breast tumor*”: ab, ti) AND “death anxiety”: ab, ti OR “fear of death”: ab, ti OR “attitude to death”: ab, ti OR “death depression”: ab, ti OR “dying anxiety”: ab, ti] | 84 |
Abbreviations: MeSH, medical subject headings; WOS, Web of Science.
a The number of * symbol indicates the number of points assigned to a given parameter.
3.2. Inclusion and Exclusion Criteria
The cross-sectional, case-control, cohort, and English language studies reporting the mean of DA in BC patients were included in this systematic review and meta-analysis. Case reports, case series, experimental, qualitative, Letters to the editor and review designs due to the lack of use of primary data were not included. To retrieve grey literature, conference papers and websites related to theses and dissertations were reviewed, and no relevant studies were extracted.
3.3. Study Selection
This systematic review and meta-analysis was conducted using EndNote X8, a data management application. Two separate researchers carried out the evaluation of the title, abstract, and full text, in addition to eliminating duplicate articles, in order to select the included studies based on the inclusion and exclusion criteria. The third evaluator's decisive opinion was used to mediate conflicts between the opinions of the two researchers.
3.4. Data Extraction
The data extracted from the included studies consisted of the first author's name, publication year, location of study, study design, sample size, age, marital status, and mean ± SD of DA and key results. This section was done with the participation and agreement of two investigators.
3.5. Quality Assessment
The Newcastle–Ottawa Scale (NOS) serves as the basis for quality assessment of the current studies in this systematic review. One of the most well-known measures for evaluating the risk of bias in observational studies is the NOS. This scale evaluates articles according to four criteria: Comparability (a section that reviews confounders and other influencing factors), sample size (non-respondents and measurement tool), representativeness of the samples, and results (from two aspects: Assessment of the outcome and statistical test). With the exception of the comparability parameter, which can receive up to two points, each item on the scale is scored from one point. As a result, the highest score for every study is nine, and research with a score of less than five is considered to be at high risk of bias (21). Two investigators assessed each study's quality independently. In case of a discrepancy, the opinion of a third assessor was sought. The specifics of the scoring were displayed in Table 2.
| Author (Y) | Selection | Comparability | Outcome | Star (0 - 9) | ||||
|---|---|---|---|---|---|---|---|---|
| Representativeness of the Cases | Sample Size | Non-response Rate | Ascertainment of the Screening/Surveillance Tool | The Potential Confounders Were Investigated by Subgroup Analysis or Multivariable Analysis | Assessment of the Outcome | Statistical Test | ||
| Kiyak and Turkben Polat (2022), (22) | 1 (*) | 0 | 0 | 2 (*) | 0 | 1 (*) | 1 (*) | 5 |
| Yousefi Afrashteh and Masoumi (2021), (23) | 1 (*) | 0 | 0 | 2 (*) | 0 | 1 (*) | 1 (*) | 5 |
| Salmanian and Marashian (2021), (10) | 1 (*) | 0 | 0 | 2 (*) | 1 (*) | 0 | 1 (*) | 5 |
| Mahdavi et al. (2019), (6) | 1 (*) | 0 | 0 | 2 (*) | 1 (*) | 0 | 1 (*) | 5 |
| Karampour et al. (2017), (24) | 1 (*) | 0 | 0 | 2 (*) | 0 | 0 | 1 (*) | 4 |
| Ahmead et al. (2024), (18) | 1 (*) | 0 | 0 | 2 (*) | 1 (*) | 1 (*) | 1 (*) | 6 |
| Bibi and Khalid (2020), (25) | 1 (*) | 0 | 0 | 2 (*) | 1 (*) | 1 (*) | 1 (*) | 6 |
| Su et al. (2022), (19) | 1 (*) | 0 | 0 | 2 (*) | 1 (*) | 1 (*) | 1 (*) | 7 |
| Yang et al. (2024), (26) | 0 | 1 (*) | 1 (*) | 2 (*) | 1 (*) | 1 (*) | 1 (*) | 7 |
3.6. Death Anxiety Scale
Donald Templer developed the Death Anxiety Scale (DAS) in 1970. This scale consists of 15 true/false items ranging from 0 to 15, with six questions having reversible scores. A higher score indicates a higher level of DA, with scores of 8 or higher indicating a high level of DA. The DAS includes four dimensions: Fear of dying, anxiety over pre-death achievements, fear of caregiver forgetfulness, and anxiety over post-death occurrences (27). According to internal consistency and test-retest results, the scale's Cronbach's alpha was between 0.89 and 0.91 (28).
3.7. Statistical Analysis
Data analysis was conducted using STATA software version 11. I2 and Cochrane Q tests were utilized to compute the Heterogeneity Index among the studies. Furthermore, in the Cochrane Q test, a P-value less than 0.01 was considered significant. The forest plots estimated the mean of DA using the random effects model (REM) and a 95% confidence interval (CI). Sensitivity analysis was employed to assess the effect of removing each study on the overall mean of DA (29, 30). Using a funnel plot analysis and the Egger and Begg tests, publication bias was evaluated (31).
4. Results
4.1. Study Selection
A total of 789 studies were identified during the thorough search of electronic databases as shown in Figure 1. After excluding 256 duplicates and 507 studies that were not aligned with the goals of the current study, 26 articles remained. At the end of the subsequent phase. Of these, 17 articles were excluded based on specific criteria: Nine studies due to the lack of differences in cancer type, seven due to differences in the type of study design, and 1 because of overlapping population data. As a result, 9 studies were deemed eligible for inclusion in the systematic review. However, only 6 of these met the criteria for inclusion in the meta-analysis.
4.2. Study Characteristics
The 9 eligible studies included four from Iran, two from China, and one each from Pakistan, Turkey and Palestine. All studies were cross-sectional and were all published between 2017 and 2024. Nine studies, with a total of 1776 patients with BC, were conducted with sample sizes ranging from 80 to 514. T-DAS tool was the most frequently (7 studies). The two studies used different measures. Among the seven studies, one study used a different scoring method. Finally, only the 6 studies using true/false scoring on T-DAS were entered into the meta-analysis (Table 3).
| Author’s Name | Year | Location | Study Design | Sample Size | Age (y) | Marital Status (Married) | Measure | Key Results |
|---|---|---|---|---|---|---|---|---|
| Karampour et al. (24) | 2017 | Iran | Cross-sectional study | 118 | 46.75 ± 10.45 | 60.2% | T-DAS | 66.9% of BC patients had DA and the mean ± SD of DA was 9.68 ± 3.67. 75.4% of the participants were afraid of having an operation. 72% of the women had the fear of death. The mean of DA was significantly higher in married participants (P = 0.007). The statistical test showed there were no significant associations between age, economic status, employment status, place of residence and type of hospital with DA. |
| Mahdavi et al. (6) | 2019 | Iran | Cross-sectional study | 100 | Mean: 49.06 | 69.0% | T-DAS | The mean ± SD of DA was 10.67 ± 0.65. There was a significant relationship between DA and mental (β = -0.329, P = 0.006), existential (β = -0.273, P = 0.004), and religious (β = -0.536, P < 0.001) well-being. |
| Yousefi Afrashteh and Masoumi (23) | 2021 | Iran | Cross-sectional study | 210 | 18 - 30 (22.9%); 31 - 40 (32.9%); 41 - 50 (26.2%); 51 - 65 (18.1%) | 53.3% | T-DAS | The mean ± SD of DA was 14.3 ± 1.1. There was a significant positive correlation between DA with depression (R = 0.77, P < 0.01) and DA with anxiety (R = 0.85, P < 0.01). But, the correlation between DA and self-compassion was significant negative (R = -0.46, P < 0.01). DA was not significantly different in the three age groups including 18 - 33, 34 - 49 and 50 - 65 years (P = 0.79). There was a significant indirect path of depression on DA (β = 0.065, P < 0.03) and anxiety on DA (β = 0.089, P < 0.04) via self-compassion. |
| Salmanian and Marashian (10) | 2021 | Iran | Cross-sectional study | 200 | 30 - 35 (19.0%); 35 - 40 (33.5%); 40 - 45 (29.5%); 45 - 50 (21.0%) | 84.5% | T-DAS | The mean ± SD of DA was 9.25 ± 2.28. There was a significant association between DA and emotion-focused strategy (β = -0.26, P = 0.001) and DA and disease perception (β = 0.39, P = 0.001). |
| Kiyak and Polat (22) | 2022 | Turkey | Cross-sectional study | 140 | Median: 51 y (range: 28 - 77) | 87.1% | T-DAS | The mean ± SD of DA was 8.86 ± 2.83. There was a significant positive correlation between DA with fear of COVID-19 (R = 0.383, P < 0.01) and DA with Coronavirus Anxiety Scale (R = 0.271, P < 0.01). |
| Ahmead et al. (18) | 2024 | Palestine | Cross-sectional study | 214 | 18 - 30 (10%); 31 - 40 (36%); 41 - 50 (25%); ≥ 51 (29%) | 69.7% | T-DAS | The mean ± SD of DA was 7.0 ± 1.6. There was a significant negative correlation between DA with self-distraction (R = -0.255, P < 0.000), active coping (R = -0.200, P < 0.003), use of instrumental support (R = -0.169, P < 0.014), use of emotional support (R = -0.162, P < 0.018), humor (R = -0.293, P < 0.000), and acceptance (R = -0.147, P < 0.033). |
| Bibi and Khalid (25) | 2020 | Pakistan | Cross-sectional study | 80 | 20 - 30 (13.8%); 31 - 40 (20.0%); 41 - 50 (35.0%); ≥ 51 (31.3%) | 71.3% | DAS Goreja and Pervez | The mean ± SD of DA was 51.16 ± 15.21. There was a significant negative correlation between DA with social support (R = 0.38, P < .001). |
| Su et al. (19) | 2022 | China | Cross-sectional study | 200 | 50 ± 10 | 91.0% | Death and Dying Anxiety Scale (DADDS) | The mean ± SD of DA was 20.6 ± 17.5. There was a significant positive correlation between DA with depression (R = 0.57, P < 0.001), anxiety (R = 0.60, P < 0.001) and symptom burden (R = 0.43, P < 0.001). |
| Yang et al, (26) | 2024 | China | Cross-sectional study | 514 | 46.69 ± 9.94 | No report | T-DAS | The mean ± SD of DA was 3.07 ± 0.62. There was a significant positive correlation between DA with self-esteem, social support, and subjective well-being (P <0.05). |
Abbreviations: BC, breast cancer; DA, death anxiety; DAS, Death Anxiety Scale.
4.3. Mean of Death Anxiety in Breast Cancer Patients
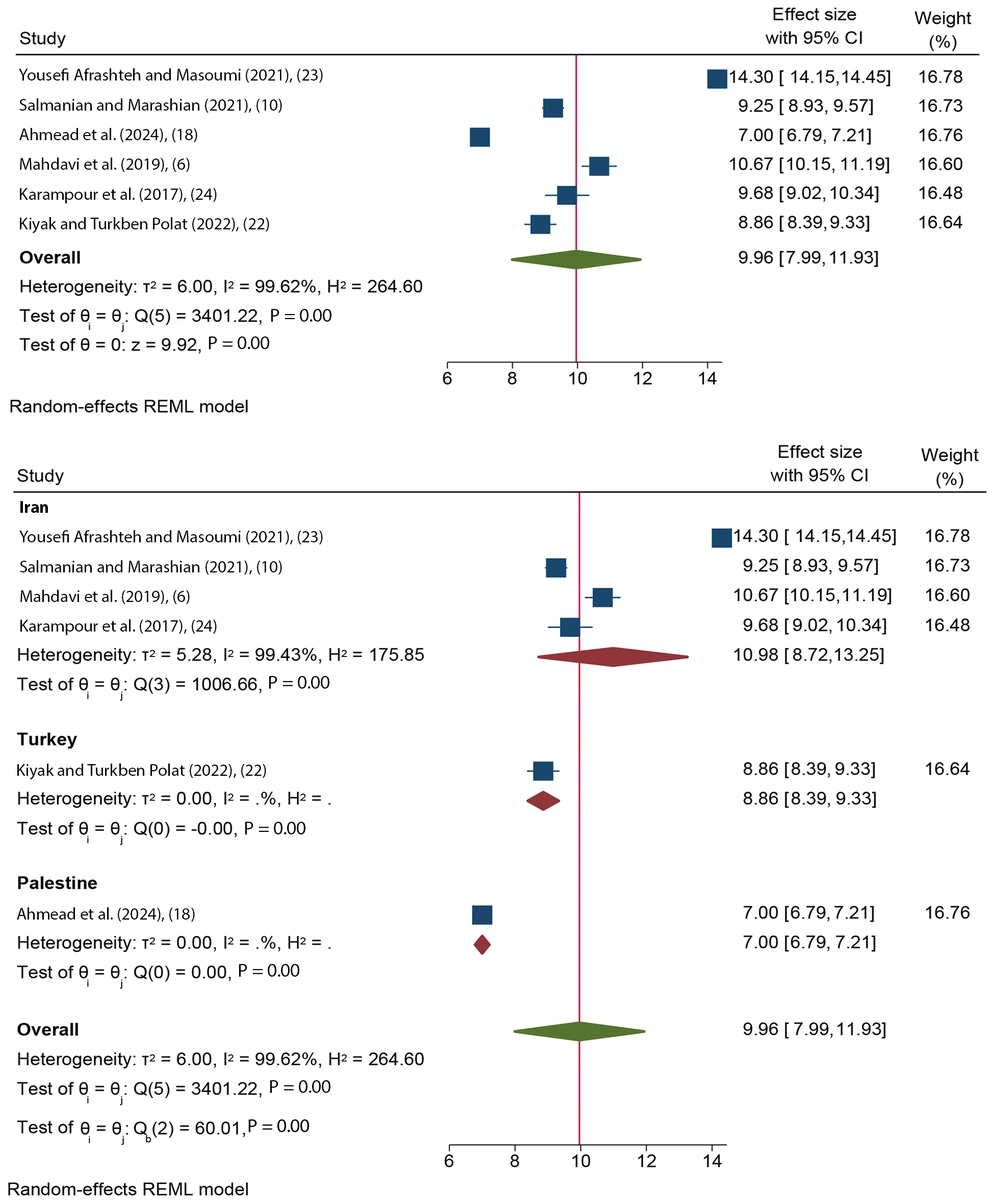
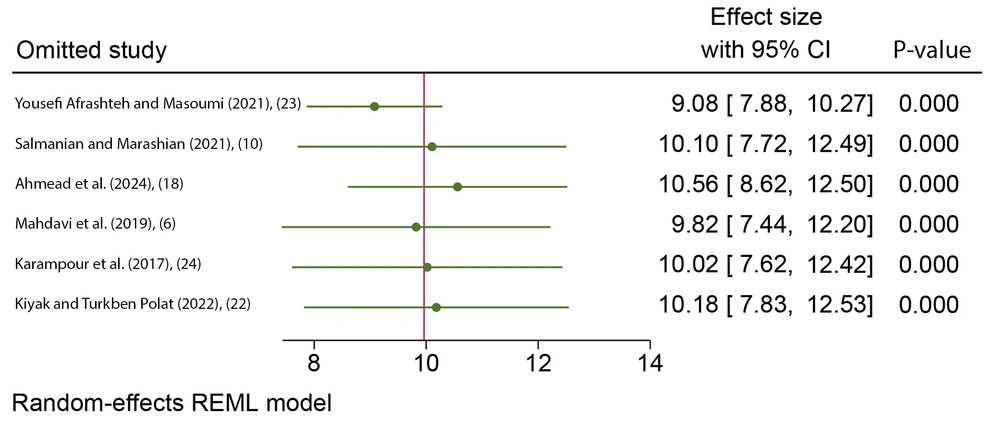
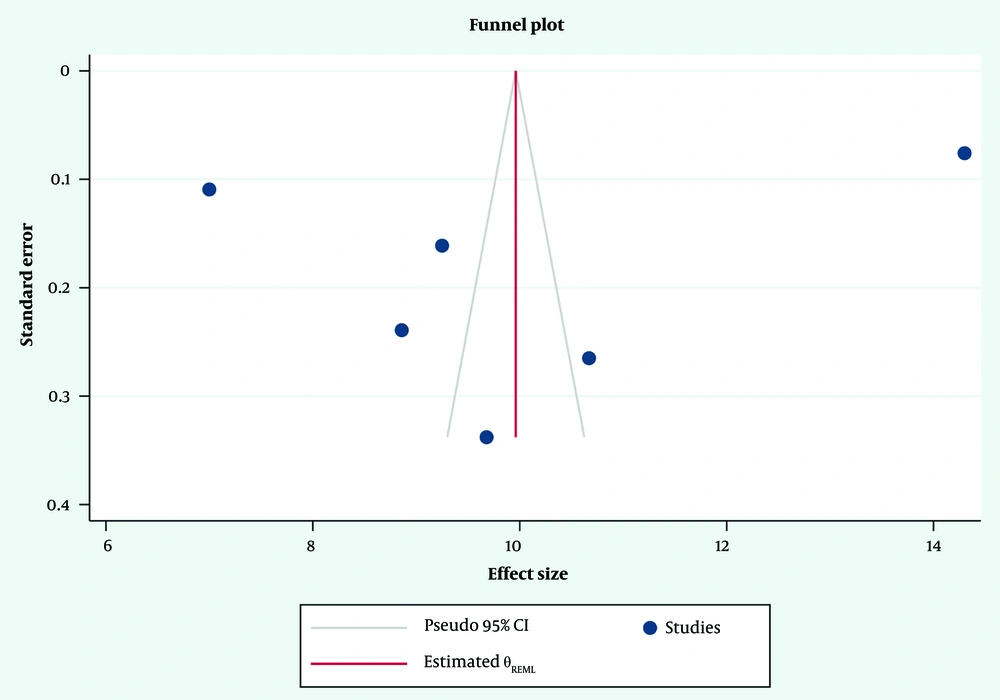
Figure 2 displays the pooled mean of DA in patients with BC, which was 9.96 (CI: 7.99 - 11.93, I2 = 99.69, P < 0.001). As presented in Figure 3, the results of sensitivity analysis revealed that the highest impact was related to the Yousefi Afarashteh and Masoumi study (23), so, its removal has reduced the amount of pooled mean of DA. As seen in Figure 4, the asymmetrical funnel plot for the mean of DA indicates the presence of publication bias. However, the results of the Egger (Z = -0.47, P = 0.64) and Begg's regression test (Z = 0.38, P > 0.71) do not corroborate this data.
5. Discussion
The present study was conducted to estimate the mean DA in BC patients with a systematic review approach. The results showed that the DA level was greater than the moderate level in cancer patients. Similarly, Soleimani et al. reported that cancer patients experienced a moderate level of DA. However, this phenomenon could be influenced by various factors, one of which was the type of cancer, with a greater DA in BC than in other cancers (16). In 2024, another study on DA-related factors among a cancer population revealed a positive association of the female gender with DA. Breast cancer is a terrible event in the lives of numerous women (32). Patients with BC demonstrate negative signs such as anger, anxiety, and frustration. After mastectomy and other treatments, women experience changes in their mental image, reduced self-confidence, and psychosocial stresses. Most BC women have dependent and minor children, which increases their parental concern. They experience a series of challenges, including an impairment in their role as parents and fear for their children’s future after death (33-36).
High heterogeneity was observed in this systematic study, primarily because it was conducted during the COVID-19 pandemic (37). In this study, stressful conditions during the COVID-19 pandemic and life-threatening diseases (e.g. cancer) intensified patients’ anxiety levels. The patients experienced high anxiety due to uncertainty about the future. According to a systematic study on this topic, existential anxiety was experienced by chronic patients, such as those suffering from cancer and cardiovascular disease, during the COVID-19 pandemic, which increased their anxiety (38, 39). Two studies that were conducted during the Covid-19 pandemic also showed that BC patients experience high DA (22, 23).
The meta-analysis results indicated a greater mean of DA in Iranians with BC than in those of Palestine and Turkey. The attitude toward death can be influenced by cultural and religious differences. Discrepant results were reported by studies that examined the relationship between religious beliefs and DA (5, 40-42). A weak association between DA and religion was found in a review study in 2021 (43). In 2024, a systematic study among cancer patients revealed a negative connection between DA and religious beliefs (32). A negative link between DA and religious/spiritual beliefs was observed in another systematic in 2024 (44). The Iranian society is mostly religious, and based on the death management theory, religious beliefs can enhance afterlife immortality. However, other factors seem to cause stress and intensify DA in Iranian patients. A study in 2024 has evidenced that economic factors are a positive predictor for the distress of Iranians with cancer (5). Iran has undergone economic sanctions in recent years, and patients have been exposed to such challenges as a chemotherapy drug shortage. These challenges in the Health System of Iran can exacerbate psychological concerns among Iranians with cancer, which can cause fear of an ambiguous future and aggravate their DA cancer (45).
Death anxiety is an unavoidable event among cancer patients. Based on the higher mean level of DA among women with BC, our results highlight the need for the attention of healthcare providers to the psychological concerns of BC women. Healthcare providers can offer supportive measures to improve patients’ ability to cope with these cancer-related negative complications.
5.1. Limitations
This study had several limitations, and its results should be interpreted with caution. We did not have access to some databases, and some studies were not included in the analysis due to different tools. Since only English studies were analyzed, studies in other languages were an obstacle in the analysis, and the lack of necessary findings in some cases caused the exclusion of related studies.
5.2. Conclusions
This study increased our knowledge of the mean of DA in the BS population. Women with BS experience more DA and a decrease in their quality of life compared to other cancers. Therefore, future studies should focus on developing intervention strategies that are key in reducing the DA of BC patients. Healthcare workers in psycho-oncology care should conduct counseling sessions and education workshops to enhance BS adaptability, improving quality of life, the ultimate goal of palliative care.