1. Introduction
Nasopharyngeal carcinoma lymphoepithelioma has been very rare among the children. Only 3% of all nasopharyngeal carcinoma cases havee observed among the children less than 19 years which make up to 1% of all childhood cancers (1-3). Nasopharyngeal carcinoma (NPC) has known as a malignancy of the postnasal space. This cancer was highly prevalent in southeast China, with an incidence varying between 30 and 80 cases per 100,000 per year, and among Eskimos, with an incidence of 25 cases per 100,000 per year. An intermediate incidence of NPC has found in the Mediterranean basin and among Arabic populations from North Africa [8 – 12 cases per 100,000 per year compared with, 1 case per 100,000 per year in Western countries]. It has suggested that the Geographic and genetic factors may also play a role in its occurrence. Some studies in Asia and Mediterranean region or basin have suggested a relation between salted fish and meat with nasopharyngeal carcinoma incidence due to releasing volatile nitrosamines during cooking (1). In addition, nasopharyngeal carcinoma has associated with specific HLA (human leukocyte antigen) alleles such as B17, BW46, AW19, Bsinz, and A2. Epstein-Barr virus (EBV), alcohol and tobacco have also been risk factors for nasopharyngeal carcinoma (1-4). So far, the world health organization has introduced three histological types of nasopharyngeal carcinoma. Type I: Keratinizing squamous cell carcinoma which has associated with EBV infection, and alcohol and tobacco consumption. Type II: Non-keratinizing epidermoid carcinoma. Type III: lymphoepithelioma which has been an undifferentiated carcinoma. Almost all nasopharyngeal carcinomas in children were type III (4). NPC was more common in males. The mean age of occurrence is 13 years old and the most common involved site is Rosen- muller's fossa. It has frequently presented as a painless upper neck mass which has associated with palpable cervical lymphadenopathy. Tumor infiltration could cause hearing loss, tinnitus, nasal obstruction, epistaxis and dysphagia. Cranial nerve XII and VII involvement might cause diplopia. Other symptoms might include vision disturbances, Ageusia and flaccidity of shoulder. The most common sites of distant metastases were lungs, bones, mediastinum, bone marrow, and visceral organs. Paraneoplastic symptoms such as hypertrophic osteoarthropathy (HOA), dermatomyositis (DM), and inappropriate antidiuretic hormone secretion have seen in advanced cases. Differential diagnoses have commonly included Rhabdomyosarcoma and lymphoma. angiofibroma was the most common benign tumor of the nasopharynx (1-4). Because of its rarity in children, the diagnosis has often delayed, and most patients have presented at advanced stage (III or IV) of the disease. Moreover NPC treatment guidelines were controversial (2). Serological evidence of EBV infection has seen mostly in patients. Circulating EBV DNA analysis has helped to evaluate the response to treatment and relapse (5). Patients with metastatic disease at diagnosis had a poor prognosis. Although, it has not associated with size of the mass (6). The most important prognostic factor was pathological subtype and early response to treatment (2). Radiotherapy has remained the main treatment modality for NPC. Limited involvement of the nasopharynx with or without extension to parapharyngeal space (T1, T2) could be treated with radiotherapy 65 to 70 Gy. These regions were inaccessible for surgery (1-3, 7). NPC was a very sensitive tumor to chemotherapy. Neoadjuvant therapy followed by local radiation therapy; has improved the prognosis of children with advanced disease (1, 3, 7). Neoadjuvant chemotherapy could diminish margin of tumour and destroy hidden metastases, which ameliorate survival (8).Cisplatin, methotrexate (MTX), leucovorin (LV), fluorouracil (5-FU) has used more frequently and have associated with event-free survival rates (EFS) of 77% at 4 year (7). Neoadjuvant chemotherapy in children has carried less risk and yields better outcomes due to limiting the dose of radiation (6).
2. Case Presentation
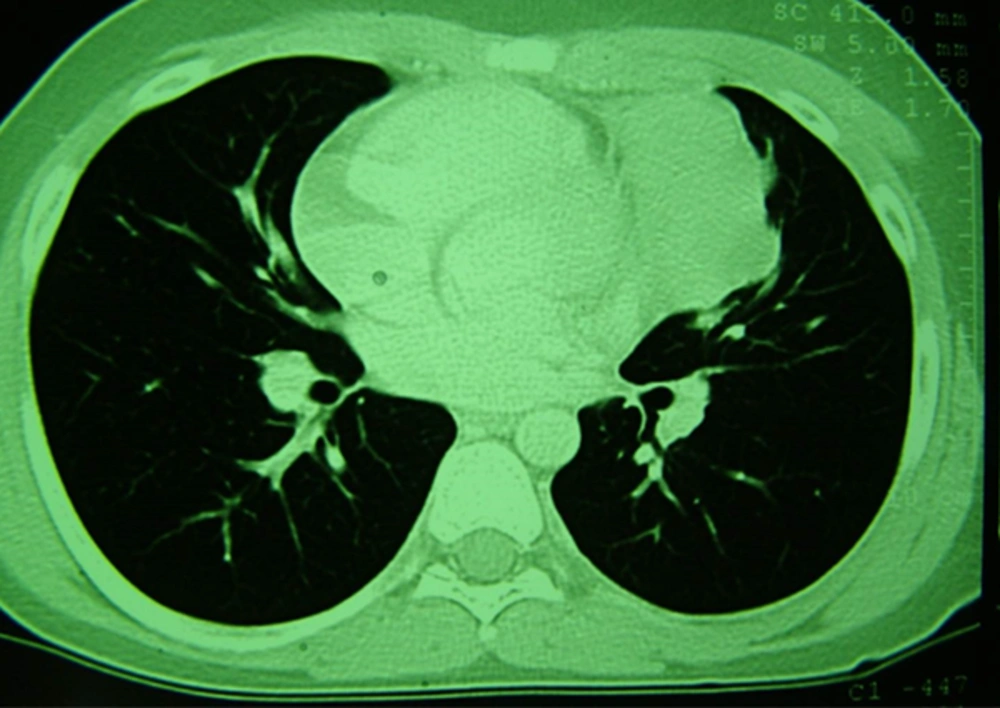
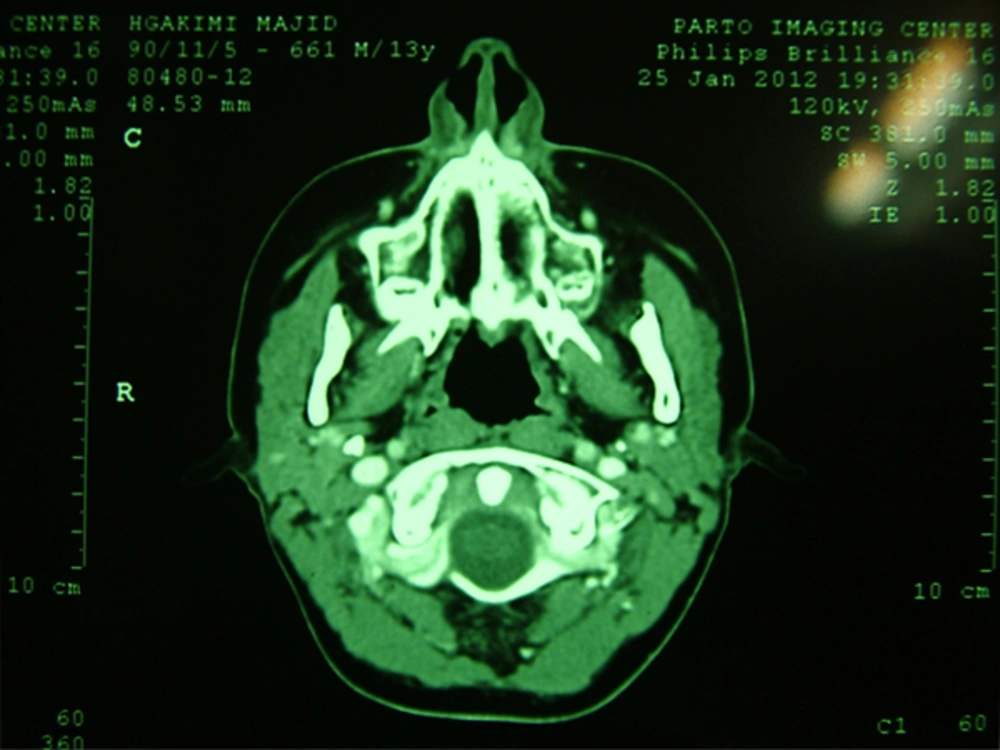
A 15-year-old patient with a history of chest pain and a left sternal mass over two years ago has referred to our medical center.Within a few weeks, mediastinal mass progressed quickly. The patient's CT scan has revealed a soft tissue mass adjacent to the heart and the left side of anterior mediastinum (Figure 1). In addition, a small mass attached to the posterior wall of the left diaphragm has seen in the lung parenchyma. The patient had no pleural effusion. It has also shown the lack of involvement of the nasopharynx on serial MRI and CT scans (Figure 2).
The patient underwent nasopharyngoscopy as well as biopsy from multiple regions. Pathologic evaluation has revealed lymphoid hyperplasia and chronic inflammatory changes with no evidence of neoplastic tissue. The patient had no cerebral, abdominal or bone marrow involvement.
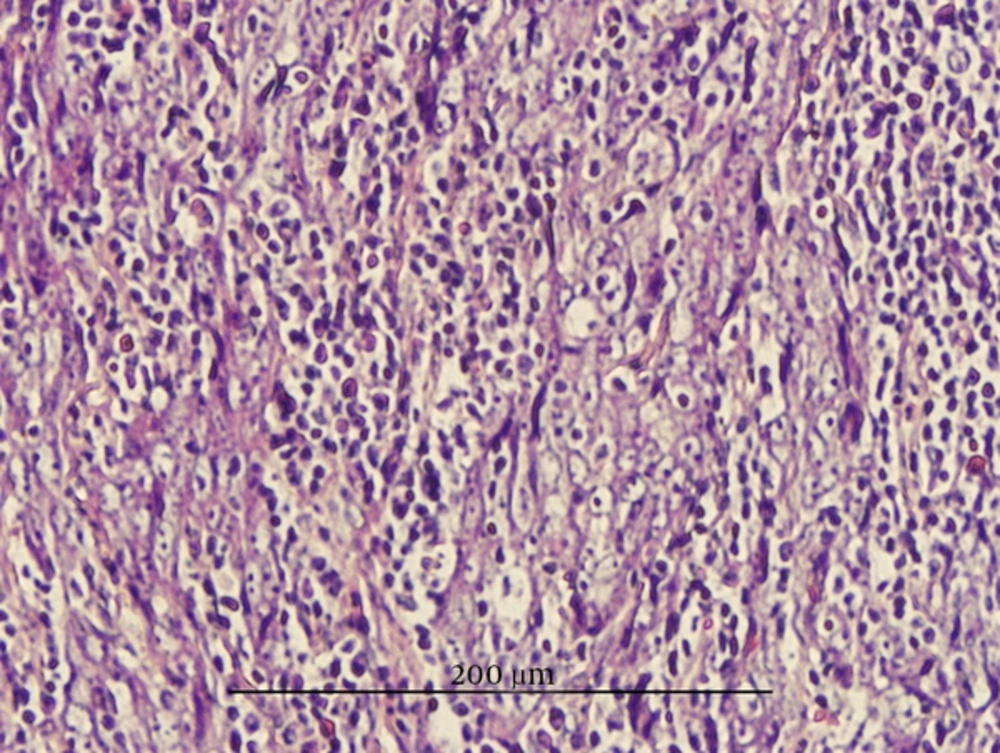
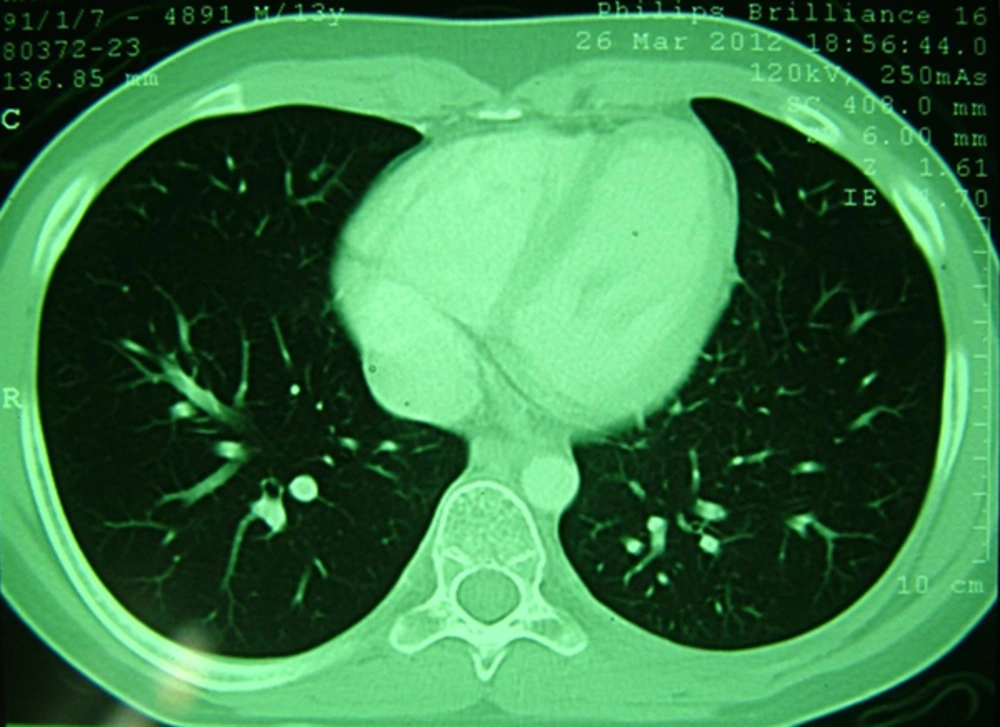
The patient received 70 Gy (2.0 Gy/fraction) radiotherapy in 27 sessions and chemotherapy with Taxotere for two sessions. The tumor size shrunk initially but grew back after one month, causing chest pain and shortness of breath in patient. The biopsy sample taken from mass has reassessed pathologically. The examinations have revealed multiple clusters of metastatic cells with vesicular nuclei and prominent nucleoli as well as median amount of non-keratinizing cytoplasm. The Non-keratinizing type (WHO type II) of nasopharyngeal carcinoma has confirmed (Figure 3). EBV RNA s markers have definite it. The patient has received new chemotherapy protocol of Cisplatin 100 mg/m2 intravenous on days 1, 22, and 43 accompanied with radiation, then cisplatin 80 mg/m2 intravenous (IV) on day 1 plus fluorouracil (5-FU) 1000 mg/m2/day by continuous intravenous infusion on days 1 - 4 every 4weeks for 3 cycles. After the second cycle, the mass has fully resolved in CT scan (Figure 4). Upon completion of the third cycle, the patient has received Interferon beta 105µg/kg/SQ 3 times a week for 6 months as additive therapy. During the maintenance therapy blisters have emerged on the patient’s face which have controlled with Clindamycin. Furthermore, three months after completion of the treatment, the patient has developed hypothyroidism with a TSH of 21.27 and underwent treatment with Levothyroxine. After one year of follow- up, the patient was in complete remission and had no particular complaint and was fine with heavy physical exercises. It hasn't given him shortness of breath or other signs anymore. CT scan of the neck, chest, and nasopharynx, in addition to abdominal sonography hasn’t shown any sign of relapse.
| Variable | Condition |
|---|---|
| CD20 | positive in lymphoid cells |
| CD3 | positive in lymphoid cells |
| Cytokeratin | positive in epithelial cell |
| CEA | negative |
| Thyroglobulin | negative |
| EMA | positive |
| CK | positive |
| LCA | negative |
| Ki 67 | positive |
. IHC Study from Specimen
| Variable | Condition |
|---|---|
| EBV-VCA IgG | 243 (positive) |
| EBV-VCA IgM | < 10 (negative) |
| Alpha-Fetoprotein | 2.4 |
| Beta HCG | negative |
| ESR | 68 |
| CBC | normal |
| LFT | normal |
| ALP | normal |
| LDH | normal |
Laboratory from the First Hospitalization
3. Discussion
Nasopharyngeal carcinoma has been rare among children accounting for 1-3% of all pediatric malignancies and 20 - 50% of all primary tumors in this age group. Moreover it has often presented in advanced stage (2). Our case was a 15 year-old male patient with nasopharyngeal carcinoma on the left side of the heart. Age, sex, geographic location and severity were identical to other reports while the site was ectopic. nasopharynx and neck were the most common primary site of Nasopharyngeal carcinoma. Although in this case no cervical involvement has found neither initially nor in the development of the disease (1-3). Lymphoepithelioma (WHO type III) has reported as the most common type of nasopharyngeal carcinoma in children. Our patient has diagnosed as non-keratinizing epidermoid (WHO type II) (9). This type of pathology was uncommon and had poorer response to treatment than Type III (2). Investigating EBV-VCA IgG In our patient has revealed strongly positive EBV infection. The result has confirmed the association of EBV in causing nasopharyngeal carcinoma (NPC), especially in non-keratinized type as other studies have highlighted as well (1, 2, 4, 5). The patient has not responded to the Initial radiotherapy. Thus, cisplatin-based chemotherapy administered to the patient and subsequently was followed by remission. Then, over the 6 months period, Patients received interferon as maintenance therapy. During one-year follow-up, the patient has sustained complete remission. The only complication was radiation-induced hypothyroidism. Response to treatment has caused enhanced recovery, reducing tumor size, and subsequently reducing radiation fields and dosage, hence it could reduce adverse effects of treatment particularly advanced stages, and type II (2, 6, 10).
3.1. Conclusions
Primary Nasopharyngeal carcinoma in children could occur in ectopic locations (e.g. around the heart). Early diagnosis has played an important role in the prognosis of the patient. Cisplatin-based Neoadjuvant chemotherapy, 5-fluorouracil (5-FU) and supportive therapy with interferon beta have appeared to be effective in the treatment of children with advanced NPC.