1. Background
Heavy menstrual bleeding is a common problem in women (1). Post-menopausal bleeding that occurs 1 year after the permanent cessation of menstruation is considered abnormal and must be examined (2, 3). Abnormal uterine bleeding, which is very common among post-menopausal women, is an important symptom of both benign and malignant diseases in women (4, 5). The chance of endometrial cancer is about 10% in women with post-menopausal bleeding (6). More than 90% of post-menopausal women with endometrial cancer have vaginal bleeding, with benign causes in most cases, such as genital atrophy and endometrial polyp (7-9). The risk of endometrial cancer is highly varying in post-menopausal women presenting with vaginal bleeding; the incidence of malignancy ranges from 1% to 24%, depending on the study population and the presence of cancer risk factors (10-14). The early detection of the cause of post-menopausal bleeding is necessary even in mild and non-continuous bleeding; however, there is no consensus on a proper diagnostic method (15). Common diagnostic methods of vaginal bleeding include transvaginal ultrasound and endometrial biopsy, but each of these methods have their disadvantages (16). Transvaginal ultrasound is a safe non-invasive method for examining endometrial thickness and problems in the other pelvic organs (17). Endometrial biopsy should be performed only for endometrial thicknesses over 4 mm as observed in the transvaginal ultrasound (16). One of the major limitations of this method is its high rate of false negative and false positive cases in local intrauterine pathologies (18-20). Cooper conducted a study to compare the cost-effectiveness of methods such as transvaginal ultrasound, endometrial biopsy, saline infusion, sonohysterography, and outpatient hysteroscopy in abnormal uterus bleeding diagnoses. The results of the study revealed outpatient hysteroscopy to be a good first-line diagnostic approach for women, who like to preserve their uterus and fertility. Women with post-menopausal bleeding and an endometrial thickness over 5 mm need to undergo diagnostic strategies other than transvaginal ultrasound (21).
Clark et al. examined diagnostic methods such as endometrial biopsy, transvaginal ultrasound, and hysteroscopy to find the most cost-effective method for post-menopausal women with abnormal vaginal bleeding. A decision-making analysis framework was modeled; the consequences and cost of each method were investigated and a sensitivity analysis was also carried out. Transvaginal ultrasound and endometrial biopsy were ultimately found to be the most cost-effective methods. Hysteroscopy was not cost-effective either separately or in combination with the other methods (3). Some models were also proposed based on patients’ clinical profile in order to predict the risk of endometrial cancer in post-menopausal patients with bleeding (3, 22). The results obtained in a study conducted by Bruchim et al. in 2004 showed that invasive methods can be avoided by 60% in the diagnosis of endometrial cancer if the time of menopause and endometrial thickness are both identified (23).
Given the prevalence of abnormal post-menopausal bleeding, the importance of the timely diagnosis of the condition for the early detection of malignancies, and the many studies conducted on the use of bleeding patterns and endometrial thickness in transvaginal ultrasound as a diagnostic method for abnormal uterus bleeding (3, 17, 20, 24), the present study was conducted to investigate the relationship of post-menopausal bleeding patterns and endometrial thickness as observed in the transvaginal ultrasound with uterine pathologies and, thus, to offer predictive models for endometrial cancer.
2. Methods
The present descriptive-analytical cross sectional study was conducted on post-menopausal women with vaginal bleeding presenting to Ayatollah Rouhani Hospital in Babol, Iran, between May 2014 and May 2015. The research was approved by the ethics committee of Babol University of Medical Sciences (MUBABOL.REC.1393.11). All the participants provided written consents.
The subjects were selected through convenience sampling method. The inclusion criteria consisted of having had amenorrhea for at least 12 months, not receiving estrogen hormone replacement therapy, and lacking congenital uterine anomalies resulting from the abnormal formation, fusion, or resorption of the Müllerian ducts during fetal life (as per the patient’s history). The exclusion criteria consisted of the impossibility of undergoing an endometrial biopsy (such as cervical stenosis), the patient’s failure to return after sampling, and known malignancies in other organs. The research was approved by the ethics committee of the University and the subjects were ensured of the confidentiality of their information in accordance with the principles of the Helsinki declaration. After providing written consent forms, the patients underwent a transvaginal ultrasound and endometrial biopsy by a gynecologist through curettage. The patients who had a focal lesion in their ultrasound underwent hysteroscopy. The samples taken were sent to Ayatollah Rouhani hospital for pathological examination and the results were recorded in the patients’ medical records. The patients’ standing height was measured barefoot with a stadiometer; their weight was also measured barefoot and with minimal clothing, using a scale (precision: 0.1 kg).
The data recorded included the subjects’ personal information, age, duration of menopause, BMI, parity, gravidity, disease history, and medication history. In order to differentiate between single-episode and recurrent-episode bleeding, the patients were asked about their number of bleeding episodes. They were also asked about the number of sanitary pads they used daily to find their frequency and amount of bleeding. Abnormal bleeding was divided into 3 categories: A) Spotting: If bleeding lasted for only 1 day and the patient used only 1 sanitary pad; B) Mild: If bleeding lasted for only 1 day but more than 1 sanitary pad was used or if bleeding lasted for more than 1 day and a single sanitary pad was used; C) Severe: If bleeding lasted for more than 1 day and more than 1 sanitary pad was used daily. The number of sanitary pads per day was used to quantify the bleeding amount such that the number of bleeding days was multiplied by the number of pads used (3).
To determine the optimal predictors of endometrial cancer, the logistic regression model was used in this study for defining 3 models, namely AM30, AMD30, and AMDI30.
In the AM30 model, A and M represent the amount of bleeding and menopause age while number 30 is used for BMI. The total AM30 score is the sum of the scores for the different clinical characteristics; mild or severe bleeding in the patient is assigned a score of 4, menopause ages of at least 58 are assigned a score of 2 and a BMI of at least 30 kg/m2 is assigned a score of 1. If one criterion is not present, the score will be 0. The total score for the AM30 model ranges between 0 and 7.
In the AMD30 model, besides the amount of bleeding, menopause age and BMI, the patient’s diabetes history is also considered and represented by D. If the patient suffers from diabetes, the score will be 2; otherwise, it will be 0. The total score for the AMD30 model varies between 0 and 9.
The AMI30 model is defined by adding I to the AM30 model to represent internal diseases. If the patient suffers from thyroid diseases, hypertension or diabetes, the score will equal 2, but if none of these diseases exist, the score will be 0. The total score for this model varies between 0 and 9.
2.1. Sample Size
The study subjects were selected, using the census method and Daniel’s formula was used to estimate the sample size as follows:

Z: normal distribution percentile
d: confidence interval
P: probability
Studies have reported a prevalence (p) of 10% for endometrial cancer (25). Considering a test power of 80, a significance level of α = 0.05, Z = 1.96 and d = 0.07, a minimum of 72 subjects were needed for this study (n = 72).
2.2. Data Analysis
SPSS-16 and STATA-12 and MedCalc software were used to analyze the data. The mean and standard deviation (SD) were used to report the quantitative variables; frequency and percentage were used for the qualitative variables. Pearson’s correlation coefficient was used to investigate the relationship between the quantitative variables, while χ2 and Fisher’s exact test (if necessary) were used to examine the relationship between the qualitative variables. The independent t test and the one-way ANOVA were used to compare the quantitative variables in double and multiple groups, respectively. To find the relationship of the personal and clinical variables with endometrial cancer and determine the optimal predictive model for endometrial cancer, the logistic regression model and ROC curve analysis were used. P values less than 0.05 were considered statistically significant.
3. Results
Of the 117 patients examined, 5 were excluded, as 4 of whom did not present after the sampling stage and 1 could not undergo biopsy. The data of 112 patients were ultimately analyzed. The mean age of the patients was 63.1 ± 8.3 years, their mean menopause age was 55.6 ± 5.1, and their mean duration of menopause was 7.4 ± 6 years. All the patients were married and their mean BMI was 28.7 ± 5.5.
A total of 31 patients (27.7%) experienced spotting, 77 (68.8%) experienced mild bleeding, and 4 (3.6%) experienced severe bleeding. The pathological examination of the samples revealed endometrial polyps in 51 patients (45.54%) and revealed this condition to be the most common cause of bleeding, followed by endometrial atrophy in 39 patients (34.82%), endometrial cancer in 14 (12.5%), and endometrial hyperplasia in 8 (7.14%). Of the 14 cases of cancer reported in the pathology examination, 11 had adenocarcinomas, 2 had carcinosarcomas, and 1 had endometrial serous carcinoma.
Table 1 presents the demographic details, bleeding patterns, and transvaginal ultrasound results (uterine size and endometrial thickness) of the post-menopausal women with vaginal bleeding divided into 2 groups, including patients with and patients without endometrial cancer (as per their pathological results). The group with endometrial cancer had a significantly higher mean age (P = 0.008), menopause age (P = 0.004), BMI (P = 0.007), and amount of bleeding (P<0.001), although higher cases of recurrent bleeding were observed in the group without cancer. In addition, the ultrasounds reported that the mean endometrial thickness was higher in the women with endometrial cancer compared to in those without cancer (13.3 ± 5.3 mm versus 8.9 ± 7.5 mm), and the difference was statistically significant (P = 0.04). As for internal diseases in the patients with cancer, 4 subjects (28.6%) had HTN (Hypertension), 6 (42.9%) had diabetes, and 1 (7.1%) had thyroid disease; in the patients without cancer, 16 (16.3%) had HTN, 18 (18.4%) diabetes, and 9 (9.2%) thyroid disease.
| Variable | Patients with Cancer (N = 14) | Patients without Cancer (N = 98) | P Value |
|---|---|---|---|
| Age, y | 66.7 ± 3.6 | 62.5 ± 8.6 | 0.008* |
| Body mass index (BMI), kg/m2 | 32.4 ± 5.2 | 28.2 ± 5.4 | 0.007* |
| Menopause age, y | 59.2 ± 3.6 | 55.1 ± 5.1 | 0.004* |
| Bleeding index (number of pads*number of days) | 43.2 ± 93.2 | 12.1 ± 22.2 | 0.005* |
| Frequency of bleeding episodes, % | 0.05 | ||
| Single | 11 (78.6) | 92 (93.9) | |
| Recurrent | 3 (21.4) | 6 (6.1) | |
| Amount of bleeding | < 0.001* | ||
| Spotting | 1 (7.1) | 30 (30.6) | |
| Mild | 10 (71.4) | 67 (68.4) | |
| Severe | 3 (21.4) | 1 (0.01) | |
| Frequency of internal diseases | 11 (78.6) | 43 (43.9) | 0.02* |
| Frequency of cesarean deliveries, % | 1 (7.1) | 21 (21.4%) | 0.2 |
| Uterine size, mm | 89.2 ± 21.4 | 88.8 ± 21.4 | 0.7 |
| Endometrial thickness, mm | 13.3 ± 5.3 | 8.9 ± 7.5 | 0.04* |
aValues are expressed as mean ± SD or No. (%).
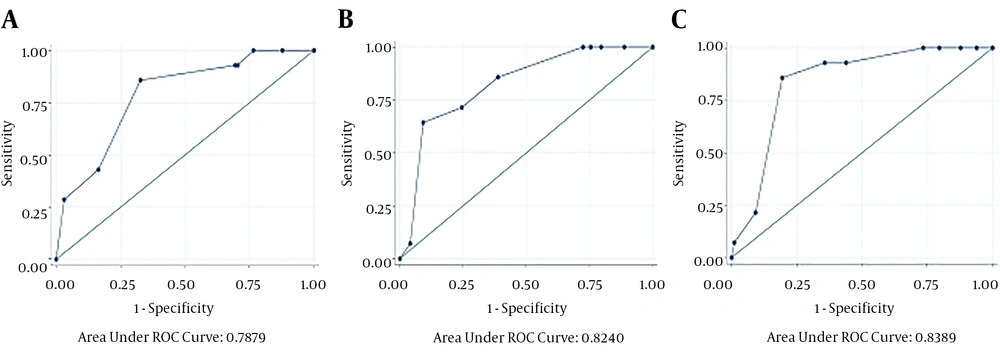
According to the multivariate logistic regression analysis of the AM30 diagnostic model, menopause age (OR = 5.03 and criterion = 2.36) and BMI (OR = 8.00 and criterion = 2.97) were significantly effective variables (P < 0.05), while amount of bleeding (OR = 6.07 and criterion = 1.65) was not a significant variable at the 0.05 level, although it was a significant variable at the 0.1 level (Table 2). The sensitivity, specificity, accuracy, LR (likelihood ratio) (+), LR (-), and d-or of the AM30 diagnostic model were also measured. The optimal cut-off point for this model is, therefore 5, in which the model sensitivity was 85.71% and its specificity and accuracy were 67.35% and 69.67%. According to Figure 1A, the area under the ROC curve was 0.7879, which is deemed favorable, given the number of samples with and without the cancer.
| Cut-Off Point | Sensitivity, % | Specificity, % | Correctly Classified, % | LR(+) | LR(-) | d-OR |
|---|---|---|---|---|---|---|
| (≥ 0) | 100 | 0.00 | 12.50 | 1.00 | - | - |
| (≥ 1) | 100 | 12.24 | 23.21 | 1.13 | 0.00 | - |
| (≥ 2) | 100 | 23.47 | 33.04 | 1.30 | 0.00 | - |
| (≥ 3) | 92.86 | 29.59 | 37.50 | 1.31 | 0.24 | 5.45 |
| (≥ 4) | 92.86 | 30.61 | 38.39 | 1.33 | 0.23 | 5.78 |
| (≥ 5) | 85.71 | 67.35 | 69.64 | 2.62 | 0.21 | 12.47 |
| (≥ 6) | 42.86 | 83.67 | 78.57 | 2.62 | 0.68 | 3.85 |
| (≥ 7) | 28.57 | 96.94 | 88.39 | 9.33 | 0.73 | 12.78 |
| (> 7) | 0.00 | 100 | 87.50 | - | 1.00 | - |
Abbreviations: LR, likelihood ratio; OR, odd ratio.
According to the multivariate logistic regression analysis of the AMD30 diagnostic model, menopause age (OR = 6.64 and criterion = 2.55) and BMI (OR = 12.45 and criterion = 3.13) were significantly effective variables (P < 0.05), while amount of bleeding (OR = 7.14 and criterion = 1.77) was not a significant variable at the 0.05 level; however, diabetes (OR = 6.00 and criterion = 2.44) was also a significant variable (P < 0.05). According to Table 3, the optimal cut-off point for this model was 6, with a sensitivity of 71.43%, specificity of 75.51% and accuracy of 75%. According to Figure 1B, the area under the ROC curve was 0.8240, which is deemed favorable, given the number of samples with and without the cancer.
| Cut-Off Point | Sensitivity, % | Specificity,% | Correctly Classified, % | LR(+) | LR(-) | d-OR |
|---|---|---|---|---|---|---|
| (≥ 0) | 100 | 0.00 | 12.50 | 1 | - | - |
| (≥ 1) | 100 | 11.22 | 22.32 | 1.12 | 0.00 | - |
| (≥ 2) | 100 | 20.41 | 30.36 | 1.25 | 0.00 | - |
| (≥ 3) | 100 | 24.49 | 33.93 | 1.32 | 0.00 | - |
| (≥ 4) | 100 | 27.55 | 36.61 | 1.38 | 0.00 | - |
| (≥ 5) | 85.71 | 61.22 | 64.29 | 2.21 | .23 | 9.60 |
| (≥ 6) | 71.43 | 75.51 | 75.00 | 2.91 | 0.37 | 7.86 |
| (≥ 7) | 64.29 | 90.82 | 87.50 | 7.00 | 0.39 | 17.94 |
| (≥ 8) | 7.14 | 95.92 | 84.82 | 1.75 | 0.96 | 1.82 |
| (> 8) | 0.00 | 100 | 87.50 | - | 1.00 | - |
Abbreviations: LR, likelihood ratio; OR, odd ratio.
According to the multivariate logistic regression analysis of the AMI30 diagnostic model, menopause age (OR = 8.64 and criterion = 2.49), and BMI (OR = 13.50 and criterion = 2.91) were significantly effective variables (P < 0.05), while the amount of bleeding (OR = 5.88 and criterion = 1.62) was not significant at the 0.05 level; however, internal diseases (OR = 8.29 and criterion = 2.38) also comprised a significant variable (P < 0.05). The optimal cut-off point for this model was 7, with a sensitivity of 85.71%, specificity of 80.61%, and x accuracy of 81.25% (Table 4). According to Figure 1C, the area under the ROC curve was 0.8389.
| Cut-Off Point | Sensitivity, % | Specificity, % | Correctly Classified, % | LR(+) | LR(-) | d-OR |
|---|---|---|---|---|---|---|
| (≥ 0) | 100 | 0.00 | 12.50 | 1.00 | - | - |
| (≥ 1) | 100 | 6.12 | 17.86 | 1.06 | 0.00 | - |
| (≥ 2) | 100 | 12.24 | 23.21 | 1.13 | 0.00 | - |
| (≥ 3) | 100 | 20.41 | 30.36 | 1.25 | 0.00 | - |
| (≥ 4) | 100 | 26.53 | 35.71 | 1.36 | 0.00 | - |
| (≥ 5) | 92.86 | 56.12 | 60.71 | 2.11 | 0.12 | 17.58 |
| (≥ 6) | 92.86 | 64.29 | 67.86 | 2.60 | 0.11 | 23.63 |
| (≥ 7) | 85.71 | 80.61 | 81.25 | 4.42 | 0.17 | 26 |
| (≥ 8) | 21.43 | 90.82 | 82.14 | 2.33 | 0.86 | 2.70 |
| (≥ 9) | 7.14 | 98.98 | 87.50 | 7.00 | 0.93 | 7.52 |
| (> 9) | 0.00 | 100 | 87.50 | - | 1.00 | - |
Abbreviations: LR, likelihood ratio; OR, odd ratio.
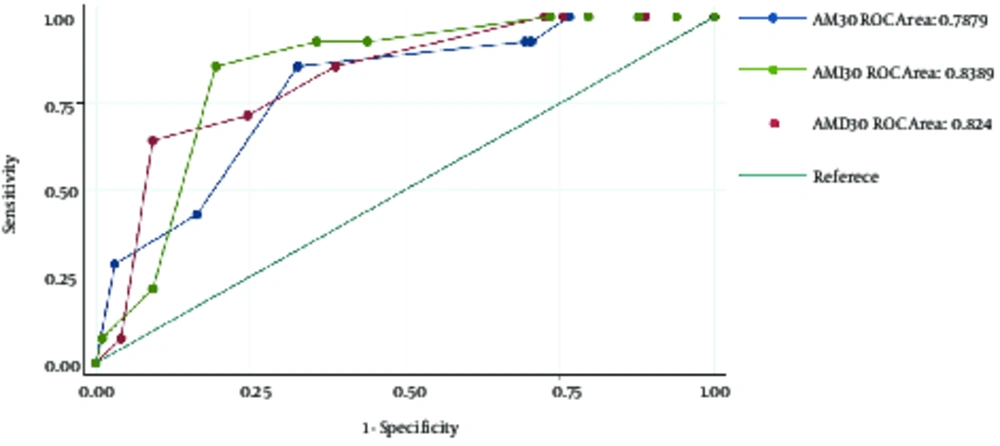
AMI30 was thus found to be the best predictive model in this study, as it had the highest area under the ROC curve, although there were no statistically significant differences between these 3 models (P = 0.29) (Figure 2).
4. Discussion
Early examination is crucial for the detection of malignancies in post-menopausal women with vaginal bleeding. Currently, there are some diagnostic models available for classifying post-menopausal patients with vaginal bleeding and predicting their probability of endometrial cancer; however, not all healthcare providers agree on their use. The findings of this study showed that BMI, menopause age, amount of bleeding, and history of internal diseases can significantly predict the incidence of endometrial cancer in post-menopausal women with abnormal uterus bleeding. Three models were introduced for predicting endometrial cancer in these women. The best predictive model was AMI30, which had the highest area under the ROC curve.
A study was showed that endometrial carcinoma is associated with higher age, higher BMI, longer duration of menopause, higher amount of bleeding, and recurrent bleeding (25), which is consistent with the present findings. Another study examined the risk of endometrial cancer based on bleeding patterns and concluded that endometrial cancer is more prevalent in patients with a higher age, higher BMI, longer duration of menopause, and recurrent bleeding episodes (24). Similarly, in a study conducted in the Netherlands, history of recurrent bleeding was found to be a predictor of endometrial cancer (26). Although the present study found more frequent cases of recurrent bleeding in the group without cancer, severe bleeding was more prevalent in the cancer group, who experienced higher amounts of bleeding (P < 0.001).
The authors recommended endometrial biopsy in post-menopausal women, especially in those aged over 60 with endometrial bleeding and an endometrial thickness of less than 3 mm (27). A meta-analysis showed that transvaginal ultrasound cannot eliminate the need for invasive diagnostic methods in women (20). In the present study, all the post-menopausal women with endometrial cancer and vaginal bleeding had an endometrial thickness equal to or greater than 5 mm in the transvaginal ultrasound.
In another study in the UK, the FAD31 model was presented, with F representing the frequency of menstrual bleeding, A the patient’s age, D the patient’s diabetes history, and 31 her BMI of at least 31. The total FAD31 score ranged between 0 and 8. With a cut-off point of at least 4, the model sensitivity and specificity were reported as 80% and 51%. A BMI higher than 31 correlated significantly with an increased risk of malignancy in post-menopausal women with vaginal bleeding (24). In the present study, the researchers used the FAD31 model with a cut-off point of at least 4 and found an area under the ROC curve of 0.621 and the model was found to be able to predict endometrial cancer with a sensitivity of 78.57% and a specificity of 6.12%; therefore, it is considered a weaker predictor compared to the models proposed in this study. With a cut-off point of at least 6, FAD31 had a sensitivity of 50% and specificity of 78.57%. The AM30, AMD30, and AMI30 models proposed in this study, thus, offer a higher sensitivity, specificity, and area under the ROC curve with the defined cut-off points.
Another study conducted in the UK compared the DEFAB model with the DFAB model. Variables such as diabetes, endometrial thickness of at least 14 mm, frequency of episodes of recurrent bleeding, age over 64, and BMI of 31 and over were included in the DEFAB model, while endometrial thickness was excluded from the DFAB model. With a cut-off point of at least 3, the DEFAB model offered a sensitivity of 85.9% and a specificity of 48.4%; with a cut-off point of at least 4, the DFAB model yielded a sensitivity of 81.8% and a specificity of 50.8%. No statistically significant differences were ultimately observed in the two models in terms of sensitivity, specificity, and positive and negative predictive values. Both of these models could, therefore, be used to predict the risk of endometrial malignancy (28). The researchers of the present study also used the DEFAB model with a cut-off point of at least 3 and found the area under the curve to be 0.6611 and the model sensitivity and specificity to be 100% and 10.5%; even with a cut-off point of at least 6, a sensitivity of 64% and a specificity of 70% were reported as the best predictive power of the model, which is still considered weak compared to the predictive power of the models offered by the present researchers.
A study in Italy proposed the RHEA model, which consists of variables such as recurrent bleeding episodes, hypertension, endometrial thickness over 8 mm, and age over 65. With a cut-off point of at least 4, the sensitivity was reported as 87.5% and specificity as 80% (29). The researchers of this study also used this model and found a sensitivity of 78.57% and a specificity of 35.71% and an area under the curve of 0.624 for a cut-off point of at least 4, while the sensitivity and specificity were 57.14% and 67.35% for a cut-off point of at least 5 as the best predictive power of the model. All the models proposed in the present study are, therefore, better than this model in terms of their predictive power.
Although different risk factors have been proposed in the cited studies, the majority have also examined age, internal diseases (diabetes and hypertension), and BMI. The present study found a more significant relationship between menopause age and the prevalence of endometrial cancer. The low sensitivity and specificity obtained for the FAD31, DEFAB, DFAB, and RHEA models in the present study is probably caused by the smaller sample size used compared to the papers cited (24, 28, 29). All the 3 models proposed in the present study had a good area under the curve and sensitivity and specificity; however, the AMI30 model was the best in terms of the area under the curve.
If the AMI30 score is less than 7 in women with post-menopausal bleeding, non-urgent transvaginal ultrasound is recommended for assessing endometrial thickness (ET). If ET < 5 mm, there is no need for further investigation or hospital admission, but if ET ≥ 5 mm, then, hospital admission for endometrial sampling is recommended. Women with AMI30 scores of 7 or higher should undergo endometrial biopsy.
This study was conducted in a single center, which can be considered a limitation, because the results obtained may not be easily generalizable due to the likelihood of bias caused by the more uniform study population. Another limitation of the study is its small sample size. Future studies are recommended to be conducted on larger sample sizes for validating this model. The prevalence of endometrial cancer observed in the group of women assessed in this study can be taken to indicate the general scenario in primary healthcare settings.
The present study compared 3 clinical models for estimating the risk of endometrial cancer in post-menopausal women with abnormal vaginal bleeding. These models can help simplify the evaluation and referral of these women. With an area under the ROC curve of 0.8389, the AMI30 model can properly differentiate between women with and without endometrial cancer.