1. Background
Non-Hodgkin’s lymphomas (NHLs) are a heterogeneous group of malignancies of the lymphoid system (1, 2) and account for almost 3.4% of cancer deaths in the US (3). This disease is the fifth most frequently diagnosed cancer and its incidence has risen by at least 100% over the past five decades especially in Western countries (4). Based on WHO’s classification of hematological and lymphoid tumors, these diseases have been divided as B-and T-cell neoplasms. B-cell lymphomas account for approximately 90% of all lymphomas, and the 2 most common histological disease entities are follicular lymphoma and diffuse large B-cell lymphoma (DLBCL) (5). Compared with Western countries, high-grade NHLs are more prevalent in Iran (6). Expression of Ki-67, a nuclear antigen protein present in all cycling cells, is used to distinguish the growth fraction of tumors (7). General prognosis of NHL depends on various tumor and host-related factors including age of patients and performance status, histological subtype, grade and stage of lymphoma (8). Other risk factors are sex, race, primary or hereditary immune deficiency syndrome, autoimmune diseases such as Sjogren’s, Celiac disease, Rheumatoid arthritis, systematic Lupus Erythematosus, certain infections (such as EBV, HCV), genetic factors and family history of lymphoma in first-degree relatives (4). Rituximab is the monoclonal antibody responsible for all clinical improvement noted to date. The addition of this drug to cyclophosphamide, doxorubicin, vincristine, prednisone (R-CHOP) improves the response rate, progression-free survival (PFS) and overall survival (OS) in NHL, especially DLBCL (9).
2. Objectives
The aim of this study is to investigate Clinicopathology figures, OS and PFS in patients with NHL in Iran.
3. Methods
3.1. Patients
Between 2005 and 2014 in a descriptive study, 143 patients referred to Clinic of hematology in two centers. We checked age, sex, types and subtypes of NHL, recurrence, Ki-67, organomegaly, lymphadenopathy, radiotherapy, OS and PFS in the patients. The mean follow-up was 49 months and during this time, there was 32 deaths and 4 patients lost follow-up and were censored from our study. OS was defined from the date of diagnosis until death from any cause or the date of the last follow-up. PFS was defined as the time elapsed between treatment initiation and (3) tumor progression (growth of the tumor, new tumors, metastasis etc) (4) death from any cause or the date of the last follow-up, whichever came first, with censoring of patients who are lost to follow-up. All patients received R-CHOP regimen for 6 to 8 cycles.
3.2. Statistical Analysis
The curves of OS and PFS were plotted by GraphPad Prism 5 software. Date analysis was done by SPSS version 19 software.
4. Results
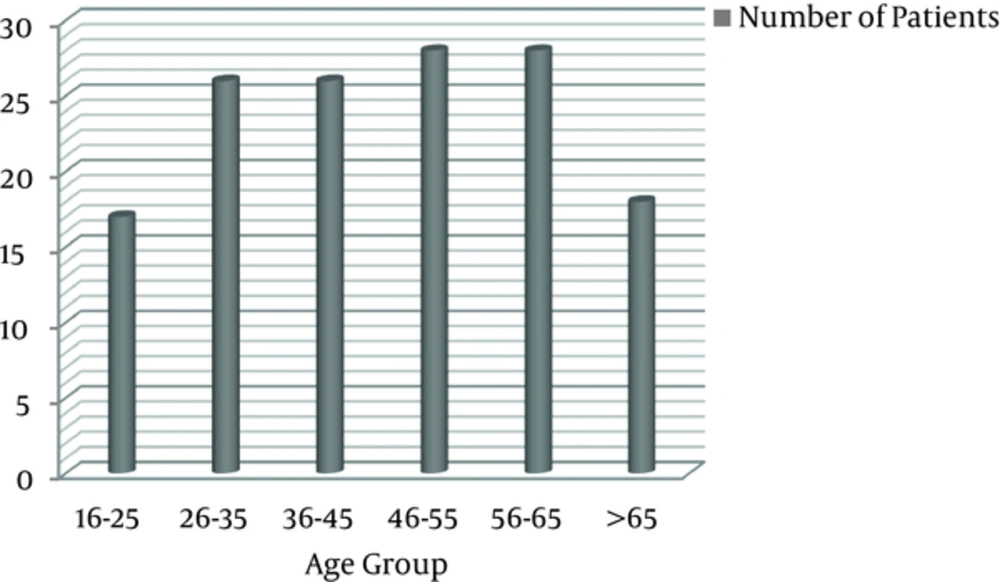
The median age at diagnosis for the patients was 46 ± 16 years (range, 16 - 82) that 110 patients (76.9%) had age < 60 years and 89 patients (62.2%) were male (Table 1). Eighty-three patients (58%) had primary nodal NHL and out of 139 patients, 123 patients (88.5%) were aggressive NHL. In follow-up time, 45 patients (31.5%) had recurrence. Out of 87 patients, Ki-67 < 65% was in 51 patients (58.6%). Organomegaly and lymphadenopathy were in12 patients (8.4%) and 80 (55.9%), respectively. Of all patients, 106 patients (74.1%) were treated with radiotherapy.
| Variables | Values |
|---|---|
| Age, year | 46 ± 16 (16 - 82) |
| Age group, year | |
| < 60 | 110 (76.9) |
| ≥ 60 | 33 (23.1) |
| Sex | |
| Male | 89 (62.2) |
| Female | 54 (37.8) |
| Type of primary NHL | |
| Nodal | 83 (58) |
| Extranodal | 60 (42) |
| Subtype of NHL | |
| Aggressive | 123 (88.5) |
| Indolent | 16 (11.5) |
| NA | 4 |
| Recurrence | |
| Yes | 45 (31.5) |
| No | 98 (68.5) |
| Ki-67 | |
| < 65% | 51 (58.6) |
| ≥ 65% | 36 (41.4) |
| NA | 56 |
| Organomegaly | |
| Yes | 12 (8.4) |
| No | 131 (91.6) |
| Lymphadenopathy | |
| Yes | 80 (55.9) |
| No | 63 (44.1) |
| Radiotherapy | |
| Yes | 106 (74.1) |
| No | 37 (25.9) |
Abbreviations: NA, not applicable; SD, standard deviation.
aValues are presented as No. (%) except age that is presented as (Mean ± SD).
Table 2 shows the correlation between the type of NHL and a number of variables in patients. There was just a significant correlation between lymphadenopathy with the type of NHL (P = 0.000). Therefore, lymphadenopathy was more in nodal NHL compared to extranodal NHL.
| Variables | Nodal, n = 83 | Extranodal, n = 60 | P Value |
|---|---|---|---|
| Age, years | |||
| Mean | 44.2 | 48.8 | 0.084 |
| <60 | 66 (79.5%) | 44 (73.3%) | 0.252 |
| Sex | |||
| Male | 48 (57.8%) | 41 (68.3%) | 0.135 |
| Subtype of primary NHL, n = 139 | |||
| Aggressive | 73 (89%) | 50 (87.7%) | 0.508 |
| Recurrence | |||
| Yes | 22 (26.5%) | 23 (38.3%) | 0.094 |
| Ki-67, n = 87 | |||
| < 65% | 30 (58.8%) | 21 (58.3%) | 0.569 |
| Organomegaly | |||
| Yes | 11 (12%) | 2 (3.3%) | 0.057 |
| Lymphadenopathy | |||
| Yes | 65 (78.3%) | 15 (25%) | 0.000 |
5. Discussion
The prevalence of all NHLs coded as being of extranodal origin is between 25% and 35% in most countries that stomach, skin and small intestine were the most common extranodal sites (10). The risk factor(s) of lymphoma has not been determined or clear yet (11). The most common types of lymphoma have originated from B cells (12). In a study (13), out of 77 patients with newly diagnosed primary NHL of the bone, 56 patients (72.7%) were male; the median age was 41.8 years, with a range of 16 - 84 years. In another study (14), among 387 NHL patients, the median age was 55 years with a male to female (M: F) ratio of 1.9:1. Naz et al. (15) reported that in NHL patients, 67% were male and M: F ratio was 2.6:1 with the mean age of 43.9 years (range, 6 to 80 years). In our study, the median age was 46 years, 62.2% male that M: F ratio was 1.7:1. Therefore, the percentage of NHL in males is more than females and the median age is around between 45 years.
In a research on NHL patients, the extranodal involvement was seen in 40.3% cases, while 59.7% cases showed nodal involvement (15). Padhi et al. (16) showed that primary extranodal constituted 22.0% of all NHLs. Also, Otter et al. (17) reported that primary extranodal lymphoma was 41% in their study. In this study, 58% patients had nodal NHL. Therefore, the prevalence of nodal is more than extranodal. A study (14) showed that in their patients with NHL, the aggressive histological subtypes predominate. Our study confirmed this result.
In a study in our area (18), 67.9% patients with NHL had Ki-67 < 60% that in our study, Ki-67 < 65% is 58.6%. The results of two studies are almost similar.
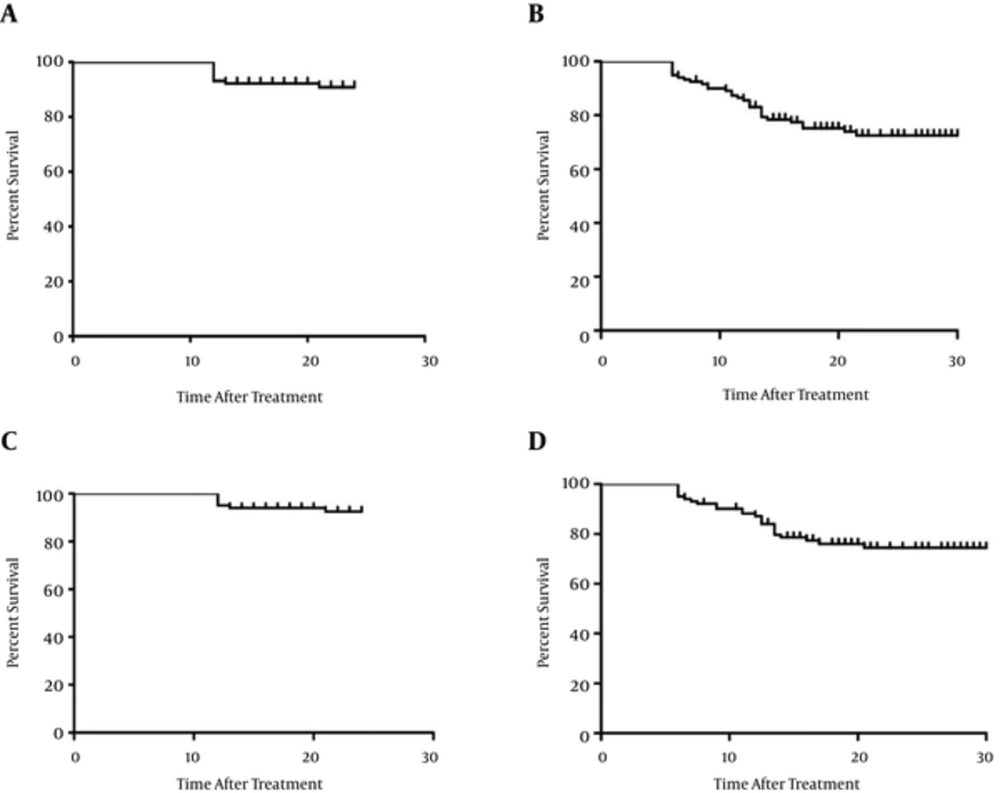
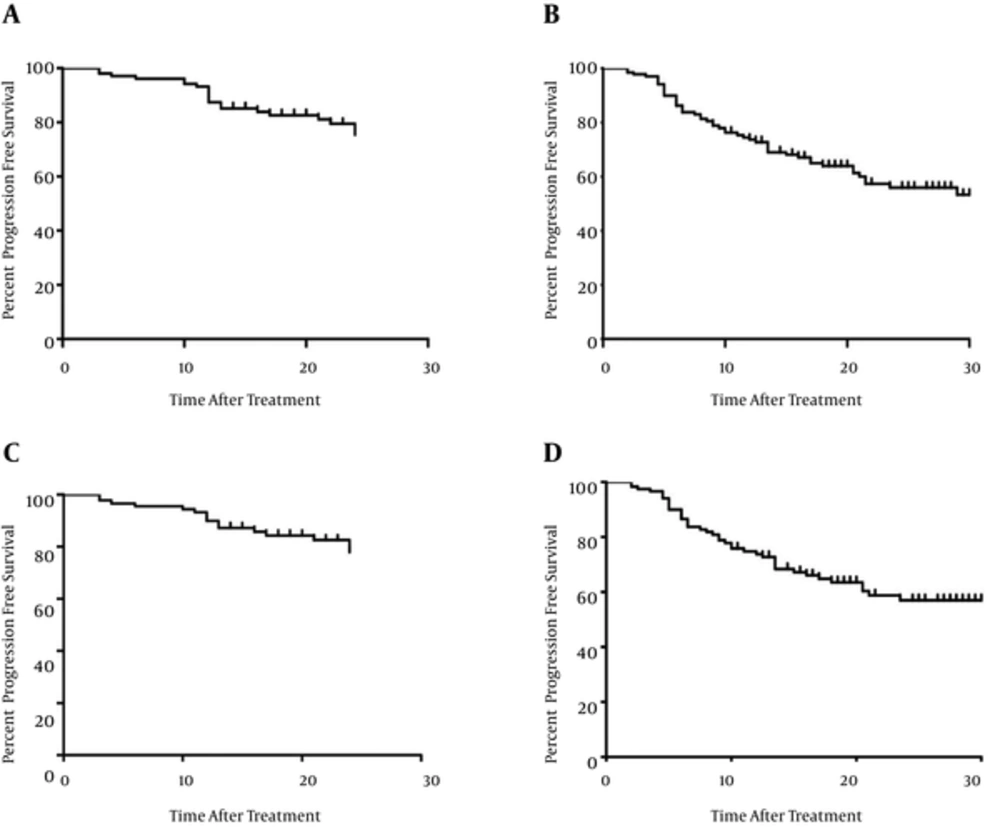
The 5-year OS rate and 5-year PFS rate were significantly higher in B-cell group than in T-cell group (69.5% vs. 35.5%, 53.3% vs. 28.9%) (19). In patients with DLBCL, The 5-year event-free survival was 61% for patients receiving chemotherapy alone and 64% for patients receiving CHOP plus radiotherapy; the 5-year OS were 72% and 68%, respectively (20). A study in primary gastric lymphoma patients showed that 5-year disease-free survival and OS rates were 60% and 70%, respectively (8). Hauptrock et al. (21) in 1666 treated patients with rituximab monotherapy, reported that median PFS was 23.5 months. Coiffier et al. (22) compared 8 cycles R-CHOP with CHOP in elderly patients with DLBCL resulted in a significant survival benefit for patients in the R-CHOP arm (OS 37 months). In a research on 2745 NHL patients (23), 2-year PFS for subtypes of DLBL was 64%, BL (Burkitt’s lymphoma) 56%, lymphoma intermediate between DLBL and BL 70%. Also, 2-year OS rates for DLBL was 76.9%, BL 56%, lymphoma intermediate between DLBL and BL 80%. Among patients of DLBL subgroup, 2-year PFS and OS according to different chemotherapy regimens were MCP-842 with 51% and 69.2%, CHOP: 65% and 80%, R-CHOP: 83.3%, and 88.7% (23). Another study (14) showed that 5-year OS rate was 65% for patients. Two studies in our area showed the 3-year, 5-year and 10-year OS rates for nodal NHL patients were 65%, 54.2% and 51%, respectively (24) and for extranodal were 70%, 62.2% and 60.8%, respectively (25). In our study that more patients treated with R-CHOP plus radiotherapy, 2-and 5-year OS rates for all patients were 91.5% and 85% and also 2-and 5-year PFS were 79.6% and 63.3%, respectively. Also, 2-and 5-year OS rates for aggressive NHL patients were 91% and 79.1%, respectively; whereas 2-and 5-year PFS were 79% and 63%, respectively. Therefore, the results show that treated patients with R-CHOP plus radiotherapy have better OS and PFS compared with other chemotherapy regimens. In the comparison between nodal and extranodal with other prognostic factors, lymphadenopathy was significantly more in nodal NHL.
5.1. Conclusions
Percentage of NHL in males is more than females and the median age of NHL patients is around 45 years. Also, the prevalence of nodal is more compared with extranodal in NHL patients.