1. Background
Radiotherapy is the gold standard for treatment of prostrate cancer as it can cover an adequate area of tissues at risk for metastasis (1). Prevention of normal tissues of rectum and bladder from high radiation scattered dose, lead to less complications related to radiation therapy (2). Conventional pelvic field parameters have used bony landmarks to design pelvic radiation therapy volumes rather than methods that can more precisely show the related pelvic nodes (3). Previous studies have indicated that conventional fields do not provide adequate margins in the gross primary tumor volume in some of the patients that decreased the local control of tumor (4). CT simulation may be helpful in detecting the corresponding lymphatic vessels and lymph nodes in imaging, and it has been broadly used around the world (5). Finlay et al. (6) used CT simulation and evaluated the coverage of conventional pelvic fields and detected that 95.4% patients had at least one insufficient margin; the authors recommended that non invasive CT simulation would provide more accurate radiation planning than bony landmarks. In agreement to Finlay’s findings, several authors indicated that conventional pelvic field provide inadequate coverage or may include normal tissue (7-11). In CT simulation images, the blood vessels of pelvic are contoured and used as a marker of lymphatic vessels and lymph nodes (5).
2. Objectives
In this study, we evaluated the pelvic lymph node coverage of conventional radiotherapy fields based on bony landmarks and CT based simulation in patients with prostate cancer referred to Shohada-e-Tajrish Hospital.
3. Patients and Methods
In this cross sectional study, 40 patients with prostate cancer were recruited. Informed written consent for radical radiotherapy was obtained from all the patients before the study.
Distances were measured at levels of aortic bifurcation of the common iliac vessels artery and superior border of AP field, external iliac vessels and lateral border of the AP field, external iliac vessels and anterior border of the lateral field and posterior border of lateral field to sacral lymph nodes.
CT simulation was performed by Multislice spiral CT every 5 mm for all patients and transferred to treatment planning system (TPS).
3.1. Setting of Conventional Pelvic Fields
On the anterior/posterior (AP) field, L5 – S1 interspace was recognized as the superior border; inferior border was verified based on the inferior aspect of the obturator foramen. Moreover, 1.5 cm beyond the widest part of the pelvic brim was assigned as the lateral border. The most anterior part of the symphysis pubis on the lateral (LAT) was verified as the anterior border, and S2-S3 interspace was verified as the posterior border field. The superior and inferior borders were identical to those on the AP fields.
3.2. Pelvic Lymph Node Coverage Measurements
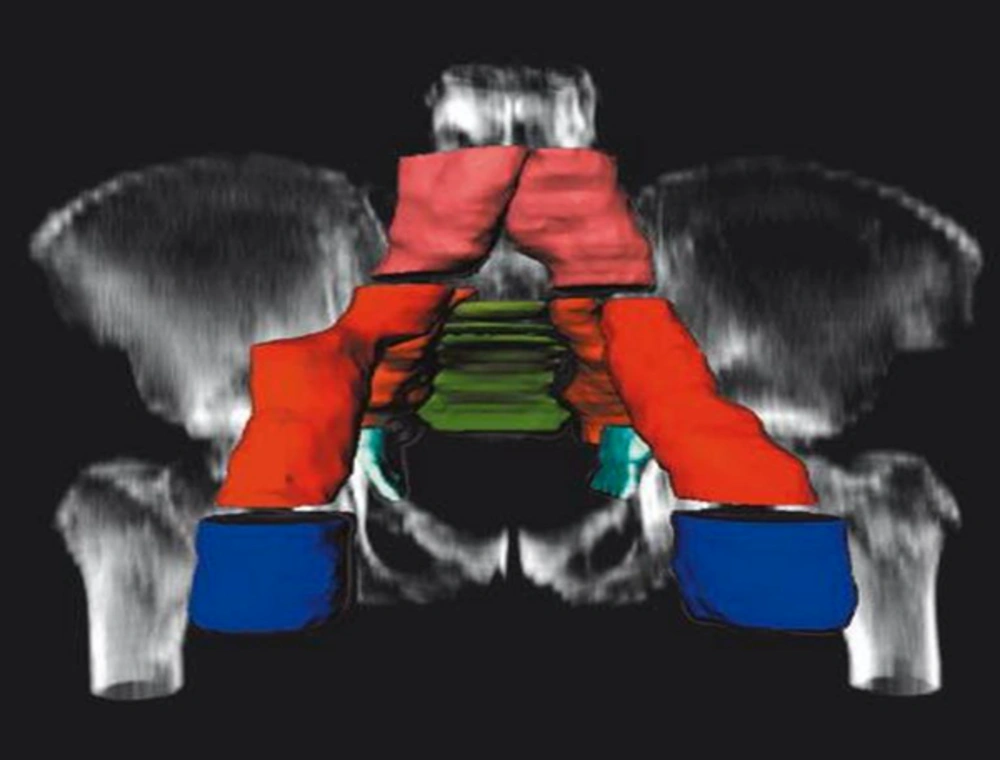
Pelvic vessels were contoured and also demonstrated on coronal and sagittal digitally reconstructed radiograph images. Then distances between the following parts were measured (Figure 1).
We contoured pelvic vessels and labeled on coronal and sagittal digitally reconstructed images and assessed the distance of aorta and superior border of the AP field (A), the distal end of the external iliac artery and ipsilateral border of the AP field (B) and anterior border of the LAT field and the distal end of the external iliac artery (C). The distances more than 5 mm were considered as adequate.
3.3. Statistical Analyses
We used this formula to calculate the sample size:

Z = the appropriate value from the normal distribution for 95%confidence=1.960
P = the anticipated prevalence
d = confidence interval
Then the required sample size for our study was 40.
Data were analyzed using SPSS version 20. Categorical data were presented as numbers (%), and continuous data as mean ± SD.
4. Results
In this study 40 patients were included. Mean and standard deviation of the distance of aortic bifurcation from the superior border was 4.73 ± 1.16 cm, the distance of common iliac bifurcation from the superior border was 1.11 ± 1.25 cm, the mean (SD) distance of right external iliac from the lateral border of AP field was 2.06 ± 0.48 cm and for left external iliac artery was 1.90 ± 0.56 cm. The distance of the external iliac artery from the anterior border of the lateral field was 2.30 ± 0.74 cm, the distance of the external iliac artery from pelvic rim was 0.59 ± 0.59 cm, distance of iliac bifurcation from sacroiliac joint was 0.82 ± 1.01 cm, the size of the pelvic rim was 12.30 ± 0.64 cm, sacral width 8.29 ± 1.01 cm, anterior promontory symphysis distance 12.02 ± 0.92 cm and posterior promontory symphysis distance was 10.98 ± 0.73 cm (Table 1).
| Anatomical Region | Mean ± SD | Median | Range |
|---|---|---|---|
| Bifurcation of aorta from superior border | 4.73 ± 1.16 | 4.75 | 2.7 - 7 |
| Common iliac bifurcation from superior border | 1.11 ± 1.25 | 1.25 | -1.40 - 3.30 |
| Right external iliac from lateral border of AP field | 2.06 ± 0.48 | 2.00 | 1 - 3 |
| Left external iliac from lateral border of AP field | 1.90 ± 0.56 | 1.58 | 0.2 - 3 |
| External iliac from anterior border of lateral field | 2.30 ± 0.74 | 2.30 | 0 - 4 |
| External iliac artery from pelvic rim | 0.59 ± 0.59 | 0.80 | -1 - 1.5 |
| Iliac bifurcation from sacroiliac joint | 0.82 ± 1.01 | 0 | -2.10 - 2.70 |
| Size of the pelvic rim | 12.30 ± 0.64 | 12.50 | 11.30 - 13.80 |
| Sacral width | 8.29 ± 1.01 | 8 | 7.40 - 9.40 |
| Anterior promontory symphysis distance | 12.02 ± 0.92 | 11.95 | 10.40 - 14.20 |
| Posterior promontory symphysis distance | 10.98 ± 0.73 | 11 | 9 - 12.30 |
The Mean and Standard Deviation, Median and Range of Vessels Contouring
5. Discussion
The radio therapeutic fields of patients with prostate cancer were mostly planned by bony landmarks. However some recent studies on CT simulation confirmed that the conventional radiation fields usually did not have adequate coverage of pelvic lymph nodes (8-11). Simulation refers to the technique of defining the tumor or treatment field. In this technique, pelvic blood vessels can be recognized and contoured and used as surrogate markers to locate the lymphatic vessels and lymph nodes (5). In the present study, we evaluated pelvic lymph node coverage of conventional radiotherapy fields based on bony landmarks in patients with prostate cancer using virtual simulation based nodal mapping by using blood vessels as surrogate markers. Mean of bifurcation of aorta from the superior border, the distance of common iliac bifurcation from the superior border, the mean distance of right external iliac and left external iliac artery from the lateral border of AP field, the distance of the external iliac artery from the anterior border of the lateral field pelvic rim and distance of iliac bifurcation from sacroiliac joint was more than 5 mm and all pelvic lymph nodes showed adequate coverage. So, our finding indicated that CT simulation with vessel contouring as a surrogate for localization of lymph nodes resulted in more accurate field description. In agreement to our results, Tunio in a study on 40 patients with prostate cancer in 2011 showed inadequate coverage of the obturator lymph nodes at the level of the acetabulum and sacral lymph nodes at the level of the second sacral vertebra (12). Harmonically, Zhang et al. in a study on women with cervical cancer confirmed that conventional pelvic fields based on bony landmarks did not provide adequate coverage of pelvic lymph nodes, and CT simulation is more useful technique for planning pelvic fields (13).
In summary, our study results and previous investigations indicated that conventional pelvic fields based on bony landmarks provided inadequate coverage of pelvic lymph nodes. CT simulation can be a feasible technique for planning pelvic fields optimally and individually.
There are some limitations in our study. Firstly, intravenous contrast was not used, that limited the ability to recognize and contour the internal iliac vessels in a credible manner. Secondly, we paid more attention on pelvic vessel contouring and the capability of nodal coverage. However which of these nodes are important for inclusion in treatment volumes and are infrequently complicated to be consequently excluded, is still unknown.
5.1. Conclusion
Radiotherapy using CT based simulation using pelvic vessels as surrogate markers provided adequate coverage for all pelvic lymph nodes in patients with prostate cancer.