1. Background
Testicular cancer is the most common neoplasia among young males aged 15 to 40 years, accounting for 1 % of adolescent malignancies and 5 % of adolescent solid tumors, with incidence rate of 3 to 11 cases per 100,000 males each year. Previous studies have indicated that these malignancies accounted for 0.1% of cancer-related deaths in males (1, 2). Due to its curative nature and important effect on fertility, early diagnosis and treatment of testicular cancers is essential (3, 4). Advancements in chemotherapy and radiotherapy have led to cure rates exceeding 90% and five-year survival rates greater than 95% for patients diagnosed at an early stage (5). In Iran, the incidence rate is about 1.3 cases per 100,000 males (6).
Germ cell tumors (GCTs) represent about 95% of testicular malignancies and are categorized into two subgroups: Seminoma and non-seminoma (7). The majority of these patients are diagnosed at the first clinical stage of neoplasia (8). Metachronous contralateral involvement may occur in certain male patients. Previous studies have reported an incidence ranging from 1.9% to 8.7% (9-11). Treatment usually consists of orchidectomy, resulting in permanent infertility and lifelong testosterone dependency (12). Due to improvement in management of testicular malignancies and increased survival rate, incidence of contralateral involvement has risen in the last decade (11).
European Association of Urology’s (EAU) guidelines emphasize performing a biopsy on the contralateral testis in cases of GCT when the contralateral testis is smaller than 12mm, in patients younger than 40 years old with a history of cryptorchidism or weak spermatogenesis (13). Some European centers perform routine contralateral biopsies for early diagnosis and radiotherapy to enhance hormonal secretion and prevent orchidectomy (14). However, significant concerns exist regarding routine contralateral testis biopsy. Many urologists in the United States oppose this procedure, due to the heightened risk of recurrence following radiotherapy (15).
2. Objectives
In this study, we aimed to investigate the incidence of metachronous contralateral testicular cancer in patient without any risk factor and under 40 years of age, to determine the necessity of routine biopsy for early diagnosis. Notably, existing studies have not stratified contralateral cancer risk in strictly low-risk populations (no cryptorchidism, family history, or testicular atrophy). Our study fills this gap by focusing exclusively on this subgroup.
3. Methods
This historical cohort study was registered and by the ethic committee of Shahid Beheshti University of Medical Sciences. All male patients younger than 40 years old who were diagnosed with testicular cancer and referred to Shahid Modarres Hospital in Tehran, Iran, up to March 2019, with a primary pathology of GCT, were enrolled in the study. Exclusion criteria included poor cooperation in follow-up, death in course of follow up, a history of cryptorchidism, testicular atrophy, a history of congenital or acquired immunocompromising conditions, a history of pelvic or testicular radiotherapy (for the treatment of primary neoplasia), and personal or familial histories of malignancies, as well as non-GCT pathologies. The year 2019 was selected to ensure a minimum of five years of follow-up. Additionally, an initial diagnosis at Shahid Modarres Hospital was not required; referral to this center for treatment sessions, such as chemotherapy, was sufficient for inclusion in our study.
Sampling included all patients presented to Shahid Modarres Hospital and was conducted using a census method. The sample volume was calculated using G-Power software (version 3.1.9.3) as total of 220 patients based on an effect size of 0.35, a two-sided Type I error (α) of 0.05, and a power (1-β) of 0.95. All patients' ages at diagnosis, sides of primary neoplasia, primary pathologies, and stages were recorded after entering the study. The patient's condition was assessed via phone call during follow-up period, and if there were suspicions of contralateral neoplasia, patients were invited for additional investigations such as physical examinations and ultrasound studies. In cases of metachronous contralateral testicular neoplasia, pathology and the mean interval time between the first and contralateral diagnosis were recorded.
Frequencies, means, and standard deviation (SD) were used to characterize the variables. In the case of a non-normal distribution, the median and interquartile ranges (IQR) were utilized. The SPSS (Version 26.0 for Windows; SPSS Inc., Chicago, IL) was used for all analyses. A post-hoc power analysis using G*Power 3.1 indicated 80% power to detect a 1.5% incidence rate (α = 0.05, two-tailed).
4. Results
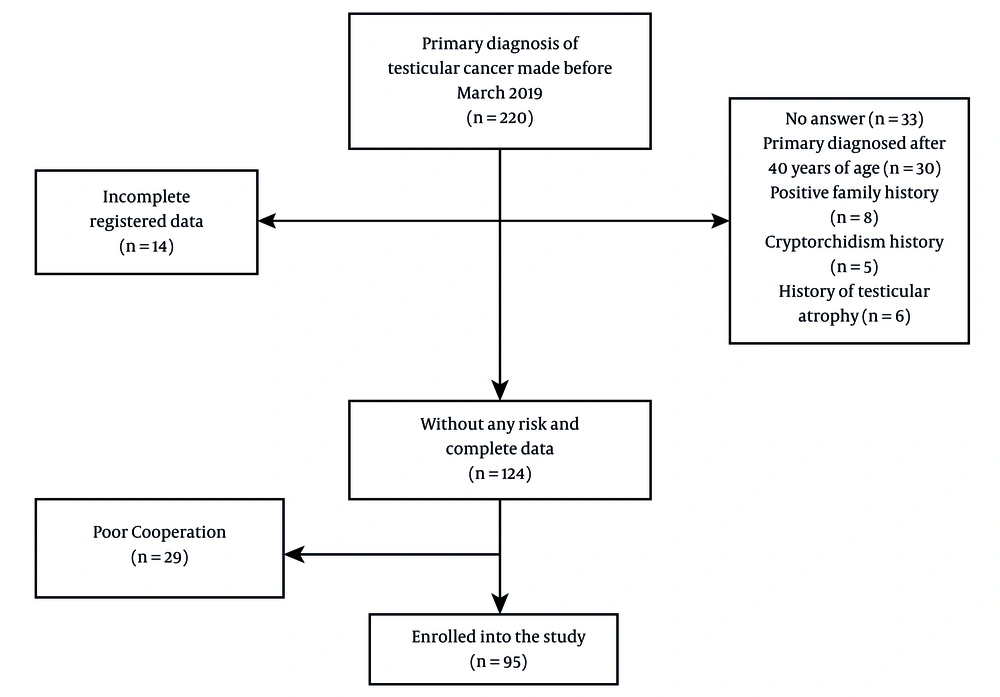
A total of 220 patients with a primary diagnosis of unilateral testicular cancer made before March 2019 were identified. Archived data were evaluated, and 206 patients had properly recorded information sufficient for enrollment in the study. After making phone calls for data completion, 33 patients did not respond, 30 patients were primarily diagnosed after the age of 40, 8 patients had a family history of testicular cancer in first-degree relatives, 5 patients had a previous history of cryptorchidism, and 6 patients reported a history of testicular atrophy and were excluded from the study. From the remaining 124 patients, 29 did not cooperate for proper follow-up and were excluded. Ultimately, 95 patients remained in the study (Figure 1).
Whether the biopsy was performed in our center or not, the primary pathologic type of malignancy in all patients was GCT, with a mean age of diagnosis of 30.5 ± 5.44 years. In 48 (50.52%) patients, the pathology was seminoma (non-seminoma in 47 patients). The tumor was right-sided in 54 (56.84%) patients, while the remaining tumors were left-sided. A total of 62 (65.26%) patients were primarily diagnosed at T1 stage, 24 (25.26%) patients at T2, and the remaining 9 patients were diagnosed at T3 stage of testicular neoplasia. None of the patients were primarily diagnosed with tumor stage T4 (Table 1).
From all participants, one (1.05%) patient was diagnosed with metachronous contralateral testicular cancer through a biopsy conducted at another center. The revealed pathology was seminoma, and the diagnosis was established with an interval of 5 years and 6 months from the primary diagnosis.
The primary aim of the study was to collect additional data, such as tumor marker plasma levels and details of chemotherapy and radiotherapy sessions. Due to incomplete data from some participants who were commonly referred from other centers for surgical treatments like retroperitoneal lymph node dissection (RPLND), we decided not to record the above data to minimize the number of excluded participants.
5. Discussion
In 2020, testicular cancer was the most prevalent cancer among men aged 15 to 44 in 62 countries globally, with the highest incidence observed in European nations and the lowest in Asia and Africa (16). Testicular cancer is seeing a rising incidence but a declining mortality rate, and the growing incidence among younger populations is concerning, highlighting the need for early detection and preventive measures (17). In European countries, this cancer is recognized as the most prevalent malignancy among young adults aged 15 to 40 years (18). Several risk factors for testicular cancer are known, including cryptorchidism (19), Klinefelter syndrome (20), a positive family history (21), a history of impotence (22), and fetal exposure to estrogen hormone (23). One of the most significant risk factors is the history of contralateral testicular neoplasia (11). Several studies have been conducted to investigate synchronous and metachronous contralateral testis involvement.
In 1853, Bidard et al. reported bilateral testicular cancer for the first time (24). In 1942, Hamilton and Gilbert described the likelihood of bilateral involvement in cases of unilateral testicular cancer as being more than a thousandfold (25). Several studies conducted across various centers demonstrated the likelihood of this occurring in 1.9 - 3.9% cases (9, 26-28). Bilateral involvement can be synchronous or metachronous. The synchronous group is characterized by involvement occurring simultaneously or within the first three months following the primary diagnosis, while the metachronous group refers to involvement that occurs later.
In this study, we enrolled patients without any risk factors for testicular cancer, including cryptorchidism, family history of malignancy, history of testicular atrophy, and immunocompromising conditions and followed them via phone calls for at least 5 years. Among the 95 participants, only one case was diagnosed with metachronous contralateral testicular cancer, resulting in an incidence of 1.05%. Our study was limited due to smaller sample volume, incomplete collected data and poor cooperation in some cases.
A large study conducted by Fossa et al. involving 29,515 patients showed a 1.9% incidence of bilateral involvement after 15 years, with 62% classified as metachronous types (9). A systematic review of data from 50,376 patients revealed a 1.26% rate of metachronous contralateral involvement (0.56%) (29). Hellesnes et al. in 2020 in Norway identified 218 patients among 5,620 (3.87%) participants with contralateral involvement and also investigated the efficacy of cisplatin as a chemotherapy agent in decreasing the incidence of secondary involvement (25). Mrinakova et al. in 2021 reported that the incidence of bilateral testicular cancer was 4.5% among 2,124 patients, with 90.62% exhibiting metachronous involvement and a mean interval diagnosis time of 8.2 years that is mildly higher than 5.5 years resulted from our study (29).
One of the most controversial tools for the early diagnosis of contralateral testicular cancer is biopsy. In 1997, Herr and Sheinfeld did not approve biopsy of the contralateral testis due to the low incidence of tubular neoplasia (5% at that time) (30). Later in 2009, Heidenreich conducted a study with a similar design, introducing contralateral testicular biopsy as a controversial tool due to its potential to increase the risk of testicular neoplasia, particularly in patients with a testis volume less than 12ml, a history of cryptorchidism, or those older than 30 years of age (31). Pfail in 2024 stated that the incidence of in situ germ cell tumors in the contralateral testis is rare and typically contralateral. Due to this fact, along with the understanding that patients will be monitored in all circumstances and the current increased risk of testicular cancer in these patients due to Leydig cell dysfunction and impotency in 20% of them, prophylactic contralateral testicular biopsy remains controversial. They suggested estimating malignancy and identifying high-risk patients for performing the biopsy as a solution (32). Our findings challenge the necessity of routine contralateral biopsy in low-risk patients, aligning with AUA guidelines (15) but contrasting with EAU recommendations (13). This discrepancy highlights the need for risk-stratified guidelines.
5.1. Conclusions
Due to the low incidence of metachronous contralateral testicular cancer during the investigated period (1.05%), this study considers prophylactic biopsy a controversial tool and suggests conducting studies with larger sample sizes and developing appropriate guidelines for early diagnosis.