1. Introduction
Pituitary adenoma (PA), a lesion arising from adenohypophysial cells, would be one of the most prevalent neuroendocrine intracranial tumors that accounted for 10% of all primary intracranial t111umors (1). Pituitary adenomas were usually benign lesions and less than 10 millimeters (mm). If they have grown to larger sizes they might result in compression with surrounding structures including cavernous sinus (2, 3). It has demonstrated that invasion of the cavernous sinus by tumors might lead to the compression and occlusion of the internal carotid artery (ICA) (4). The consequence of this event would be the presence of various clinical manifestations (4). On the other hand, the prevalence of pituitary adenomas has increased in the last few years (5). Some studies have also indicated the genetic predisposition of pituitary adenoma occurrence in individuals (6, 7). Despite huge pituitary tumors have reported as producer of stenosis or occlusion of the ICA, pituitary adenomas causing carotid compression of the ICA were rarely symptomatic (8-10). In addition, the incidence was extremely rare when there was no evidence of apoplectic event. To the best of our knowledge there was only one case report that has presented a patient with pituitary adenoma producing symptomatic carotid compression of the ICA without any apoplectic signs. In this case report we have described a 57 year old woman presenting with transient ischemic attacks (TIA) and a huge nonfunctional pituitary adenoma which produced symptomatic internal carotid occlusion. Patient has signed an informed consent for publishing data regarding her disease without her name divulged.
2. Case Presentation
A 57-year-old woman has referred to the neurology department of the Loghman Hakim hospital with complaints of sudden left hemiparesis involving her face and left extremities. She had an episode of transient hemiparesis one week before admission that lasts 12 hours. The patient has also suffered from disequilibrium, dizziness and vertigo. Physical examinations have revealed severe left hemiparesis [1/5]; mild left central facial paresis and bitemporal hemianopsis. Other neurologic examinations were normal. Patient's medical history was negative for cerebrovascular or cardiovascular diseases or other risk factors of stroke. She has declared no craniofacial trauma.
2.1. Diagnosis
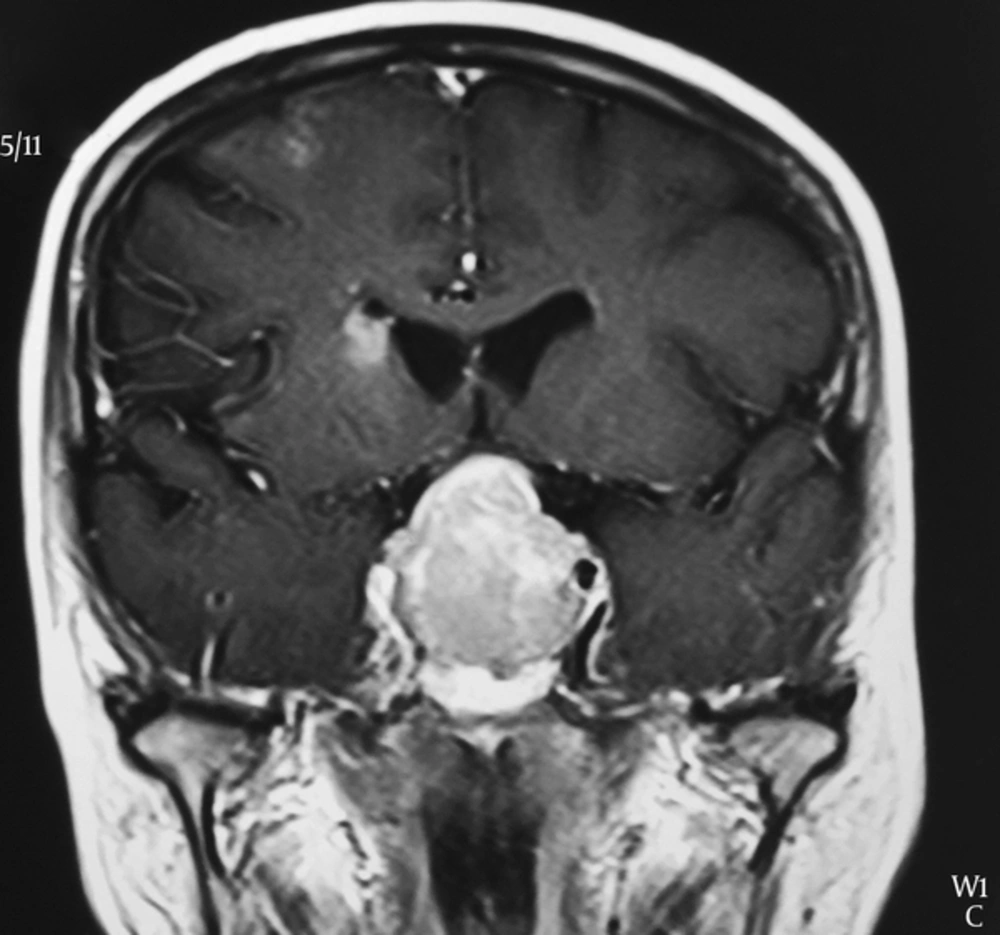
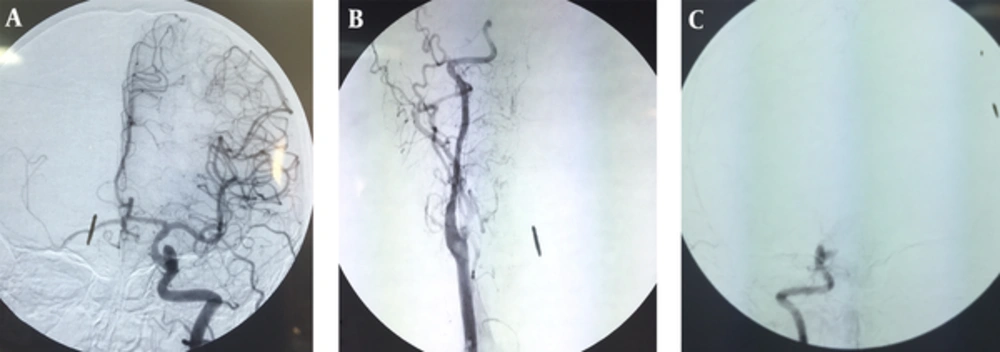
Magnetic resonance imaging (MRI) has revealed two distinct findings: high signal abnormality indicating ischemic injury in periventricular white matter and a huge sellar-suprasellar mass that has encased both of internal carotid arteries. After Gadolinium injection the mass has become heterogeneously enhanced and the right internal carotid artery has appeared to be occluded (Figure 1). Color doppler ultrasound sonography (CDUS) of carotid arteries and vertebral arteries has shown high resistance monophasic wave form with no retrograde flow in diastole in proximal part of right ICA. There was no significant plaque formation. These findings have suggested the presence of either occlusion or severe stenosis of internal carotid artery in distal region of right ICA. Spiral computed tomography (CT) scan of brain has revealed an intra sellar mass 31 × 21 mm. CT scan findings of the other areas were normal. Electrocardiogram and echocardiography have demonstrated no arrhythmia, valvular abnormality or vegetation. Digital subtraction angiography (DSA) has confirmed the occlusion in right internal carotid artery (Figure 2). She had high level of prolactin (threefold of normal limit) in laboratory investigation and other hormones were within normal limits.
2.2. Surgery
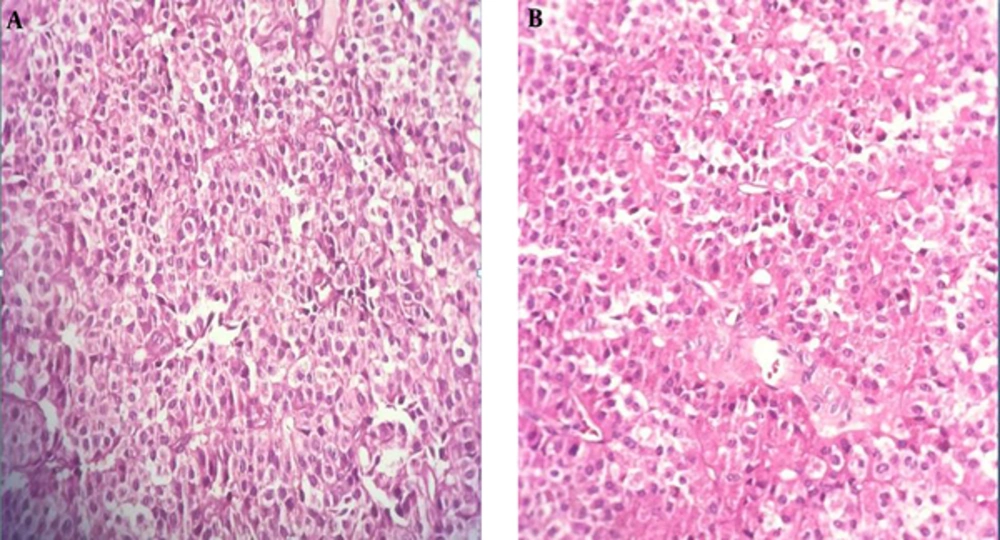
The patient has referred to our neurosurgery ward. She has undergone endonasal trans-sphenoidal surgery and the mass has resected. Sella has reconstructed as stage I according to Jalessi et al.’s (11) classification. Histopathologic examination has shown sheets of monomorphic polygona epithelial cells with amphophilic cytoplasms and round nuclei mostly in diffuse pattern with rare mitotic figures consistent with non-functional pituitary adenoma. No evidence of necrosis or hemorrhage has observed (Figure 1 A and B).
2.3. Post Operation
She has shown an uncomplicated post operation course and has discharged 6 days after surgery. Hemiparesis has improved with physiotherapy and other rehabilitation techniques during six month follow up.
3. Discussion
Pituitary adenoma was the third most common intracranial neoplasms (12). Approximately 40 percent of all pituitary adenomas were macroadenomas which their growth might invade suprasellar area, cavernous sinus and sphenoid sinus. Internal carotid occlusion in cavernous sinus region has numerously reported in the setting of pituitary apoplexy (13, 14). In addition, several studies have indicated that pituitary adenoma is an important precursor of pituitary apoplexy (15-18). Although cases of carotid arteries occlusion due to other intracranial lesions such as tumors (19) and huge aneurysms (20) have reported, compression and occlusion of ICA with pituitary adenoma were very rare especially in cases without apoplectic evidence. Molitch et al. (8) has evaluated the rate of internal carotid artery occlusion caused by pituitary adenomas. In their study 141 patients with cavernous sinus invasion have caused by different types of tumor have investigated. Eighty three patients had carotid artery encasement with 58 cases of them having pituitary adenoma. They have found that only one out of 58 cases (1.7%) has developed compression of the artery. This result has shown that pituitary adenoma producing internal carotid artery occlusion was extremely rare. In literature review we have found five case reports describing pituitary tumors producing carotid artery occlusion without the presence of apoplectic events (10, 21-24). Table 1 has summarized the details of these reports.
| Authors | Age/Gender | Clinical Manifestation | Tumor Size | Vascular Occlusion | Anatomical site of the Tumor | Treatment | Type of Adenoma |
|---|---|---|---|---|---|---|---|
| Yaghmai et al. 1996 (24) | 47/M | progressive loss of vision + severe headaches | 3 × 2.5-cm | supraclinoid portion of the right ICA | Area of the sella. and extended laterally toward both cavernous sinuses, | transsphenoidal resection | Non-functional |
| Spallone 1981 (10) | 55/F | TIA + left hemiplagia | Not mentioned | Right supracavernous ICA | Not mentioned | None | Not mentioned |
| Cavalcanti et al. 1997 (25) | 54/ F | Visual loss + right hemiparesis | Not mentioned | Narrowing of right supraclinoid ICA | sellar-suprasellar lesion | Craniotomy | Non-functional |
| Alentorn et al. 2011 (22) | 65/M | Acute aphasia Right hemiparesis | 4.2 × 3.3 × 4.2-cm | left internal carotid artery in the left cavernous sinus | macro adenoma in the pituitary region | endoscopic transsphenoidal subtotal resection | Non-functional |
| Rey-Dios et al. 2014 (23) | 48/M | TIA | Not mentioned | left ICA and severe stenosis of the right ICA at the level of the clinoid process | large pituitary adenoma encasing and narrowing both ICA | endonasal transsphenoidal resection | Not mentioned |
| This case | 57/F | TIA + left hemiparesis | 31 × 21 mm | internal carotid artery in distal region of right ICA | huge sellar-suprasellar mass that encased both of internal carotid arteries | endoscopic transsphenoidal subtotal resection | Non-functional |
The microscopic or endoscopic transsphenoidal surgery has emerged as the appropriate approach in cases with pituitary adenoma. In our case report the patient has presented with TIA without the evidence of apoplexy. Histopathologic findings has indicated that the tumor was a nonfunctional pituitary adenoma with no intra tumoral hemorrhage and no necrosis which was in consistent with lack of the apoplectic signs. Angiography in this case has confirmed the occlusion in right internal carotid artery that appears to be due to direct compression effect of the mass. Rey-Dios et al. (23) has reported a 48-year-old patient with right-hand weakness, left hemiparesis and blurred speech. He has experienced TIA which led to stroke. Further evaluation and MRI have revealed a huge pituitary adenoma causing direct compression and occlusion of the left ICA and excessive stenosis of the right ICA. Similar to our result there was no sign of apoplexy in this case. In the study by Spallone (10) three cases with internal carotid artery occlusion by intracranial tumors have reported. Two had meningioma and the other one had pituitary adenoma. The occlusion has confirmed with carotid angiography in all cases.
3.1. Conclusion
Pituitary adenomas causing symptomatic carotid compression of the ICA without any apoplexy event would be extremely rare. However, it might cause several clinical manifestations including TIA or stroke. If other causes for ischemic event have ruled out, urgent surgical procedure would be the best approach to prevent further complication in such patients.