1. Introduction
Hepatitis B virus has infected more than one-third of the global population. It has been estimated that 360 million chronic carriers are living around the world with a high risk for developing cirrhosis, hepatic carcinoma and hepatic failure (1). Age, male gender, marital status, history of contact with patient, extra-marital sexual contact, intravenous drug use, extensive surgery, visit by the experimental dentists and some jobs such as police, hairdresser and driver are independent factors of developing chronic HBV infection (2).
Prevalence of HBV carriers in low prevalence regions (The USA, Canada, Eastern Europe, Australia and New Zealand) is 0.1% - 2%. It is 3% - 5% in moderate prevalence regions (Mediterranean countries, Japan, Central Asia, Middle East and South America) and 10%- 20% in high prevalence areas (South East Asia, China and Sub Saharan countries). HBV infection prevalence is different among Iranian districts. In a recent population based study in Iran, prevalences of HBc antibody and HBs antigen were estimated as 16.4% and 2.6% respectively indicating that Iran is a country with moderate prevalence of HBV infection (3).
Hepatitis B can be transmitted vertically from mother to fetus or neonate during pregnancy, labor or breast feeding (3-5) or horizontally via intimate contact blood transfusion (4, 5), nosocomial transmission, transplantation and tattooing (4). Vertical transmission is responsible for 35% - 40% of the HBV incident cases worldwide (6). Most of the infected persons have acquired the infection during perinatal or early childhood. Risk of chronicity depends on the age of acquisition and route of transmission and is highest among neonates who acquire infection vertically (6-9). Acute HBV infection in the early pregnancy is associated with 10% risk of perinatal transmission (10), but infection close to or during labor may infect more than 60% of neonates (11). Neonatal HBV infection is often asymptomatic in early life but is associated with increased risk of liver disease in later life. In vertically HBV infected children, risk of developing liver cancer is 200 times more than that of general population (6).
Estimating the prevalence of HBV infection among pregnant women is very important information in control of vertical transmission of the disease. There are variable reports on prevalence HBV infection in pregnant women in Iran. This study aims to estimate the total prevalence of HBV infection among Iranian pregnant women using systematic review and meta- analysis methods.
2. Methods
The current study is a systematic review and meta- analysis estimating the prevalence of Hepatitis B Virus infection among pregnant women living in Iran. This study was carried out based on the review of the literature.
Search Strategy: To find published electronic papers until 31 December, 2015, we searched national (SID, Iranmedex, Magiran and Irandoc) and international (PubMed, Google Scholar, Scopus and Science direct) databases using the following keywords and their Farsi equivalents:
“Prevalence”, “Seroprevalence”, “Frequency”, “Seroepidemiology”, “Hepatitis B”, “HBsAg”, “HBV”, “Hepatitis B Surface Antigen”, “Hepatitis B Virus Infection”, “Pregnant women”, “Pregnancy”, and “Iran”.
The search was conducted during 1 - 15 January, 2015. We also investigated the references of studies to increase the search sensitivity and number of identified studies. To reduce the risk of publication bias, we interviewed with relevant experts and some research centers to find probable unpublished papers in the field of our systematic review/meta- analysis. Finally, another researcher randomly evaluated this search and found that all relevant studies had been collected in the search. In addition, we estimated Egger and Begg indicators to evaluate the degree of bias. Moreover, to minimize other kinds of bias, we probed the results and omitted the repeated researches.
2.1. Study Selection
Full texts or abstracts of all papers, documents and reports identified during the advanced search were collected. After excluding duplicates, we removed irrelevant articles investigating the titles, abstracts and full texts of the remained papers respectively.
2.2. Quality Assessment
Selected studies during the above mentioned processes were quality assessed using a specific checklist (12). This checklist was designed using STROBE checklist contents (13) including 12 questions regarding different aspects of methodology such as appropriate sample size, type of the study, sampling methods, study population, data collection methods, definition of the variables and method of dealing with samples, data collection tools, statistical analysis tests, study objectives, illustration of the results and presentation of the findings based on the objectives. Each question was assigned one score and studies obtained at least eight quality scores (12) entered into the final meta- analysis.
2.3. Data Extraction
Two researchers independently extracted all necessary data such as title, first author name, date of the study conduction, number of recruited pregnant women, sampling method, type of the study, HBV infection prevalence, average parity, site of the study conduction, publication language, mean age of the studied women, frequency of HBV vaccine coverage in each study, P value of the relationship between HBV prevalence and some variables including age, vaccination status, tattooing, high risk sexual behavior, history of imprisonment, familial history of hepatitis B, IV drug addiction, history of visit by dentist, job and area of residence. The agreement between information extracted by the two researchers were also evaluated. All data were inserted into the Excel spreadsheet.
2.4. Eligibility Criteria
2.4.1. Participants
All selected studies had to be conducted among Iranian pregnant women.
Intervention and comparison: Since we needed information about prevalence, only descriptive and some cohort studies were eligible for our meta-analysis. Therefore, analytic studies such as case controls (reporting odds ratio) or experimental studies (implementing intervention) were excluded from our systematic review. That was the case for “comparison” which was not reported in our selected papers.
2.4.2. Outcome
The main outcome required for the final meta-analysis was “prevalence”.
Statistical analysis: We calculated the standard error of prevalence according to the binomial distribution formula. Cochrane test (Q) and I2 indicator were applied to detect the degree of heterogeneity among the results of the selected studies. Based on these indices, we estimated the pooled prevalence of HBV infection among Iranian pregnant women using random effects model. To minimize the random variations between the point estimates of the primary studies, results of all studies were adjusted using Bayesian Analysis method. We also fitted meta-regression models to investigate the sources of the heterogeneity. Moreover, sensitivity analysis was performed to detect studies with most influence on this heterogeneity. Point prevalences as well as their 95% confidence intervals were illustrated by forest plots. In these plots, size of each box indicated the weight of the study, while, each crossed line referred to 95% confidence interval. All data analyses were performed using Stata SE V.11 software.
3. Results
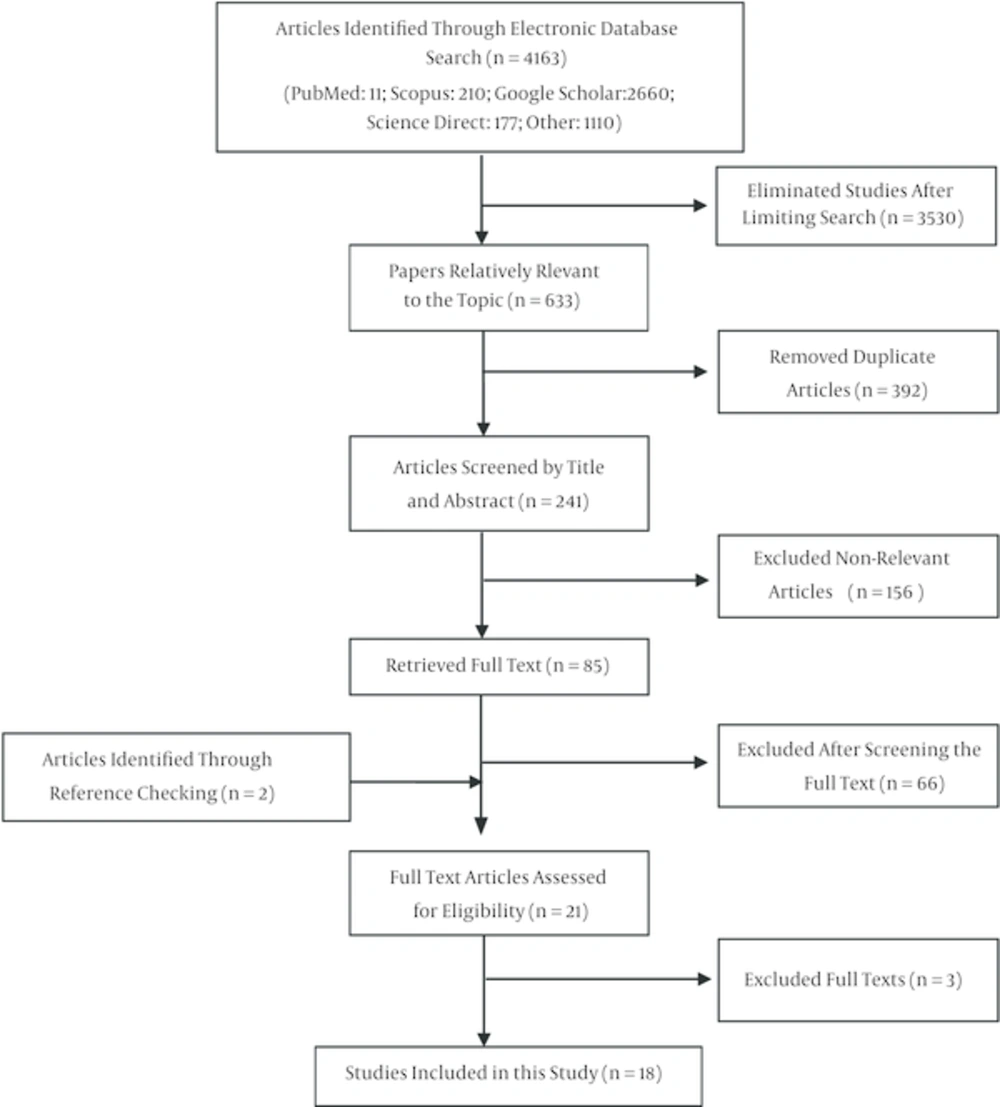
In the first step of our search, 4163 studies regarding HBV infection prevalence were identified which were reduced to 633 after limiting the search strategy. Having excluded duplicates, 392 papers were excluded. Reviewing titles and abstracts, 156 articles and reviewing full texts, 66 papers were removed. Moreover, two studies were added after investigating full texts and references. Finally, quality assessment and applying inclusion/ exclusion criteria were performed and 18 papers (14-31) were identified eligible for meta- analysis (Figure 1).
These 18 studies were carried out in 15 provinces of Iran from 1994 to 2014. Of these, 14 studies reported the type of the study (descriptive-analytical). Sampling design were consensus (six studies), randomized (three studies), facilitated (seven studies) and unknown (two studies). Diagnostic test (ELISA) was reported in 16 studies. Mean age of pregnant women specified in 12 studies ranged from 24.5 years in the study carried out by Yadegari (29) to 28.9 years in Mohammad Jafari study (30). Average gravidity was calculated in five studies varied from 1.8 (14) to 2.7 (25, 30) (Table 1).
| Id | First Author | Publication Year | Sample Size | Mean Age | Average Pregnancy Number | Prevalence of Positive HBsAg, % | Received Hepatitis B Vaccine | Association Between Prevalence of Positive HBsAg in Pregnant Women | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level Education | Age | Sexual High-Risk Behavior | Tattooing | Blood Transfusion | Dental Affairs | Drug Injection | Imprisonment | Residence | Job | Family History | ||||||||
| 1 | Ahmadi (14) | 2011 | 1078 | 26.1 | 1.79 | 0.5 | 12.5 | - | - | 0.009 | 0.03 | NS | NS | NS | NS | - | - | NS |
| 2 | Aali (25) | 1999 | 1002 | 26.5 | 2.7 | 2.3 | 4.2 | - | - | - | - | - | - | - | - | NS | 0.008 | - |
| 3 | Aminzadeh (15) | 2004 | 600 | 26.2 | 2.1 | 1.3 | 1 | - | - | - | 0.01 | NS | NS | 0.04 | - | NS | NS | - |
| 4 | Cheraghali (16) | 2012 | 1553 | - | - | 1 | - | - | - | - | NS | NS | - | NS | - | - | NS | < 0.001 |
| 5 | Mirghaforvand (26) | 2007 | 187 | - | - | 3.2 | 6.4 | NS | NS | - | - | - | - | - | - | NS | NS | - |
| 6 | Mohammadian et al. (17) | 2014 | 1317 | 26.7 | - | 0.4 | 8.6 | < 0.001 | NS | - | - | - | - | - | - | NS | - | - |
| 7 | Mohebbi (18) | 2011 | 827 | 26.1 | - | 0.7 | - | NS | NS | - | - | - | - | - | - | NS | NS | - |
| 8 | Mojibian (24) | 2001 | 1904 | 25.6 | - | 0.84 | 0.8 | - | - | - | - | - | - | - | - | - | - | - |
| 9 | Motamedifar (19) | 2012 | 237 | - | - | 0.8 | 22.8 | - | < 0.05 | - | - | - | - | - | - | - | NS | < 0.05 |
| 10 | Motazakker (27) | 2014 | 368 | 25.9 | - | 0.8 | - | NS | NS | - | - | - | - | - | - | NS | NS | - |
| 11 | Sahaf (28) | 2007 | 680 | 28.7 | - | 2.5 | - | - | - | - | - | - | - | - | - | - | - | - |
| 12 | Salimi (20) | 2014 | 9321 | - | - | 1.7 | - | NS | < 0.05 | - | - | - | - | - | - | < 0.05 | NS | - |
| 13 | Sharifi (21) | 2006 | 323 | 25 | - | 3.4 | - | - | NS | - | - | NS | NS | NS | - | - | NS | < 0.05 |
| 14 | Sharifi-Mood (22) | 2004 | 200 | - | - | 6.5 | - | - | - | - | - | - | - | - | - | - | - | - |
| 15 | Tabasi (23) | 2003 | 2000 | 24.6 | - | 0.35 | - | < 0.05 | NS | - | - | NS | - | - | - | - | - | < 0.05 |
| 16 | Mohammad Jafari (30) | 2004 | 1200 | 28.9 | 2.7 | 1.7 | - | - | - | - | - | - | - | - | - | - | - | - |
| 17 | Hasanjani rooshan (31) | 1994 | 1456 | - | - | 1.6 | - | - | - | - | - | - | - | - | - | - | - | - |
| 18 | Yadegari and Doaee (29) | 1998 | 600 | 24.5 | 2.5 | 1 | - | - | - | - | - | - | - | - | - | - | - | - |
Baseline Characteristics of Included Studies in Meta-Analysis of Prevalence of Positive HBsAg in Pregnant Women in Iran
The frequency of women receiving hepatitis B vaccine was reported in seven studies ranged from 0.8% in the study conducted by Mojibian (24) to 22.8% in the study performed by Motamedifar (19). Only six studies investigated the association between HBV infection and level of education two of which reported significantly higher rates of infection among women with low educational levels. Among eight studies investigated the relationship between HBV infection and age, two studies found that the infection prevalence was significantly higher among younger women (Table 1).
The relationship between HBV infection and high risk sexual contact was investigated in only one study, and significantly higher rates of infection among pregnant women with history of such behavior were observed. Of two studies reporting the association between HBV infection and tattooing, both found a significant association. None of the five studies assessing the correlation between HBV infection and blood transfusion proved any significant association. That was the case with the association between HBV infection and referring to the dentist which was investigated in three studies.
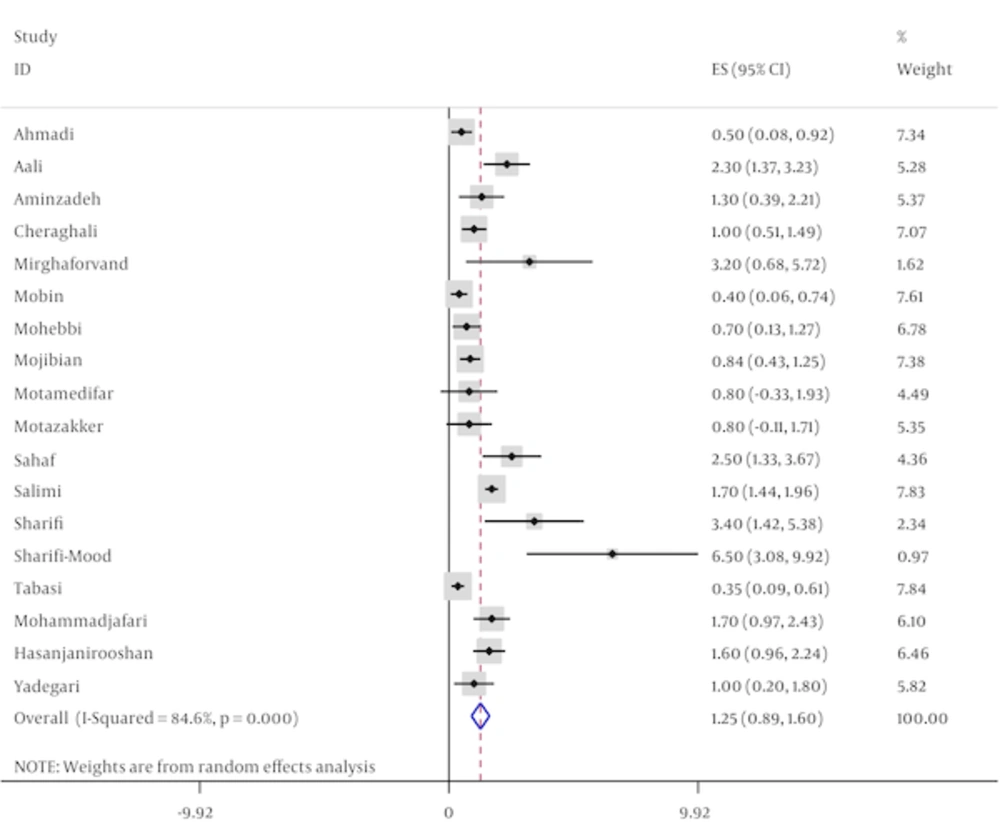
Of the studies entered into the current systematic review, four studies investigated the association between HBV infection and intravenous drug abuse, one of which showed a significant relationship. The only study, which compared the infection rate between pregnant women with and without history of imprisonment, did not prove any significant difference. Living in rural areas was significantly associated with HBV infection in only one study from seven articles that assessed such association. Among eight studies reporting association of HBV infection with job, one study reported that employed pregnant women had more frequency of HBV infection in comparison with housewives. In five studies, which investigated the relationship between familial history of HBV infection and developing HBV infection in pregnant women, four studies showed that this infection was significantly higher among those with positive familial history (Table 1). Among primary studies, prevalances of HBV infection varied from 0.3% in Tabasi study (23) that estimated the prevalence of infection for 2000 pregnant women in Isfahan province in 2003 to 6.5% in the study conducted by Sharifi-Mood (22) among 200 pregnant women in Sistan and Baloochistan province in 2004. Having adjusted the results using Bayesian analysis, the corresponding data changed to 0.4% (23) and 1.9% (22) respectively (Table 1 and Figure 2).
Totally, 24853 pregnant women were investigated in the current meta-analysis regarding the HBV infection prevalence. Based on random effect model, the pooled prevalence (95% confidence interval) of HBV infection among Iranian pregnant women was estimated as 1.24% (0.88 - 1.6). According to the sensitivity analysis, two studies conducted by Salimi (20) and Tabasi et al. (23) were identified as the studies influencing the heterogeneity between the results of the studies. Excluding these studies from the meta- analysis, prevalence of HBV infection among pregnant women was estimated as 1.25% (0.89 - 1.61) and the index of heterogeneity changed from 84.6% to 74.1%. However, a considerable heterogeneity still remained between the results (Table 2).
| Prevalence by | Sample Size | Pooled Estimate (%), 95% CI | Heterogeneity Test | Heterogeneity (I-Squared-%) | |
|---|---|---|---|---|---|
| Chi-squared(Q) | P Value | ||||
| Before sensitivity test and with all related primary studies | 24853 | 1.24% (0.88 - 1.6) | 110.1 | < 0.001 | 84.6 |
| After sensitivity test and removed influence studies in heterogeneity (20, 23) | 13532 | 1.25% (0.89 - 1.61) | 57.9 | < 0.001 | 74.1 |
Pooled Estimated of Positive HBsAg Prevalence in Pregnant Women in Iran, According to the Result of Meta-Analysis
Different factors associated with the heterogeneity such as publication date and mean age of the participants were investigated using meta-regression models, none of these variables were statistically significant (Table 3).
| Variables | Coefficient | P Value |
|---|---|---|
| Publication year | -0.03 | 0.3 |
| Average age | 0.3 | 0.1 |
Related Factor With Heterogeneity of Positive HBsAg Prevalence in the Current Meta-Analysis (Based on Univariate Meta Regression)
4. Discussion
In this meta- analysis, we estimated the overall prevalence of HBV infection among Iranian pregnant women as 1.2% with 95% confidence interval of 0.9% - 1.6%. Among the different risk factors investigated in our systematic review, HBV infection prevalence was significantly higher in pregnant women with familial history of infection.
Table 4 shows that the prevalence of HBV infection among pregnant women was lower than that of general population and IV drug users, while it was higher than that in blood donors. The lower rates of infection among blood donors might be due to the high frequency of volunteers in such groups most of which are healthy. Higher rates of HBV infection among IV drug users are predictable due to their risky behaviors. In addition, HBV prevalence is higher among general population partially because of their higher mean age. Those aged more than 25 years old did not receive HBV vaccine routinely in infancy and many acquired infection in childhood or later in early adulthood.
Prevalence of Hepatitis B Virus Infection in other Population Group in Iran According to Results of Meta-Analysis that Published Previously
According to Table 5, prevalence of HBV infection among pregnant women living in India, Spain, Denmark, Guatemala and Brazil is more than that estimated for Iranian pregnant women in this meta- analysis. But HBV infection prevalence among pregnant women living in Nigeria, Uganda, Ethiopia, Mauritania, Mali, Yemen and South Africa was much higher than the prevalence among Iranian pregnant women. In addition, Pakistani, Libyan and Turkish pregnant women were slightly more infected than Iranian women (4, 7, 32-51). Higher infection rates in most African countries and lower rates among women in most European countries indicates the effect of health promotion and vaccine coverage on the patterns of infection. Moreover, it seems that the prominent patterns of transmission in African countries are sexual, unsafe injection and vertical from mother to child, while the dominant pattern in Iran before wide coverage by HBV vaccine was occult parenteral and vertical.
| Number | First Author | Country | Prevalence of Hepatitis B Virus Infection, % |
|---|---|---|---|
| (32) | Chatterjee | India | 1.09 |
| (4) | Saraswathi | India | 0.9 |
| (33) | El-Magrahe | Libya | 1.5 |
| (34) | Musa (Based on Meta-analysis) | Nigeria | 14.1 (9.6, 18.6) |
| (35) | Oluboyo | Nigeria | 6 |
| (36) | Pennap | Nigeria | 6.68 |
| (37) | Olokoba | Nigeria | 8.2 |
| (38) | Utoo | Nigeria | 6.6 |
| (7) | Bayo | Uganda | 11.8 |
| (39) | Sabir | Pakistan | 1.7 |
| (40) | Uyar | Turkey | 2.1 |
| (41) | Yavuzcan | Turkey | 1.47 |
| (42) | Ramos | Ethiopia | 6.1 |
| (43) | Mansour | Mauritania | 10.7 |
| (44) | Salleras | Spain | 0.1 |
| (45) | MacLean | Mali | 8.01 |
| (46) | Harder | Denmark | 0.26 |
| (47) | Murad | Yemen | 10.8 |
| (48) | Andersson | South Africa | 2.9 |
| (49) | Samayoa | Guatemala, Central America | 0.22 |
| (50) | Lima | Brazil | 1 |
| (51) | Souza | Brazil | 0.9 |
Prevalence of Hepatitis B Virus Infection in Pregnancy Women in the Other Country
In the study conducted by El- Magrahe et al. in Libya (33), prevalence of positive HBS antigen among pregnant women aged more than 25 years was more than that of younger women, although the difference was not statistically significant. In the current systematic review, in all primary studies assessing the effect of age, HBV infection was more common among older women. Moreover, all positive HBS antigen neonates had been born from positive HBS antigen mothers, i.e. vertical transmission plays a main role in the development of infection among Iranian women.
In another study carried out by Dwivedi et al. in India (52), history of tattooing was reported in 78.4% of pregnant women. In the current systematic review, out of three primary studies investigating this history among Iranian pregnant women, two studies reported a significant relationship between tattooing and HBV infection. In Oluboyo et al. study in Nigeria (35), a high prevalence of infection was reported (Table 5). The majority of HBS antigen positive individuals aged between 15 - 20 years. In addition, similar to the results of three primary studies in the current systematic review, frequency of women with history of blood transfusion was higher among HBV infected group, although the difference was not statistically significant.
In a study conducted in Nigeria (36), authors reported more HBV infection rate in comparison with the current study; prevalence of positive HBS antigen was higher in pregnant women aged 40 - 44 years, illiterate, higher gravidity, with history of surgery and blood transfusion. This indicates various patterns of transmission in communities with high HBV infection prevalence. In a study performed in Uganda, frequency of positive HBS antigen was higher in pregnant women under 20 years compared to those aged more than 20 years (OR = 2.45). In that study, the number of sexual partners was not reported as a predictor for HBV infection among pregnant women (7). In another study carried out in Nigeria with 16.5% infection prevalence among pregnant women, the highest infection rate was observed in 30 - 34 year- old age group (23.3%) and no significant association was found between infection and age, educational level and job. However, it was significantly associated with history of hepatitis B vaccination (53).
Results of our systematic review and meta- analysis agree with the establishment of strategy of screening pregnant women regarding hepatitis B infection. Since vertical transmission during pregnancy or labor, usually leads to being a chronic carrier, diagnosis of infected pregnant women can prevent developing infection and disease in neonates.
There were some limitations during the current systematic review/ meta- analysis that restricted investigation of all aspects of the HBV infection prevalence. For example, risk factors of HBV infection were not report in many primary studies. Therefore, we could not exactly detect all determinants of infection among Iranian pregnant women.
4.1. Conclusions
In conclusion, our study provided evidence regarding low prevalence of hepatitis B infection among Iranian pregnant women and also showed the familial history as the only determinant factor for infection in this group. Therefore, it seems that vertical type is the dominant pattern of transmission among pregnant women in Iran.