1. Introduction
Many pancreatic neoplasms and benign conditions could present as cystic leisions on imaging studies such as ultrasonography (US), computed tomography (CT) scan or magnetic resonance imaging (MRI). Pancreatic lymphangiomas were extremely infrequent and accounted for less than 1% of all lymphangiomas (1). The clinical manifestations of pancreatic lymphangioma were non-specific and depending on size of the cyst, patients might present with symptoms including abdominal pain, nausea, vomiting, and a palpable abdominal mass (2). Some of pancreatic cystic lesions included pseudo cyst, simple cyst, mucinous cyst neoplasms, serous cyst adenoma and intraductal papillary mucinous neoplasms, so conventional imaging examinations like abdominal US, CT scan or MRI could not distinguish these tumors; therefore, preoperative diagnosis has been very difficult. For large or symptomatic lymphangiomas, a total resection has carried out to prevent recurrence, infection, torsion and pressure effect (3). Neoplastic cystic tumors or pseudocysts of pancreas were more common than lymphangioma, so, differential diagnoses between these were very important. Pheochromocytoma was a very important differential diagnosis before any invasive procedure or surgery, because it might cause paroxysmal hypertension with dangerous complications such as intracranial hemorrhage and death. In addition of imaging studies such as US, CT scan or MRI, endoscopic ultrasonography (EUS) and fine needle aspiration (FNA) by this procedure for cytology evaluation or tumor marker assay could help us in more precise diagnosis.
2. Case Presentation
A 65-year-old woman has presented with epigastric pain radiating to the back since 5 months before her admission. There was a history of diabetes mellitus, hypertension and hyperlipidemia and patient had no history of past surgery, pancreatitis or trauma which made the diagnosis of pseudo cysts less likely. The patient has not also reported any history of weight loss, nausea, vomiting, jaundice, or alcoholism. On physical examination, vital signs were normal without fever, chills or rigor, abdomen was soft without tenderness, or distension and extremities’ pulses were symmetric. Laboratory investigations have revealed a leukocytosis (white blood cell: 22600), mild anemia (Hb: 10.2 mg/dL), and raised blood sugar (blood sugar: 272 mg/dL). Abdominal ultrasound examination has illustrated a heterogeneous mass with diameter of 59 × 76 between spleen and left kidney in LUQ. Abdomenopelvic computed tomography (CT) has shown a septated solid cystic 65 × 62 × 70 mass in the tail of pancreas, adjacent to left kidney. The mass has limited to lesser sac space and it has not invaded any contiguous organs, but it has displaced left kidney to downward. No calcification has revealed and the peri tumoral fat tissue has not obliterated. The differential diagnosis of CT scan report was suggestive of a mass with adrenal origin.
In order to investigate the origin of the mass, an adrenal gland MRI has performed.it has revealed a 60 × 58 heterogeneous and lobulated mass adjacent to left adrenal gland suggestive of a tumor originated from pancreas tail, left kidney or intestinal loop with the most probability of pancreas tail tumor (e.g. pancreatic serous cyst adenoma).
To ensure distinction between cystic lymphangioma and other pancreatic cystic lesions, diagnostic investigations such as guided EUS and CT scan FNA have performed. However, neither EUS nor cytology of FNA has guaranteed a thoroughly definite diagnosis.
24 hours urine VMA and metanephrine analysis were also normal (cr: 624 mg/day, VMA: 6.0 mg/24 hours, V: 1200 mL/24 hours, Metanephrine: 185.6 µg/24 hours, Normetanephrine: 624.4 µg/h.) to rule out pheochromocytoma. Furthermore, the CEA and CA 19-9 tumor marker were within the normal range less likely to make diagnosis of malignancy.
However, laparotomy has performed by a left subcostal approach. It has revealed an 8 × 8 cm solid cystic mass in distal pancreas. The mass had no adhesion to any adjacent organs and it has gradually detached from contiguous tissues. The mass has separated from adrenal gland and the gland was left intact and normal. Distal pancreas has displaced from beneath stomach. Then left gastroepiploic and short gastric arteries have ligated. Finally, the mass has resected with 5 cm margin.so distal pancreatectomy associated with splenectomy has done because splenic vessels were adhered to the lesion severely.
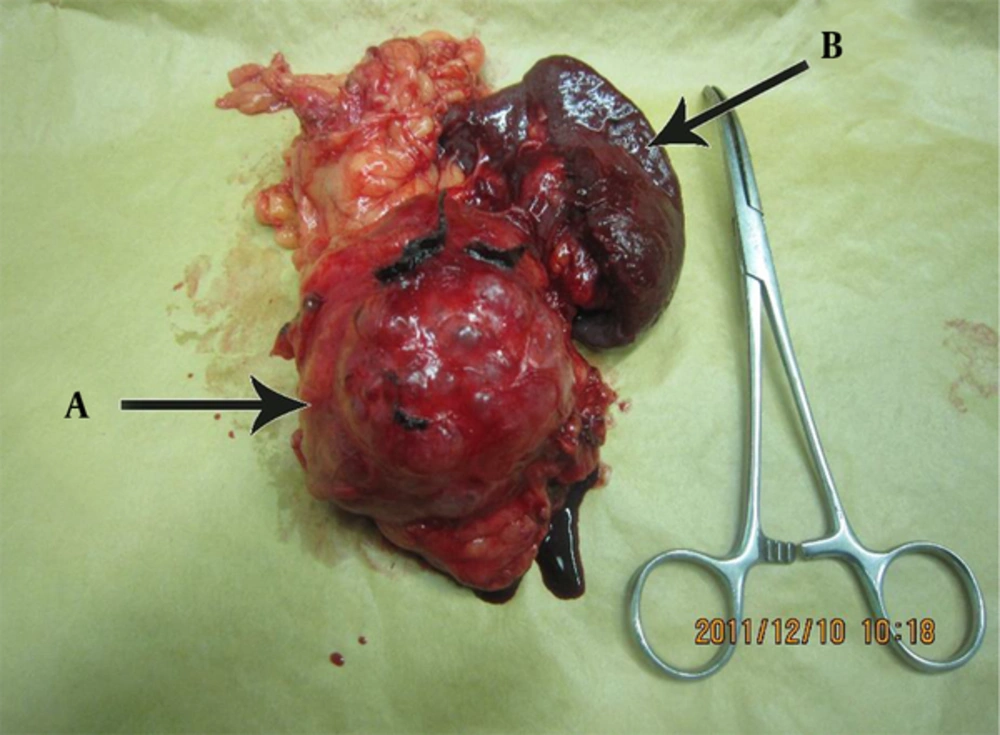
On gross examination, the tumor had a cystic and lobulated appearance (Figure 1).
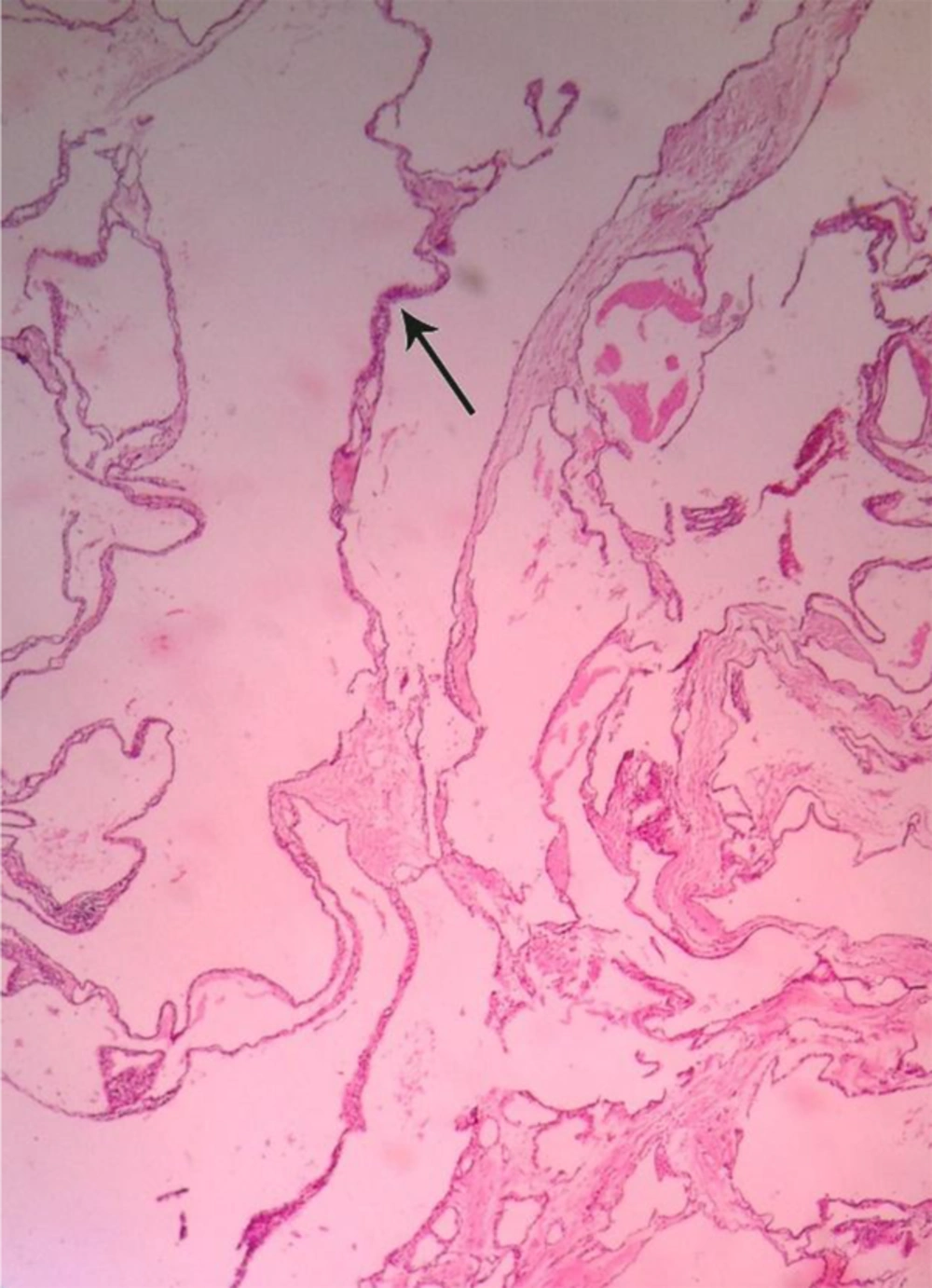
However, histologic findings have revealed numerous cystic like spaces lined by a single layer of flat shaped endothelial cells with well-defined cytoplasmic borders, small round nuclei with dense chromatin. The cystic spaces, which have resembled vascular spaces, filled with homogenous pink fluid and lymphoid aggregates were evident between cystic spaces (Figure 2).
Finally, the diagnosis of pancreatic lymphangioma has confirmed by Immunohistochemistry (IHC) which shown immunoreactivity to factor VIII-R antigen, CD31 positivity and CD34 negativity for cells lining the dilated lymphatic channels.
3. Discussion
Lymphangioma has been a small growing tumor which has resulted from congenital lymphatic malformations causing lymphatic flow obstruction and leading to lymphangiectasis (1, 4). Patients have often presented with nonspecific clinical features resulting from mass effects that have been including abdominal pain, nausea, vomiting, and an associated palpable mass. Among the adults, symptoms tend to develop over months before diagnosis. Some of differential diagnoses were simple cyst, pseudo cyst, cyst adenoma and cyst adenocarcinoma (2) .One of the most important differential diagnoses was pheochromocytoma that should rule out prior to any intervention. Abdominal US usually have revealed polycystic tumor and calcifications which were typical for cyst adenomas (5). CT scan typically has illustrated well-circumscribed homogenous cystic masses in or adjacent to the pancreas. Intravenous contrast injection might enhance septations and thin walls. Large lymphangiomas might displace adjacent organs such as the stomach, spleen, kidney and liver which could demonstrate by CT. MRI typically has not provided much more information (2).
The accurate diagnosis of cystic lymphangioma of the pancreas has confirmed immunohistochemically. Although factor VIII Ag and CD31 were sensitive and reliable markers for lymphatic endothelium identification, CD34 reactivity was commonly negative in lymphatic endothelial cell in contrast to vascular endothelial cells; suggesting that these three markers (factor VIII Ag, CD31 and CD34) could be useful in distinguishing lymphatic endothelium from vascular endothelium (1). It should consider that definite diagnosis of lymphangioma was not possible by these markers. Also staining for D2-40 could be more accurate but was not available in our country.
Another important differential diagnosis of pancreatic lymphangioma has been serous cyst adenoma. Particularly when Lymphangioma contains lymphoid aggregates, locating between cystic spaces, and then commonly developed in peripancreatic tissues rather than the pancreas. In cases with complicated clinicopathologic features, IHC investigations could demonstrate the endothelial nature of lining cells and the absence of keratin in lymphangiomas (6).
Although preoperative evaluations with abdominal sonography or abdominal CT scan could not distinguish lymphangioma from other pancreatic cystic lesions, at the very end, it has seemed histopathology and IHC examination remained the most distinctive yet highly definite approach to the end result (2, 7). While EUS-FNA was a valid procedure for diagnosis of pancreatic cystic lymphangiomas, its role in the treatment of these lesions was controversial. EUS-guided drainage could alleviate symptoms temporarily, but recurrence was inevitable (8). Though Complete surgical excision was the treatment of choice and also curative (1, 9). Depending on the tumor location and size, complete excision could be a simple excision of the mass, or require pancreatic resections, such as a Whipple procedure, or distal pancreatectomy (10) or patient might undergo cystectomy procedure with preservation of the main pancreatic duct (11). indeed incomplete excision was the only reason likely to lead to a local relapse (2).