1. Background
Esophagus cancer was the eighth most common cancer in the world in 2008. Also, in the same year, it was the sixth most common cause of death from cancer worldwide and most of these incidences and mortalities occurred in developing countries (1). The south-eastern coast of Caspian Sea is one of the highest incidence areas for esophageal cancer in the world (2). Cancer is the third cause of mortality in Iran. So this disease is an important public health issue in this country. Esophagus cancer has high incidence in north and northwestern regions of Iran (3). Accurate cancer incidence data are essential for planning, monitoring and evaluating national and regional cancer control programs (4).The purpose of population based cancer registries is to estimate the cancer burden in the area covered, to observe trends and regional differences and to provide a database for epidemiological research (5).
As the decision makers in health authorities set their policies according to the results of data registration, they need to know how much the data registration process is reliable. Therefore, completeness of registration is used as one of the measures of quality of a cancer registry (5, 6). Completeness is defined as the proportion of incident cancer cases that is registered (5). Completeness level of cancer registration is one of the main parts of quality control in such registration (7). Since most cancer registries employ more than one data source for case finding, capture-recapture methods may be used to estimate the number of incident cases in the population, and hence to assess completeness of case ascertainment (8).
Capture-recapture is the method widely used in wildlife population censuses (9). Another important application of this method in epidemiology is to estimating the prevalence of a particular disease and also estimating the completeness of ascertainment of disease registers. However, capture-recapture method can principally be applied to any situation where there are two or even more incomplete lists (10). Two assumptions have to be made when using the simple capture-recapture method. Firstly, the sources are independent, and secondly, all individuals within the same source have an equal chance of being included (9, 11). The use of capture-recapture methods is very efficient for reducing the costs of disease registration as well as reducing bias in incidence estimations and in the case of comparing population subgroups (7). Ardabil province is located in Northwestern Iran, an area 70 km inland from the western Caspian coastline. The esophagus cancer is the second prevalent cancer in both males and females. Also, upper digestive tract cancers are the leading cause of 43% death in Ardabil province (2). The pathology-based cancer registry has been established in Ardabil province since 1999. For the first time in Iran, the population based cancer registry was established in Ardabil in 2003. The Ardabil Cancer Registry (ACR) actively collects information of cancer incidence from Pathology-based, hospital-based and death certificates. The main goal of the ACR is to measure cancer incidence and mortality in residents of Ardabil province (12).
2. Objectives
This study aims to estimate the incidence rate of esophagus cancer in Ardabil by capture-recapture method using log linear model.
3. Patients and Methods
This study was conducted in Ardabil Province which is located in the north-west of Iran. All new cases of esophagus cancer reported by three sources: pathology reports, death certificates, and medical records reported to Ardabil population-based cancer registry in 2006 and 2008 were enrolled in the study. All duplicates in each source were identified and removed using EXCEL software. Some characteristics such as name, surname, father’s name, date of birth and ICD codes related to their cancer type were used to identify the common cases among three sources. The incidence rate of esophagus cancer was estimated by the capture-recapture method and log-linear models. To use capture-recapture method, two main assumptions should be considered, sources of information should be independently and all people who are in every data source should have an equal chance to presence in the study (9, 11). However, in most human populations and medical science studies, usually these assumptions are not established and different sources are not independent. Three source capture-recapture and log-linear model were used to estimate the completeness and more accurate incidence rate of esophagus cancer in Ardabil province. With three registers, there are eight possible combinations of these registers in which cases do or do not appear. The general model uses eight parameters: the common parameter (the logarithm of the number expected to be in all lists), three ‘main effects’ parameters (the log odds ratios against appearing in each list for cases who appear in the others), three ‘two-way interactions’ or second order effect parameters (the log odds ratios between pairs of lists for cases who appear in the other), and a ‘three-way’ interaction parameter. For three registers, A with i levels, B with j levels, C with k levels, the natural logarithm (ln or loge) of expected frequency Fijk for cell ijk, lnFijk, can be denoted as:

where θ is the common parameter, λA, λB, and λC are the main effect parameters, λAB, λAC and λBC are the second order effect (two-way interaction) parameters and λABC is the highest order effect (three-way interaction) parameter. The value of this last three-way interaction parameter cannot be tested from the study data and is assumed to be zero (13).To assess how the various log-linear models fit the data (model fitting) and select the best model, we used the log likelihood-ratio test, also known as G2 or deviance, Akaike’s information criterion (AIC) and Bayesian information criteria (BIC) which they can be expressed as:

Where Obsj is the observed number of individuals in each cell j, and Expji is the expected number of individuals in each cell j under model i.

Where the first term, G2, is a measure of how well the model fits the data and the second term, 2[df], is a penalty for the addition of parameters (and hence model complexity).

Where Nobs is the total number of observed individuals.
The lower the value of G2, AIC and BIC the better is the fit of the model (13). AIC is the more appropriate criteria which is used by researchers for model selection (14-16). Therefore, we used these criteria for evaluating the fitting quality. Finally the model with lower amount of the AIC was chosen as the best model.
Estimated incidence was calculated based on the estimated new cases of esophagus cancer (by use of selected model in log-linear analysis) at a certain time over the number of the population at risk in Ardabil province at that time. All the incidences are reported based on the incidence per one hundred thousand populations. Also the completeness was calculated over age groups and calendar time, respectively. The informed consent was written by Ardabil cancer registry center and the authors certified that. In all stages of this study the individual’s information such as name, surname and other characteristics were kept confidential. The P Values, less than 0.05, were considered significant. We used STATA software, version 12 (StataCorp, Texas, USA) for all computations.
4. Results
After investigating and removing duplicate cases between three sources, a total number of 471 new cases of esophagus cancer were reported to Ardabil population-based cancer registry in 2006 and 2008. The pathology source, hospital records and death certificates were reported 277, 193 and 152 new cases of esophagus cancer, respectively. Of 471 subjects 266 (56.50%) were male. The mean age of participants was 67.60 (± 12.91) years for men and 65.48 (± 13.58) years for women.
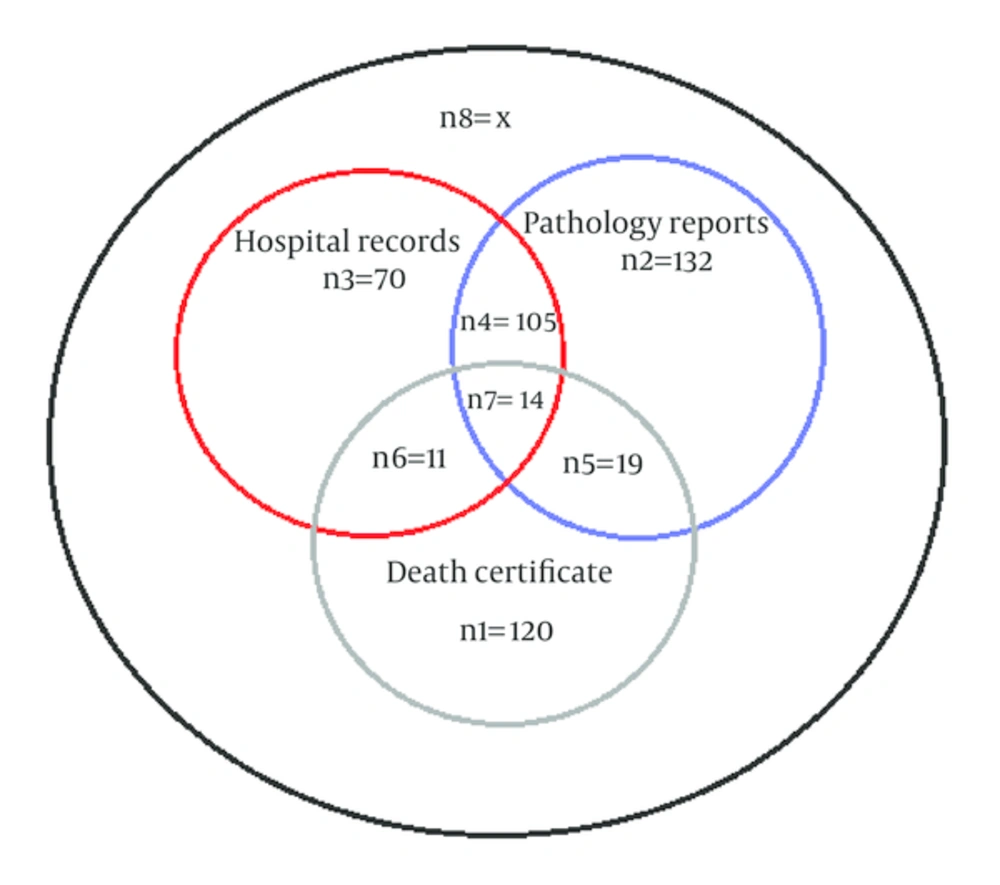
Venn diagram shows the common cases between pathology reports, hospital records and death certificate (Figure 1). In three source capture-recapture analysis, the log-linear model, a model in which two sources of pathology and medical records were mutually interdependent and death certificates source were independent, was chosen as the best model with the lowest value of Akaike’s Information Criterion and Bayesian Information Criterion (Table 1). The estimated total number of esophageal cancer in 2006 and 2008 was 1308.27 (95%CI: 1053.34 - 1674.80). The completeness of registration for all three sources after removing duplicates was 36% (471 cases) and also for pathology reports, hospital records and death certificates were 21.17% (277 cases), 14.75% (193 cases) and 11.61% (152 cases), respectively. The incidence of esophagus cancer was estimated generally and to the sex subgroups based on the estimated new cases of an esophagus cancer (by use of selected model in log-linear analysis) (Table 2). The estimated incidence rate of esophagus cancer for 2006 and 2008 was 49.71 (95% CI: 37.79 - 69.12) per 100,000 populations and 53.87% (95% CI: 38.97 - 7964.82) per 100,000 populations, respectively. In sex groups, the estimated incidence rate in male for 2006 and 2008 was 68.22 (95% CI: 45.17 - 113.32) per 100,000 populations and 58.81 (95% CI: 38.93 - 99.50) per 100,000 populations, respectively. The female estimated incidence rate for 2006 and 2008 was 33.17 (95% CI: 24.38 - 51.57) per 100,000 populations and 48.15 (95% CI: 30.31 - 89.88) per 100,000 populations, respectively. Also, the estimatedcompleteness of esophagus cancer registration for 2006 and 2008 was 37.76% and 34.36%, respectively.
| Model | X | N | 95% CI for N | DF | G2 | BIC | AIC |
|---|---|---|---|---|---|---|---|
| 258.71 | 729.71 | (673.84 - 800.96) | 4 | 102.25 | 145.48 | 145.80 | |
| 837.27 | 1308.27 | (1053.34 - 1674.80) | 5 | 0.14 | 49.33 | 49.60 | |
| 145.92 | 616.92 | (577.59 - 670.75) | 5 | 51.29 | 108.43 | 108.70 | |
| 192.26 | 663.26 | (616.92 - 724.31) | 5 | 71.51 | 126.62 | 126.89 | |
| 763.63 | 1234.63 | (865.52 - 1949.07) | 6 | 0.04 | 51.17 | 51.50 | |
| 833.68 | 1304.68 | (970.05 - 1863.68) | 6 | 0.14 | 51.28 | 51.60 | |
| 88 | 559 | (533.18 - 595.53) | 6 | 23.62 | 70.62 | 70.95 | |
| 707.36 | 1178.36 | (734.06 - 2373.06) | 7 | 0.00 | 53.08 | 53.46 |
Model Selection in Log-Linear Analysis by AIC, BIC and G2Statistics
| Subgroups for Each Year | Reported Incidence Rate, per 100,000 | Estimated Incidence Rate, per 100,000 | 95% CI for Estimated Incidence Rate |
|---|---|---|---|
| Male | 21.08 | 68.22 | (45.17 - 113.32) |
| Female | 16.33 | 33.17 | (24.38 -51.57) |
| Total | 18.77 | 49.71 | (37.79 - 69.12) |
| Male | 19.95 | 58.81 | (38.93 - 99.50) |
| Female | 16.99 | 48.15 | (30.31 - 89.88) |
| Total | 18.51 | 53.87 | (38.97 - 79.64) |
Estimated Incidence of Esophagus Cancer by Log-Linear Model Based on Ardabil Population in 2006 and 2008
5. Discussion
In this study, the incidence rate of esophagus cancer was estimated by the capture-recapture method and log-linear models. The mean age of all subjects was 66.68 ± 13.23 years (67.60 ± 12.91 for men and 65.48 ± 13.58 for women). The age distribution does not show the difference between men and women and slightly higher than the average age reported by studies conducted in other parts of Iran that reported average age 58 - 65 years for esophagus cancer (17-19), but reported average age in the study conducted in Tehran metropolitan was 70.40 (70.5 for men and 70.3 for women) that is slightly higher than present study (7). Male to female ratio was 1.29 that is consistent with international and regional reports (2, 7, 20).
In log-linear analysis, the model where sources pathology and hospital records are dependent and independent of the source death certificates was selected. In this study, we select the best model using AIC, BIC and G2 statistics. The description of this relationship in situations as to what happens in society seems also logical, especially about dependencies between pathology reports and hospital records. The reported incidence rate of esophagus cancer based on population based cancer registry in Ardabil province, after removing duplicate cases between pathology reports, hospital records and death certificates, for 2006 and 2008 years was 18.77 per 100,000 and 18.51 per 100,000 populations, respectively. Also the registered incidence rate in men and women, after removing the duplicates between sources, in 2006 was 21.08 and 16.33 per 100,000 populations, and in 2008 was 19.95 and 16.99 per 100,000 populations, respectively. Babaei et al. reported esophagus cancer incidence as 19.5 per 100,000 populations during 2004 to 2006 years (21). This result is consistent with the registered incidence rate in this study. The estimated incidence rate of esophagus cancer in log-linear analysis, with consideration of the number of cases not registered in any sources, for 2006 and 2008 was 49.71 (95% CI: 37.79 - 69.12) per 100,000 populations and 53.87(95% CI: 38.97 - 79.64) per 100,000 populations, respectively. In a study conducted in Tehran, the estimated incidence of esophagus cancer was reported 10.5 per 100,000 populations, respectively (7). Also the estimated incidence rate reported by Globocan for man and woman in Iran was 9 and 8 per 100,000 populations, respectively (22). But this estimation is for the country in general, while in Iran, most northern and northwestern areas are at high risk for esophagus cancer. Also the central and western provinces are at medium risk and the southern regions are at a low risk (23). As Ardabil is located in northwestern of Iran and has the highest incidence of esophagus cancer in Iran (23), the higher incidence in this study seems reasonable. The estimated completeness in log-linear analysis for 2006 and 2008 was 37.76% and 34.36%, respectively. The completeness of cancer registries in our study is much lower than other countries that reported 96 % to 99.6% for all types of cancers in overall (8, 24, 25) and also for gastrointestinal cancers in Canada was reported 95.83% (8). The completeness of esophagus cancer registry in Tehran was reported 27.3% (7) and is consistent with results of our study. Thus the results of our study confirmed that the quality of cancer registry in Iran is inappropriate and needs more attention to amplify its quality. Some strategies such as use of national code of patients instead of name and surname, universal online registry using electronic health records, training cancer registry staffs and also training of death registry staffs about the immediate or underlying cause of death must be used to improve the quality of the cancer registry system.