1. Introduction
Primary fallopian tube carcinomas are rare gynecological tumors accounting for approximately 1% of primary genital tract malignancies (1-3).
Histologically, all the major types of carcinoma that occur in the ovary have been reported in the fallopian tubes, with the most common type being serous (papillary) adenocarcinoma (1,2). Transitional cell carcinoma is a rare histological variant and fewer than 25 cases have been reported worldwide so far (2,4). Here, we report a case of transitional cell carcinoma of the fallopian tube with pre-operation diagnosis of myoma in broad ligament.
2. Case Presentation
A 42-year-old premenopausal lady G2L2 presented with spotting and lower abdominal pain since one year ago. She also complained about dysmenorrhea and dyspareunia. Her past medical history was not significant and she did not have family history of gynecological or other malignancies.
In physical examination, she had pallor and mild abdominal protrusion. Her laboratory findings showed hypochromic normocytic anemia (Hb: 10.7 g/dL, normal range: 12.1 to 14.1 g/dL) and elevated CA-125 (135 U/mL, normal value: 35 U/mL). Besides, her Pap smear report was normal and endometrial curettage showed proliferative endometrium with no evidence of malignancy.
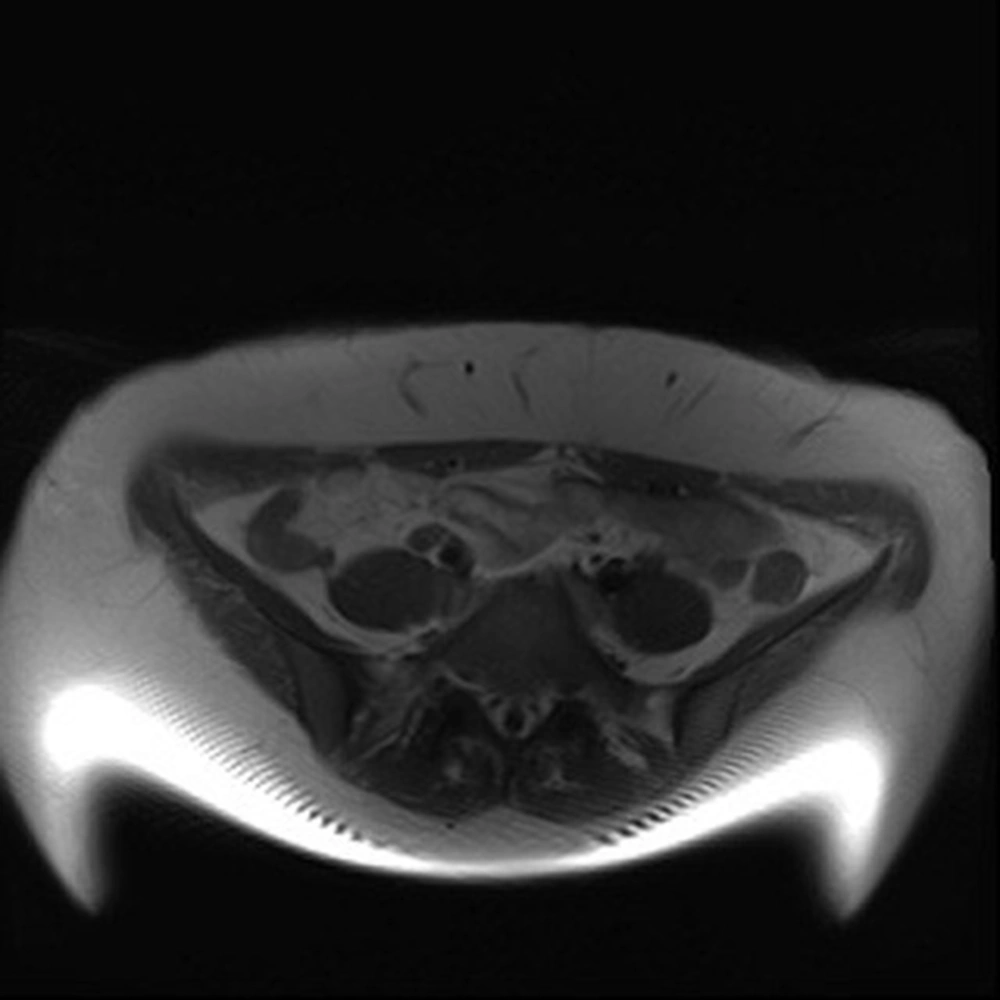
In radiological workup, she had pelvic sonography which showed a hypoechoic non-homogenous mass lesion with diameter of about 7 × 4 cm in the right posterolateral aspect of the posterior cul-de-sac and near the right ovary with possibility of subserosal myoma versus neoplastic ovarian lesion (Figure 1). Right and left ovaries were normal except for few cystic follicles. In addition, uterus had normal size and thickness with an intramural myoma of 1 cm. Urinary bladder was also normal with no stones or space occupying lesions. Pelvic Magnetic Resonance Imaging (MRI) revealed a well-defined round solid lesion measuring 5 × 3 × 3 cm arising from the right lower segment of the uterus which had signal intensity less than myometrium and minimal free fluid in cul-de-sac with possible diagnosis of pedunculated subserosal myoma (Figure 2).
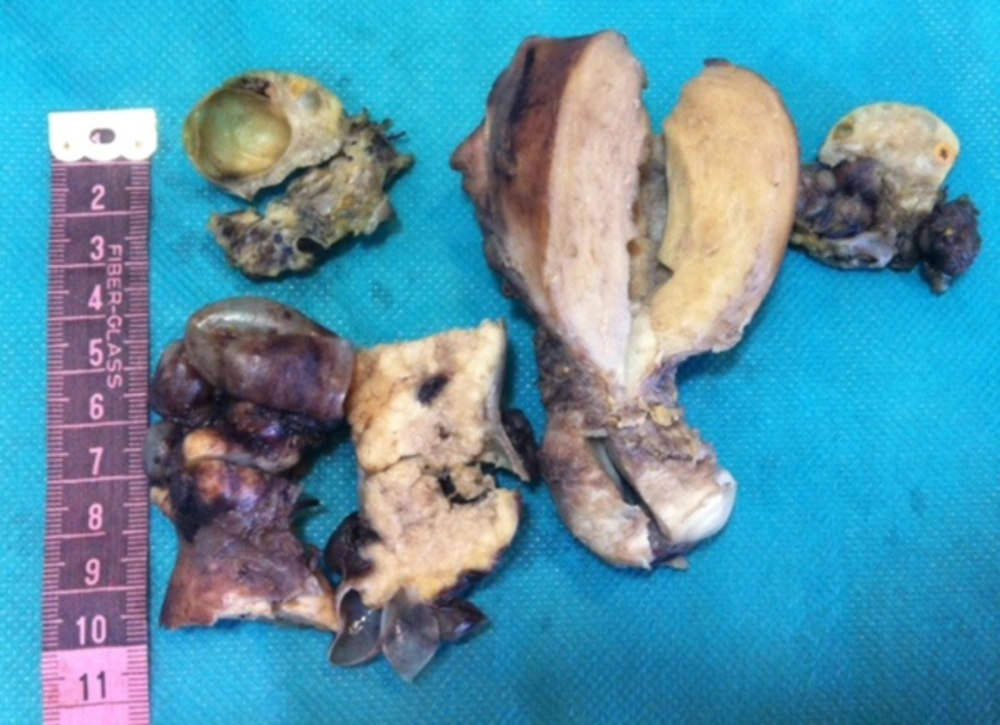
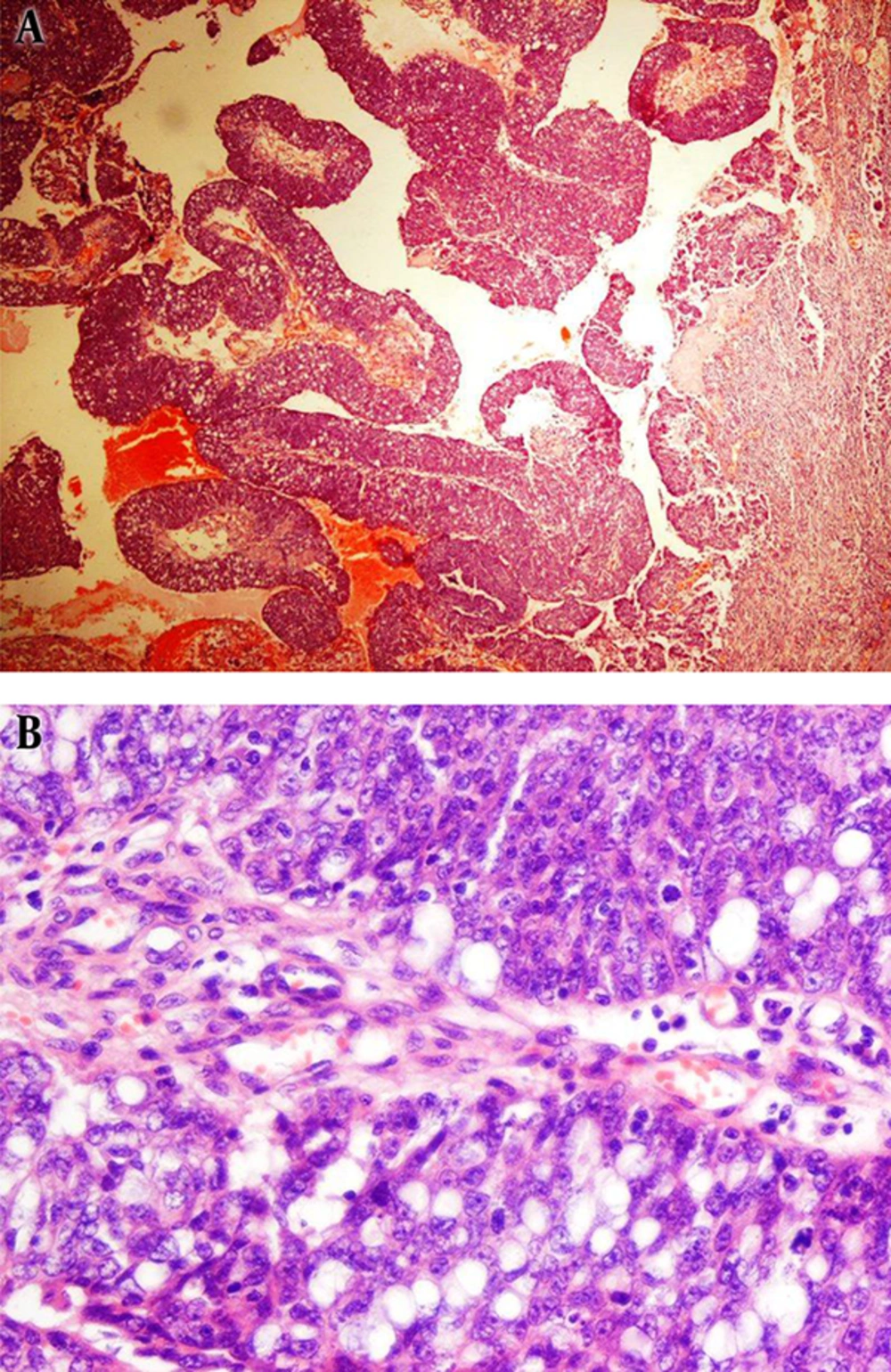
Therefore, the patient was scheduled for operation with pre-operation diagnosis of myoma in broad ligament. However, a solid-cystic mass was seen in the fallopian tube during the operation. Then, the intraoperative frozen section was sent to the pathology ward and was diagnosed as a malignant epithelial tumor. Thus, total abdominal hysterectomy, bilateral salpingo-oophorectomy, multiple peritoneal biopsies, and omentectomy were done for the patient besides removal of the main mass. The right fallopian tube which was first sent for the intraoperative frozen section had a solid-cystic mass measuring 7 × 5 × 4 cm with creamy cut surface and soft to rubbery consistency (Figure 3). Grossly, the uterus and the left ovary were unremarkable and the right ovary showed a functional cyst measuring 1.3 cm in the greatest diameter. Microscopically, the mass was composed of nests and papillae of highly atypical cells with some punched out microcystic spaces and patchy areas of necrosis. Besides, the tumor cells’, nuclei had prominent nucleoli and some showed nuclear grooves with more than 20 mitoses per 10 high power fields. These were all consistent with diagnosis of transitional cell carcinoma (Figure 4A and 4B). The patient underwent chemotherapy and is well after 11 months. An informed consent was obtained from the patient for publication of this case report.
3. Discussion
Primary fallopian tube carcinomas are rare gynecological tumors (1-3). More than 90 % of malignant tumors of fallopian tube are adenocarcinomas (1,2). Transitional cell carcinoma of the fallopian tube is a rare histological subtype that needs to be distinguished from the other subtypes due to different prognosis and better response to chemotherapy (1,2).
Primary carcinoma of the fallopian tube is proved in case all the criteria first suggested by Hu et al. and later modified by Sedlis in 1978 are met. These criteria include i) the tumor originates from the endosalpinx, ii) the histological pattern mimics the epithelium of the tubal mucosa, iii) transition from benign to malignant epithelium is found, and iv) the ovaries are free of tumors or have smaller tumors compared to the tube (2).
Most patients with fallopian tube carcinoma are postmenopausal (2) and in the fifth and sixth decades of their lives (3). Yet, the incidence of tubal carcinoma is higher in nulliparous compared to parous women (3). In this condition, most signs and symptoms are non-specific (1). Abnormal vaginal bleeding is the most common symptom and other symptoms include abdominal pain, dysmenorrhea, and mass sensation. Moreover, Latzke’s triad of the disease represented by vaginal discharge, abdominal and/or pelvic pain, and a palpable pelvic mass occurs in less than 15% of the patients (2,3).
The etiology of primary fallopian tube carcinoma is unknown; germ line mutation of BRCA 1 or 2 is the only recognized risk factor (3). Fallopian tube transitional cell carcinoma may arise from transitional metaplasia of tubal serosa, paratubal cyst, or Walthard cell nest (3,4).
Pre-operative diagnosis of fallopian tube tumors is usually a difficult task because of non-specific symptoms and low index of suspicion for this tumor due to its rarity (4). Ultrasonography is valuable for detecting a tubal mass. Nevertheless, when a tubal mass is detected, other radiological modalities, such as computed tomography (CT) and MRI, are not helpful in establishing the diagnosis (3,4).
In most of such patients especially in those with advanced disease, CA125 is increased. Pretreatment CA125 levels are independent prognostic markers and are associated with disease-free survival in the patients with fallopian tube carcinoma. Similar to ovarian carcinoma, CA125 is a valuable marker for post-treatment follow up in tubal carcinoma (3,4).
Few cases of fallopian tube tumors have abnormal Pap smear results, and diagnosis of transitional cell carcinoma of the fallopian tube from cervical cytology has been reported just once (5).
Total abdominal hysterectomy, bilateral salpingo-oophorectomy, tumor debulking, and full staging are the treatment of choice for fallopian tube malignancies. Survival rates are better with complete removal of the tumor and with pelvic and para-aortic lymphadenectomy in comparison to lymph node sampling (1-4). Moreover, adjuvant chemotherapy with a combination of carboplatin and paclitaxel, which is the gold standard of chemotherapy in epithelial ovarian cancer, is advised after surgery due to the risk of recurrence in fallopian tube carcinoma (3). It should be noted that transitional cell carcinoma is among the subtypes with good response to chemotherapy (1,2).
In the case presented above, the patient was neither postmenopausal nor nulligravid and radiological findings were in favor of an extrauterine myomatous lesion in broad ligament which could be preceded to wrong or insufficient management of the patient without intraoperative diagnosis of the tumor. In conclusion, it seems that frozen sectioning is an appropriate procedure in diagnosis and correct management of adnexal masses which are separated grossly from ovaries or uterus.