1. Introduction
At present 15% to 30% of the cancers detected in mammography screening programs are DCIS, and the greatest increase in the incidence of DCIS has been seen in women aged 49 to 69 years. PT is an uncommon tumor of female breast and the average age at diagnosis is in the fourth decade. Phyllodes tumors are classified as benign, borderline, or malignant based on the nature of the tumor margins (pushing or infiltrative), presence of cellular atypia, mitotic activity, and over growth in the stroma. Clinically, phyllodes tumors are smooth, round, usually painless multinodular lesions that may be indistinguishable from fibroadenomas (1). PT, like fibroadenoma, arises from intralobular stroma. These lesions often have bulbous protrusions (phyllodesis Greek for leaf like) due to the presence of nodules of proliferating stroma covered by epithelium. Low grade lesions may contain mitotic images. High grade lesions may be difficult to distinguish from other soft tissue sarcomas and may have foci of mesenchymal differentiation (2).
Coexistence of PT and ductal carcinoma are extremely rare: often epithelial malignant lesion is invasive and DCIS is very unusual (3).
In this report, we have malignant alteration of epithelial component of PT in a 26 -year-old woman that is a rare phenomenon.
2. Case Report
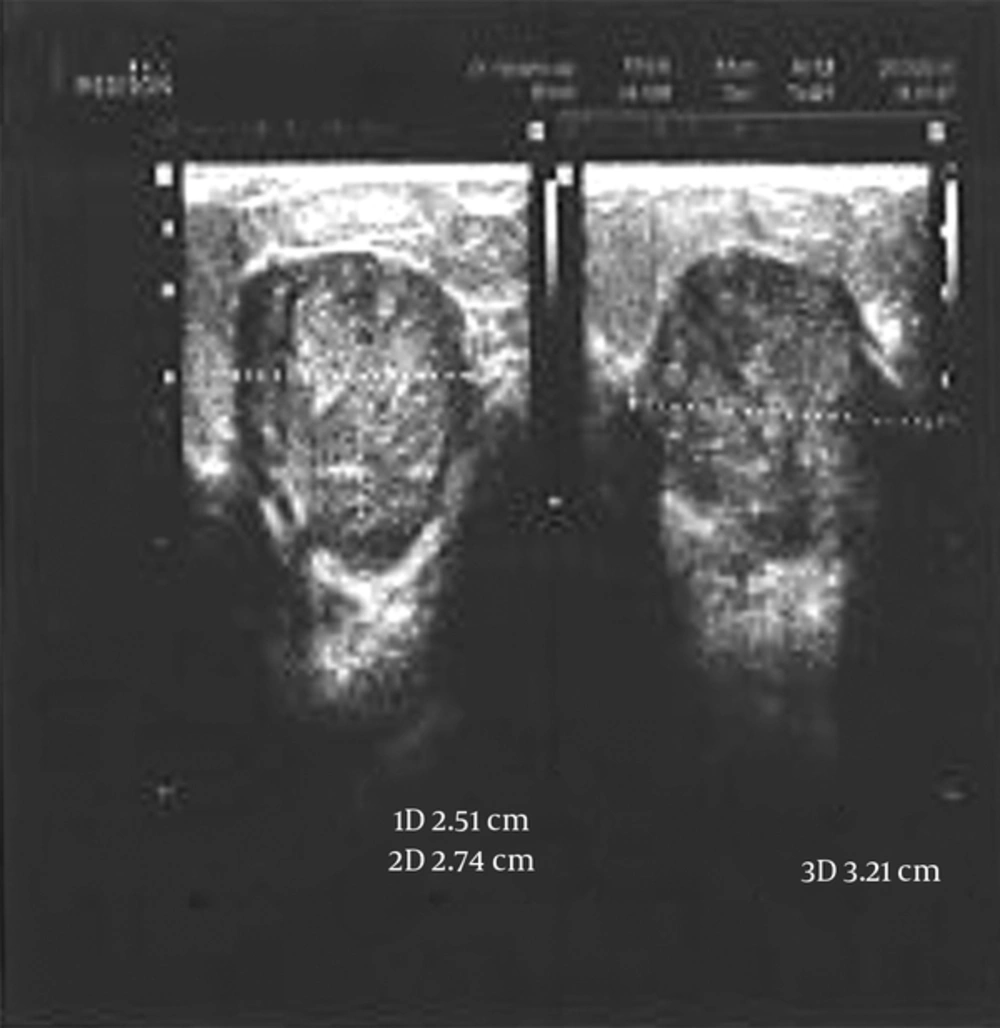
A 26 -year-old woman presented with a 2-cm nodule without any nipple changes and discharge. At first, she had noticed it about 3 months earlier. The tumor grew slowly over 3 months and then she visited a surgeon. Her family history was negative about existence of cancer in first and second degree relatives. On physical examination, the tumor did not have any adhesion to the skin and there was no palpable lymph node in the axillary or supraclavicular region. Ultrasound imaging showed a hypo echo mass, 26 × 28 × 32 mm in size, in the outer half of the left breast with regular border with clinical diagnosis of fibroadenoma. After 3 months, she visited her doctor again. Ultrasonography of the left breast mass was showing a 30 × 34 × 40 mm mass in 3 o’clock site with lobulated border and with regard to the increasing size and vascularity, biopsy was recommended. Excisional biopsy was performed and pathologic diagnosis of DCIS in benign PT was reported. After oncologic consultation considering both options of BCS and simple mastectomy, she selected simple mastectomy and reconstruction (Figure 1).
2.1. Pathological Findings
Grossly, the mass consisted of a cream relatively well circumscribed multilobulated mass measuring 4.5 × 3 × 3 cm. Cut surface was solid, gray white with cleft like spaces at periphery.
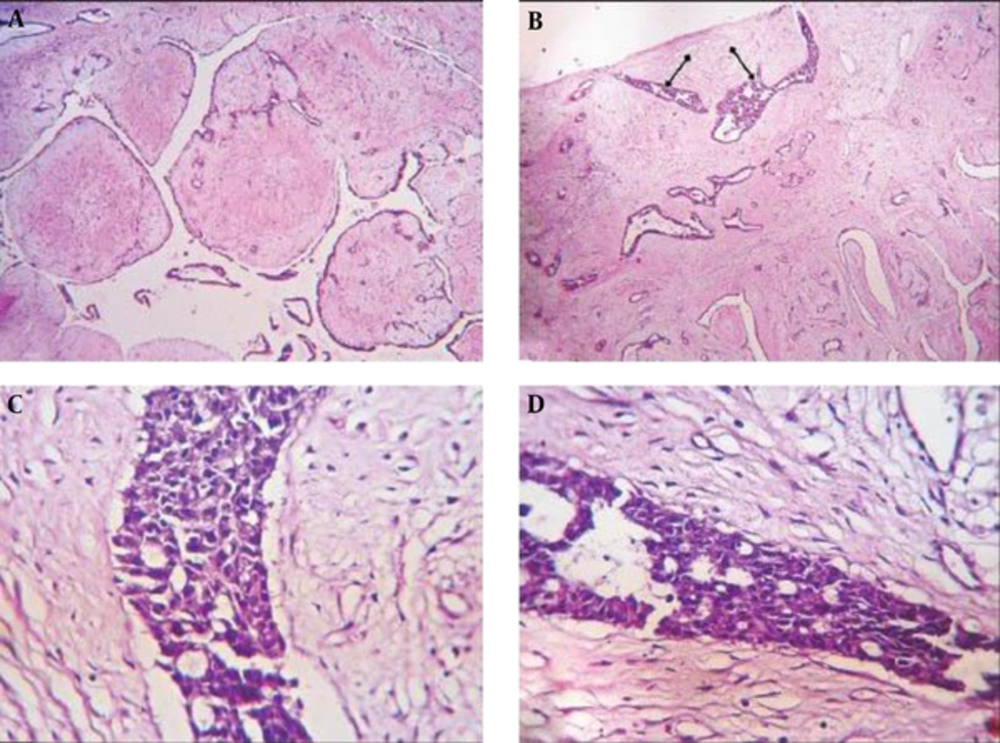
Histopathological examination demonstrated sections from breast mass that revealed biphasic neoplasm composed of both stromal and epithelial components. A moderately hyper-cellular stroma composed of spindle cells with mild to moderate pleomorphism and few mitotic activities (1-2/HPF) embedded in loose connective tissue were seen. Epithelial component represented foci of ductal hyperplasia, in solid, clinging and irregular cirbriform, with foci of central necrosis in few tubules. Epitelial cells showed moderate to severe pleomorphism, hyperchromatic nuclei, and atypical mitotic images. There was not any invasion. The final diagnosis was high grade (comedocarcinoma) DCIS of breast in benign PT (Figure 2).
A, a Microscopic View of the phyllodes Tumor with Cleft Like Epithelial and Benign Stromal Proliferation (HEx400); B, The Epithelial Component of the Phyllodes Tumor Showed Foci of Atypical Ductal Hyperplasia - DCIS (HEx100); C, A Microscopic View of Phyllodes Tumor with DCIS and Intraductal Atypical Cells (IHCx400); D, A Microscopic View of Phyllodes Tumor with DCIS (H&Ex1000).
3. Discussion
PT is a rare disease that is classified into benign, borderline, and high grade malignant tumors. The distinction among these three subgroups is based on the combination of histological characteristics of the tumors and also it is predictive of the probable clinical course (4).
The epithelial component of PT may show changes ranging from hyperplasia to invasive carcinoma. Sawyer et al. showed hyperplasia in the epithelial component of PT in 60%, and a moderate to strong overexpression of cyclin D1 in 46% of cases (5). Cyclin D1 is frequently overexpressed in breast cancer and DCIS (6, 7) but not in atypical ductal hyperplasia and other benign breast diseases. So it was unexpected to find such expression in the epithelium of benign tumors (8, 9).
As it was mentioned before, the median age of occurrence of phyllodes tumor is 40 - 50 years, and also ductal carcinoma in situ arising in phyllodes tumor is a rare situation, so our patient aged 26 years old was one of the youngest cases of benign PT with an arising DCIS in it that we have seen in documented literature.
According to a survey in literature, only one younger case of 19 years of age with DCIS arising in benign PT of breast has been reported before (10). Parfitt et al. reported a 26-year-old woman presented with a left breast mass and palpable lymph nodes in the left axilla. The pathologic study showed extensive high grade DCIS and invasive carcinoma of no special type, entirely located within the phyllodes tumor that subsequent axillary lymph node dissection revealed metastatic carcinoma (11).
Recently a case of PT with DCIS in a 42-year-old woman was reported from India (12). Yamaguchi et al. reported a 54- year- old postmenopausal woman with DCIS arising in benign PT with rapid overgrowth to 18 × 17 × 13 cm in size during 1 year. Simple mastectomy was done for her and tamoxifen was prescribed and after 1 year, she had remained well (3).
Nio et al. reported another case with DCIS and PT in a 53-year-old female who received a local excision with a margin of 1 cm from the tumor edge, and because of multiple recurrence of PT local irradiation at a total dose of 50 Gy was prescribed (13).
We managed our patient with simple mastectomy and reconstruction. Different types of managements have been performed for benign PT with DCIS. Local managements include simple mastectomy or partial mastectomy with or without adjuvant radiotherapy. Endocrine therapy with tamoxifen depending on the estrogen/progesterone receptors status of DCIS component has been recommended by some authors. According to the literature, it seems there is not any preferred management for this combined lesion because of its rarity and common treatment approach is on the basis of surgeon and patient decision. All mentioned ways have satisfactory results in the short term run; however, more investigation on long term outcomes is necessary.
Diagnosis of DCIS within a PT before surgery is impossible. Pathologist should be aware of the possibility of existence of carcinoma within a PT even in young people like our patient and investigate malignancy in the epithelial component like stroma.
We reported this case after obtaining her witten consent.