1. Background
Oral cancer is a common malignancy with annual global estimated incidence of about 2,750,00 (1). Approximately two-thirds of these cancers have been reported to occur in developing countries (2). In India, oral cancer has the highest incidence among men and the third highest incidence among women (3). Almost 80,000 cases of head and neck cancer are diagnosed annually and 46,000 oral cancer-related deaths occur yearly (4). The global incidence of oral cancer is on the rise, especially in developing countries (5). The 5- year survival remains approximately 50% (6). To reduce morbidity and mortality, oral lesions and conditions which often precede oral cancer, better known as oral potentially malignant disorders (OPMD) must be identified and managed early. The oral cavity is well suited for easy, early detection of OPMD because it can be readily visualized and examined by the individual. Still, only 34% of oral malignancies are diagnosed at an early stage when the cancer is localized (7). Although oral cancer is the sixth most common cancer across the globe, public awareness of this serious malignancy and OPMD remains low, especially in the Indian subcontinent (2). A plausible solution to improve this situation is to increase the awareness of these OPMD among those who have high risk potential, so that they promptly seek professional care. There is a strong association of the carcinoma occurring in the oral cavity with tobacco use and up to 80% of oral cancer cases are associated with tobacco use in different forms (8). In general, tobacco and alcohol users over the age of 40 are at highest risk for this disease but often do not appreciate their own sensitive risk status (9). In India, regular use of tobacco in one form or the other was reported by 43% of rural males and 28% of urban males (NSSO 1998). Previous studies have focused mainly on awareness of oral cancer, especially pertaining to either the public’s knowledge of causative factors (e.g., tobacco, alcohol) and signs of oral cancer (10-14) or confined to a specific sample like medical undergraduates students, dentists and primary care physicians (5, 15-18). Very few studies have investigated the awareness of individuals regarding OPMD (2, 19-21). A small number of studies have been dedicated to high risk patients, tobacco and alcohol users, but have been mainly limited to oral cancer awareness (9, 22, 23). This is the first study to evaluate awareness of OPMD and oral cancer among those with heightened risk of developing them because of their lifestyle. The aim of this study was to investigate the self-awareness of individuals, regarding OPMD and oral cancer, knowledge of its major risk factors and clinical signs, who are at higher risk of developing them because of their adverse habits.
2. Methods
This cross-sectional study was conducted at SDM college of dental sciences and hospital, Dharwad, India in 2009 - 2010, which is the only tertiary care centre in the district and therefore the catchment area of this centre covers the whole Dharwad district. Prior permission from Institutional ethical committee was taken before starting the study (IEC/2009). Study population comprised of patients visiting dental outdoor patient department with different oral/ dental problems that were screened for the adverse habit of tobacco or alcohol consumption in any form at the time of this study or having such a previous history. Five hundred patients with history of tobacco or alcohol consumption were recruited in the current study and formed the study sample. The sample size was calculated using G power software in accordance with the questions in the questionnaire. Written informed consent was obtained from each enrolled person. Diagnosed cases of OPMD and squamous cell carcinoma affecting the oral cavity were excluded from this study.
Demographic data (name, age, gender, and address) and relevant information, such as education and occupation were noted. All subjects were interviewed for tobacco and alcohol consumption history, using an interviewer-administered structured pre-validated questionnaire. As part of the interview, subjects were asked six questions regarding awareness of OPMD and oral cancer, and their responses were noted on a 3-point scale (yes/no/not sure). The subjects’ awareness of risk factors, like tobacco use and alcohol consumption, associated with increased risk of OPMD and oral cancer was evaluated on a 4-point response scale. Study participants’ knowledge of clinical signs and symptoms which may be possible indicators of OPMD and oral cancer was also assessed in this study. The awareness response was cross-tabulated with variables such as age, sex, education, monthly income, occupation, marital status and type of tobacco use. Statistical analysis was done using SPSS: Chicago, IL, USA (version 13). The relationships between two categorical variables were tested by chi-square. P values of < 0.05 were considered statistically significant.
3. Results
A total of 500 patients who had habit of tobacco or alcohol consumption at the time of study or in the past were included in this study. The mean age of the study subjects was 38.8 years (age range 16 - 80 years) with majority of them being males (94.4%) (Table 1). Approximately 36% of the subjects had no or primary education whereas 30.8 % had received graduation level education. Professional and clerical occupations were represented by 33% of the subjects, 36% belonged to skilled/unskilled workers, 9.2% were self-employed, 7.6 % were unemployed/housewives and 14.2% were students. Seventy-two percent of the study participants were married at the time of investigation and 66% had monthly income below 10,000 Rupees.
| Characteristics | Number | Percentage |
|---|---|---|
| Gender | ||
| Male | 472 | 94.4 |
| Female | 28 | 5.6 |
| Age | ||
| 10 - 20 | 34 | 6.8 |
| 21 - 30 | 157 | 31.4 |
| 31 - 40 | 103 | 20.6 |
| 41 - 50 | 87 | 17.4 |
| 51 - 60 | 65 | 13 |
| 61 - 70 | 48 | 9.6 |
| 71 - 80 | 6 | 1.2 |
| Level of education | ||
| Illiterate | 111 | 22.2 |
| Primary education | 69 | 13.8 |
| Higher secondary level | 166 | 33.2 |
| Graduate or higher | 154 | 30.8 |
| Monthly Income | ||
| 0 - 10,000 | 330 | 66 |
| 10,001 - 25,000 | 37 | 7.4 |
| > 25,000 | 24 | 4.8 |
| Occupation | ||
| Unemployed and house wives | 38 | 7.6 |
| Skilled and unskilled | 180 | 36 |
| Professional and clerical | 165 | 33 |
| Self employed | 46 | 9.2 |
| Student | 71 | 14.2 |
| Marital status | ||
| Single | 140 | 28 |
| Married | 360 | 72 |
Socio-Demographic Data of Study Participants (n = 500)
3.1. Prevalence of Risk Habits Among Study Participants
Adverse Life styles of the study participants was evaluated by detailed questioning about tobacco and alcohol consumption habits including the frequency, duration and ever or current use. Ever users were defined as those who had such habits in the past but had quit the habit at the time of this study. Tobacco consumption was divided into smoking and smokeless form of tobacco users. The smoking category was further divided into cigarette or bidi smoking, whereas smokeless tobacco was categorized as gutkha chewers, betel quid chewers with tobacco and without tobacco, and areca nut chewers (Table 2). Bidi smoking was observed in 43 (8.6%) of study participants with a mean frequency of 12.05 (SD 9.788) times/day and mean duration of 22.02 (SD 12.33) years. Cigarette smokers (86 participants) had mean frequency of 5.4 (SD 4.8) times/day and mean duration of 10.52 (SD 9.907) years. A total of 476 (85%) of the study population had habit of smokeless tobacco consumption in one or the other form with a mean frequency of 6.67 (SD 6.36) times/day and mean duration of 10.18 (SD 9.96) years. In the study sample, 91 patients had habit of both smoking and smokeless tobacco consumption. There were 41 patients who reported alcohol consumption (36 current and 5 ever) with a mean alcohol quantity being 138.66 (SD 114.91) ml/day and mean duration of 10.18 (SD 10.36) years.
| Variables | Tobacco Smoking | Smokeless Tobacco | ||||
|---|---|---|---|---|---|---|
| Cigarette | Bidi | Gutkha chewing | Betel quid chewing (with tobacco) | Betel quid chewing (without tobacco) | Areca nut chewing | |
| N (%) | 86 (17.2) | 43 (8.6) | 156 (31.2) | 250 (50) | 51 (10.2) | 19 (3.8) |
| Frequency, number of times/day | ||||||
| 0 - 10 | 76 | 25 | 125 | 222 | 51 | 19 |
| 11 - 20 | 9 | 10 | 24 | 20 | 0 | 0 |
| > 20 | 1 | 8 | 7 | 8 | 0 | 0 |
| Duration, y | ||||||
| 0 - 10 | 55 | 13 | 139 | 135 | 42 | 16 |
| 11 - 20 | 24 | 12 | 16 | 71 | 6 | 2 |
| > 20 | 7 | 18 | 1 | 44 | 3 | 1 |
| Use | ||||||
| Ever | 5 | 2 | 9 | 9 | 0 | 0 |
| Current | 81 | 41 | 147 | 241 | 51 | 19 |
Tobacco Consumption Habits of Study Participants
3.2. Overall Awareness of Oral Cancer and OPMD
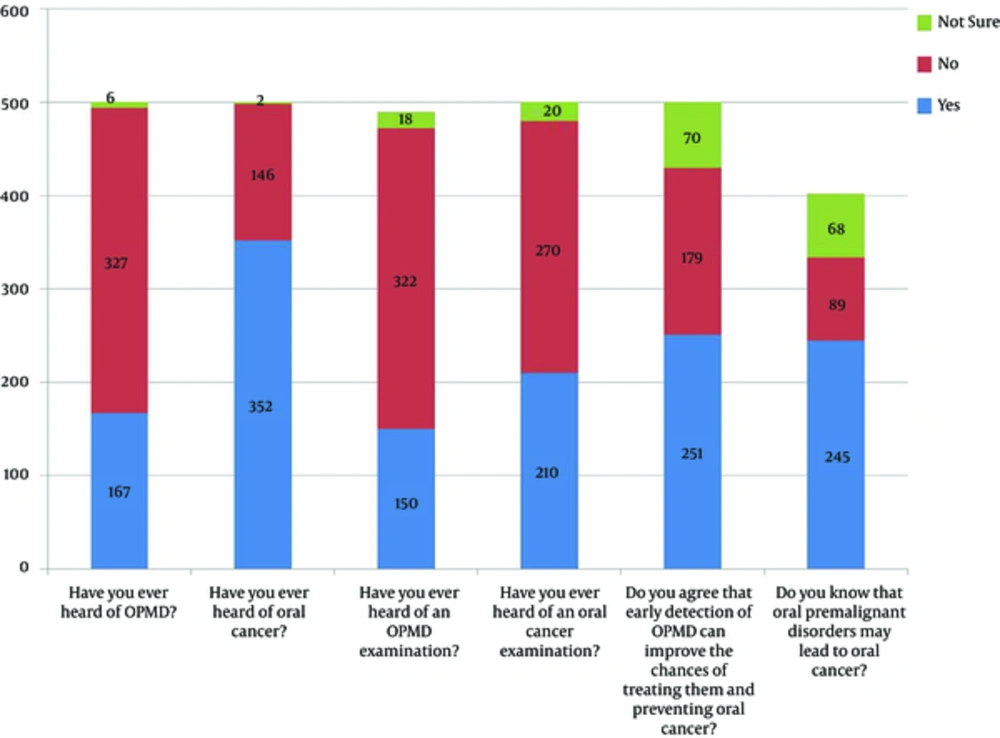
Of the study subjects, 70.4% were aware of oral cancer, but only 33.4% were aware of OPMD (Figure 1). Approximately 30% and 42%.of the study participants had heard of OPMD and oral cancer examination respectively. Approximately 50.2% of the study participants agreed that early detection of OPMD can improve the chances of treating them and preventing oral cancer, while 48.6% were aware that OPMD may lead to oral cancer.
3.3. Knowledge of Early Symptoms and Risk Factors
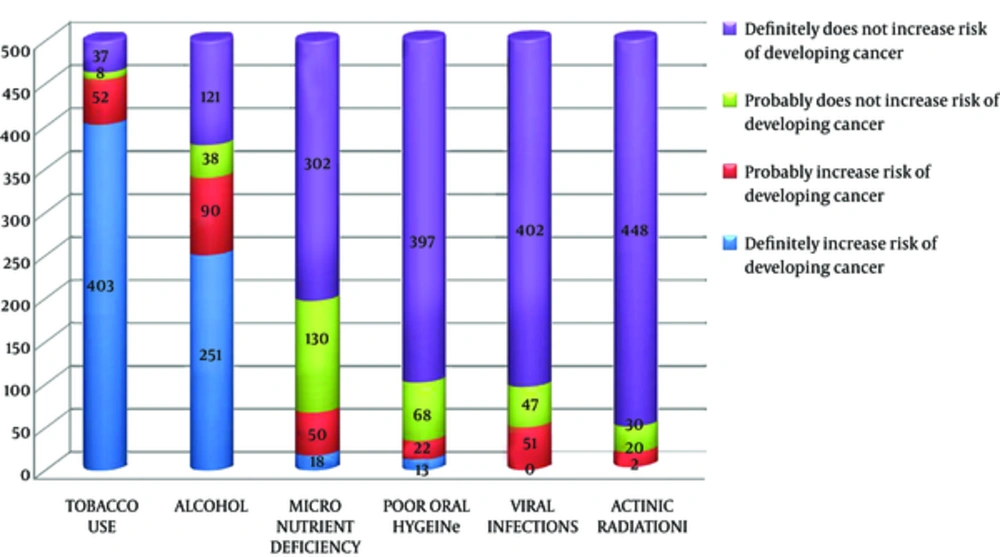
In relation to the awareness of the symptoms and risk factors of oral cancer and OPMD, the majority of subjects were not aware of the symptoms of oral cancer and of OPMD (Table 3). Among the 4 symptoms questioned, study subjects showed the highest awareness for pain or burning sensation of mouth (25%) while the lowest for non-healing sores or lesions (3%). Among those who were aware of these symptoms, majority correlated them with oral cancer rather than OPMD. Of the 500, 320 (64%) were not aware of even one symptom (Pain or burning sensation of mouth, restriction of mouth opening, white or red patches in the mouth and non-healing sores or lesions) of oral cancer or OPMD. About 77% and 60% subjects were aware that tobacco and alcohol consumption are risk factors for oral cancer but only 14% and 8.6% were aware of these as high risk behavior for OPMD. The subjects’ awareness of risk factors on 4-point response scale is shown in Figure 2.
| Awareness | Not Aware | Aware | |
|---|---|---|---|
| Oral cancer only | Both oral cancer and OPMD | ||
| Awareness of symptoms | |||
| Pain or burning sensation of mouth | 375 (75) | 86 (17.2) | 39 (7.8) |
| Restriction of mouth opening | 401 (80.2) | 79 (15.8) | 20 |
| White or red patches in the mouth | 432 | 49 | 19 |
| Non-healing sores or lesions | 485 | 15 | 0 |
| Awareness of risk factors | |||
| Tobacco use | 45 | 385 | 70 |
| Alcohol consumption | 159 | 298 | 43 |
| Micronutrient deficiency | 432 | 66 | 2 |
| Poor oral hygiene | 465 | 26 | 9 |
| Viral infections | 449 | 51 | 0 |
| Actinic radiation | 478 | 22 | 0 |
Awareness of Symptoms and Risk Factors of Oral Cancer and OPMDa
This study also investigated the awareness of micronutrient deficiencies, poor oral hygiene, viral infections and actinic radiations as risk factors for oral cancer and OPMD. Almost all (95.6%) were not aware of the implications of actinic radiations, and 93% were not aware of the risks associated with poor oral hygiene. Awareness regarding micronutrient deficiencies and viral infections were 13.6% and 10.2% respectively. The carcinogenic potential of all these risk factors were better known for oral cancer than OPMD.
3.4. Correlation Between Awareness and Socio-Demographic Characteristics and High Risk Behavior
Awareness of oral cancer, its magnitude, of OPMD, and of early signs and symptoms and risk factors were studied in relation to socio-demographic characteristics and adverse habits of subjects (Table 4). Significant differences were observed in the levels of awareness of both OPMD and oral cancer by age, gender, level of education, marital status and occupation. (P < 0.05) Significant difference was also observed for both OPMD and oral cancer when correlated with smoking type (P = 0.000) and the type of smokeless tobacco consumed (P = 0.000). No significant association was observed regarding the awareness of oral cancer and monthly income (P > 0.05), but this was significant for OPMD (P = 0.023). Carcinogenic potential of tobacco perceived as high risk behavior showed statistically significant correlation for age (P = 0.000), occupation (P = 0.010) and type of smokeless tobacco consumed only (P = 0.030). Cross tabulation of the risk factors tobacco and alcohol in terms of 4-point scale, showed Pearson Chi-square coefficient of 272.265 and likelihood ratio of 241.639 (P Value = 0.000). Awareness of the 4 symptoms of oral cancer and OMPD showed statistically significant correlation in terms of gender, level of education, occupation, monthly income, smoking type and type of smokeless tobacco consumption (P < 0.05). No correlation was observed between monthly income for all the 4 symptoms and for non-healing sores and lesions only for age (P > 0.05).
| Characteristics | Sample | P Value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Awareness of OPMD and oral cancer | Awareness of risk factor - tobacco | Awareness of symptoms of OPMD and oral cancer | ||||||||||
| Q1a | Q2b | Q3c | Q4d | Q5e | Q6f | S1g | S2h | S3i | S4j | |||
| Gender | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.068 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Male | 472 | |||||||||||
| Female | 28 | |||||||||||
| Age | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.007 | 0.000 | 0.000 | 0.000 | 0.317 | |
| 10 - 20 | 34 | |||||||||||
| 21 - 30 | 157 | |||||||||||
| 31 - 40 | 103 | |||||||||||
| 41 - 50 | 87 | |||||||||||
| 51 - 60 | 65 | |||||||||||
| 61 - 70 | 48 | |||||||||||
| 71 - 80 | 6 | |||||||||||
| Level of education | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.068 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Illiterate | 111 | |||||||||||
| Primary education | 69 | |||||||||||
| Higher secondary level | 166 | |||||||||||
| Graduate or higher | 154 | |||||||||||
| Monthly Income | 0.023 | 0.844 | 0.136 | 0.022 | 0.124 | 0.256 | 0.894 | 0.500 | 0.172 | 0.731 | 0.974 | |
| 0 - 10,000 | 330 | |||||||||||
| 10,001 - 25,000 | 37 | |||||||||||
| > 25,000 | 24 | |||||||||||
| Occupation | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.010 | 0.000 | 0.000 | 0.000 | 0.000 | |
| Unemployed and house wives | 38 | |||||||||||
| Skilled and unskilled | 180 | |||||||||||
| Professional and clerical | 165 | |||||||||||
| Self employed | 46 | |||||||||||
| Student | 71 | |||||||||||
| Marital status | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.266 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Single | 140 | 0.000 | ||||||||||
| Married | 360 | |||||||||||
| Smoking type | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.44 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Bidi | 43 | 0.000 | ||||||||||
| Cigarette | 86 | |||||||||||
| Smokeless tobacco | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.030 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Gutkha chewing | 156 | 0.000 | ||||||||||
| Betel quid chewing (with tobacco | 250 | |||||||||||
| Betel quid chewing (without tobacco) | 51 | |||||||||||
| Areca nut chewing | 19 | |||||||||||
Awareness of Oral Cancer and OPMD According to Socio-Demographic Characteristics and Adverse Habits of Subjects
4. Discussion
This study highlights the alarming lack of awareness of OPMD as compared to oral cancer among tobacco and alcohol users. Although 70.4% of the study participants were aware of oral cancer, only 33.4% were aware of OPMD and even fewer (30%) had heard of OPMD examination. Surprisingly, though 352 study participants had heard of oral cancer, only 210 had an idea regarding oral cancer examination. The level of awareness of oral cancer reported in this study is better than other studies previously reported. Warnakulasuriya (13) had previously reported the awareness of oral cancer in 56% of the respondents in Great Britain in the year 1999. In a study assessing awareness of oral cancer among Florida adults above 40 years, 15.5% had never heard of oral cancer and another 40.3% reportedly knew little or nothing about it (12). Another study which collected data from a large oral cancer screening program in New York and New Jersey area reported that 66 percent of its study participants had heard about oral cancer; however, only 39 % reported having heard of an oral cancer examination (11). These studies had taken study sample from low risk populations where prevalence of risk factors like tobacco and alcohol is low, thereby accounting for low awareness of OPMD and oral cancer. Similar results to the present study regarding awareness of oral cancer and OPMD have been reported recently among some rural populations of Srilanka, which is a high risk population (2). The level of public awareness of oral cancer was 84%, but only 23% for OPMD. In the Indian scenario, a study done to evaluate the awareness of oral cancer as well as its risk factors and to estimate the prevalence of risk factors in a high-risk semi-urban population in Kerala reported that 86% had heard about oral cancer and 62% of the subjects correctly identified the causes of oral cancer (22). A study involving male alcohol drinkers and tobacco smokers above the age of 44 in England revealed lack of knowledge and understanding of the risk of oral cancer, in this whole at-risk population sample (9). In the present study, similar at-risk study sample was selected as all study subjects had habit of either tobacco or alcohol use, while some had both. Further, the study population chosen here were those attending a dental hospital who are regularly exposed to health care messages and therefore may be more aware of the OPMD and oral cancer than the overall population. The awareness for oral cancer was much more than OPMD in our study. Previous studies have reported awareness of OPMD ranging from 19% (Formosa et al. (21)), 22.7% (Amarasinghe et al. (2)) to 44.9% (Ariyawardana et al. (19)).
Poor awareness of presentation of OPMD and oral cancer in the oral cavity was found in the present study. This is in accordance with the data published from the United Kingdom in 2006 (14) and Srilanka in 2010 (2). Amarasinghe et al. (2) reported that awareness of early signs was significantly lower in people who, as a result of their behavior, are at higher risk. Further, the awareness of oral cancer and OPMD, their early symptoms, and tobacco use as risk factor were found to significantly vary among different age groups, gender, education level, occupation and according to the marital status. Similar results were found for the type of smoking and smokeless tobacco used.
This study has brought to light a disturbing aspect that though all the study subjects in this study had high risk behavior, only a handful recognized that their adverse habit could lead to OPMD. Tobacco use and alcohol consumption were appreciated as risk factors for oral cancer by 77% and 60% of the subjects, which was an encouraging finding, but only 14% and 8.6% were aware of these as high risk behaviors for OPMD. Among those who were aware of OPMD, not even half appreciated their lifestyle could lead to development of OPMD. The awareness of other risk factors like poor oral hygiene, actinic radiation, viral infections and micronutrient deficiency was very low. Formosa et al. (21) have reported that 92% of their study respondents agreed or strongly agreed that smoking is a strong risk factor for oral cancer, followed by tobacco chewing (84%), tobacco chewing with areca nut (68%), chewing areca nut alone (51%) and exposure to actinic radiation (71%) as risk factors. However, the results for alcohol intake, age, and HPV infection were found to be relatively poor with proportions 33%, 34%, and 23% respectively. In the study by Elango et al. (22) 77% of the subjects identified smoking, 64% alcohol and 79% pan chewing as a cause of oral cancer. Ariyawardana et al. (19) reported that 80.7%, 47% and 17% were aware of links with tobacco smoking and alcohol consumption, respectively. Results similar to our study were reported by Amarasinghe et al. (2) where majority of alcohol consumers and smokers and about half of the betel quid chewers surveyed were unaware of the risks conferred by their lifestyles. Pai et al. (23) reported that smokers and past users of tobacco were found to be more aware of effects of tobacco on oral and general health as compared to smokeless and current users but awareness about OPMD remained low in their study as well. This situation calls for specific intervention. There is need for not only increasing awareness regarding OPMD and its presentation in the oral cavity, but the association between adverse life style and increased risk of developing OPMD needs to be stressed. In addition, information needs to be focused on making the tobacco and alcohol users aware of the synergistic potential of these high risk behaviors leading to development of oral cancer and OPMD. For the small number of tobacco and alcohol users who were aware of OPMD as well as its causal relationship with their adverse lifestyle, it is understood that other factors must be reinforcing continued use. Further investigations have to be carried out to find out the reasons behind the continued practice of high-risk habits, despite knowledge. For this subset, specific counseling is necessary.
In conclusion, awareness of oral cancer and OPMD is low in this study, a conclusion observed in many studies conducted globally. There is the greatest need to raise awareness in those at most risk due to their adverse lifestyle. Oral cancer should be our top priority in terms of public policy on increasing awareness of cancer. Early recognition and management is the key to reduce mortality associated with oral cancer, and increasing awareness and screening for OPMD is the most concrete step in this direction.