1. Background
Transurethral resection of the bladder tumor is the standard surgical procedure for non-muscle invasive bladder cancer. Intramural tumors of urinary bladder are among the main causes of pelvic surgeries. Spinal anesthesia is anesthetic procedure of choice in which the reflex of adductor muscles is not blocked leading to some problems for surgeons and bladder perforation. The selective obturator nerve block is an alternative way for this matter (1, 2). More interest in obturator nerve block emerged a few years later when Pauchet, Sourdat and Labat performed the obturator nerve block combined with blocks of the sciatic, femoro-cutaneous nerves to anesthetize the entire lower extremity (3).
With the introduction of modern nerve stimulators, selective blockade of the obturator nerve has become more reliable and has seen a resurgence of interest in recent times (4, 5). The obturator nerve is a mixed nerve which in most cases provides motor function to the adductor muscles and skin sensation to a small area behind the knee. The obturator nerve blockage has a success rate ranging from 65 to 90 percent according to blind use or guided one and however selective blockade of the obturator nerve is relatively safe, there is little possibility of neural injury or some injuries to other neighboring parts (6). The frequency is not so clear because the patient has previously had spinal anesthesia. For this reason, the use of an imaging guide is a useful tool for better performance during the procedure and the use of ultrasonographic guide is an option for this matter (7). Accordingly, in this study, the procedures by selective obturator nerve block with and without use of ultrasonographic guide were compared.
2. Methods
This interventional study was performed as an open-label randomized clinical trial among 50 consecutive subjects under surgery for intramural tumors of urinary bladder in Shohada hospital, in 2016.
(α = 0.05, 1 - β= 90%, p1 = 0.60, p2 = 0.98, n = 25 in each group) and

The subjects were randomly assigned to be operated under spinal anesthesia accompanied with nerve locator guided selective obturator nerve block (10 mL of 1.5% lidocaine adding 1:200000 epinephrine (Iranpharma Co.)) with or without ultrasonographic guide. Randomization was performed by block method including five-patient blocks. Also all patients had spinal anesthesia with 3 mL of 0.5% bupivacaine after the block was performed.
The patients who signed the informed consent form were included. The study was approved by the university’s ethical committee (IR.SBMU.MSP.REC.1395.155) and the Helsinki Declaration was respected during the study.
All patients who needed Transurethral resection of the bladder tumor were enrolled in the study. Patients with addiction, sensory or motor deficit, ASA Class III and more, diabetes mellitus, coagulopathy, infection on injection site, hyper or hypotension, refusal to spinal anesthesia, surgery time more than 3 hours, need for general anesthesia, and electrolyte imbalance were excluded from study.
In both groups after standard monitoring and fluid therapy, the sedation was made by midazolam 0.02 mg/kg.
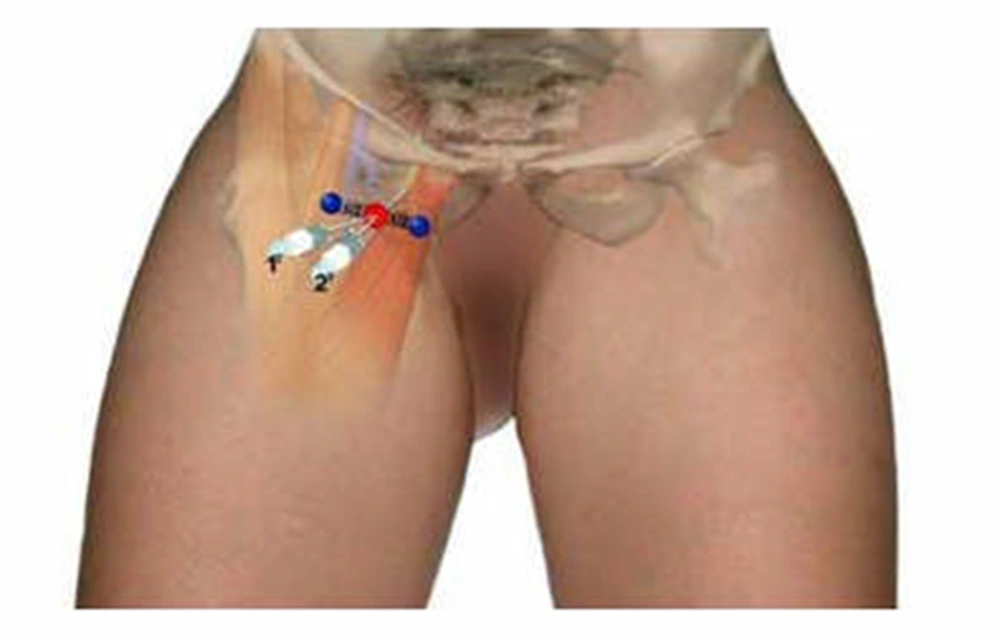
The used needle was 80 mm (visicon) and the aseptic techniques were respected. This ultrasonographic-guided (50 mm linear probe 6 - 13 MHZ Zonare L10-5, CA, US). Nerve stimulator guided block technique consists of selective block of the two branches of the obturator nerve (anterior and posterior), performed at the inguinal level and slightly more caudal. The femoral artery and the tendon of the long adductor muscle at the pubic tubercle were identified. For tendon identification, extreme leg abduction was required (Figure 1).
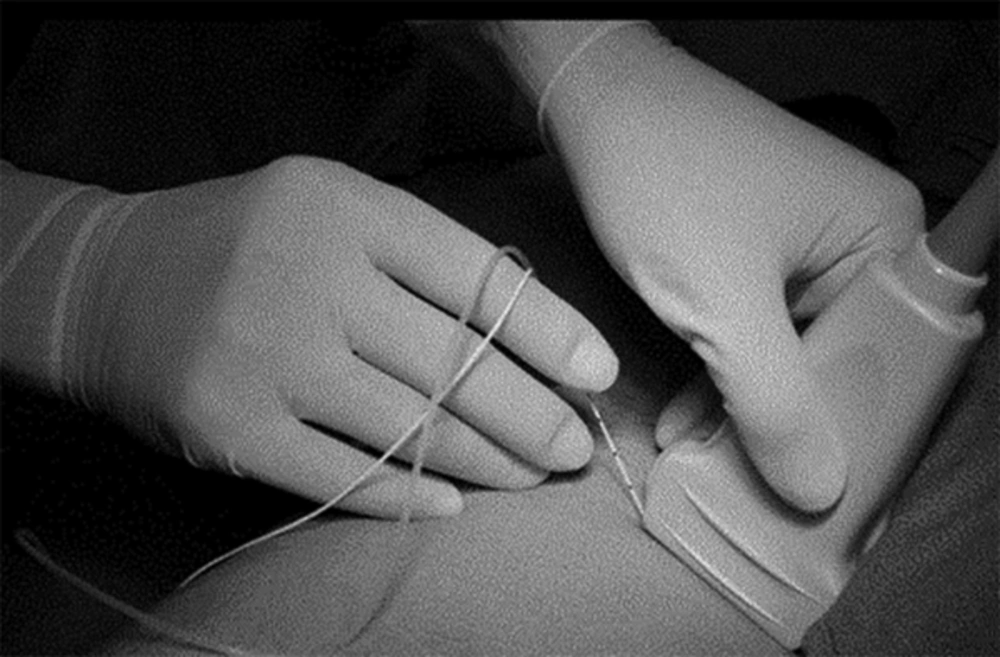
The needle was inserted at the mid-point of this line at an angle of 30° anterior/posterior and the long adductor muscle. Subsequently, the needle was inserted deeper (0.5 - 1.5 cm) and slightly laterally over the short adductor muscle until a response from the major adductor muscle was obtained and could be visualized on the posterior-medial aspect of the thigh. Nerve stimulation began using a current of 2 - 3 mA (2 Hz, 0.1 - 0.3 msec), and reduced to 0.5 mA before injection of local anesthetic. Following needle insertion, infiltration of 5 mL lidocaine was done. In sono-guided group place of injection was confirmed by sonography.
The injection was slow with a rate less than 10 mL per minute. Understudy variables included age, gender, lower extremity jerking, bladder hemorrhage, perforation, and other complications.
Data analysis was performed among 50 subjects including 25 patients under selective obturator nerve block with ultrasonographic guide and 25 subjects in control group without use of ultrasonographic guide. Data analysis was performed by SPSS (version 18.0) software (Statistical Procedures for Social Sciences; Chicago, Illinois, USA). Chi-Square and Exact-Fisher tests were used and were considered statistically significant at P values less than 0.05.
3. Results
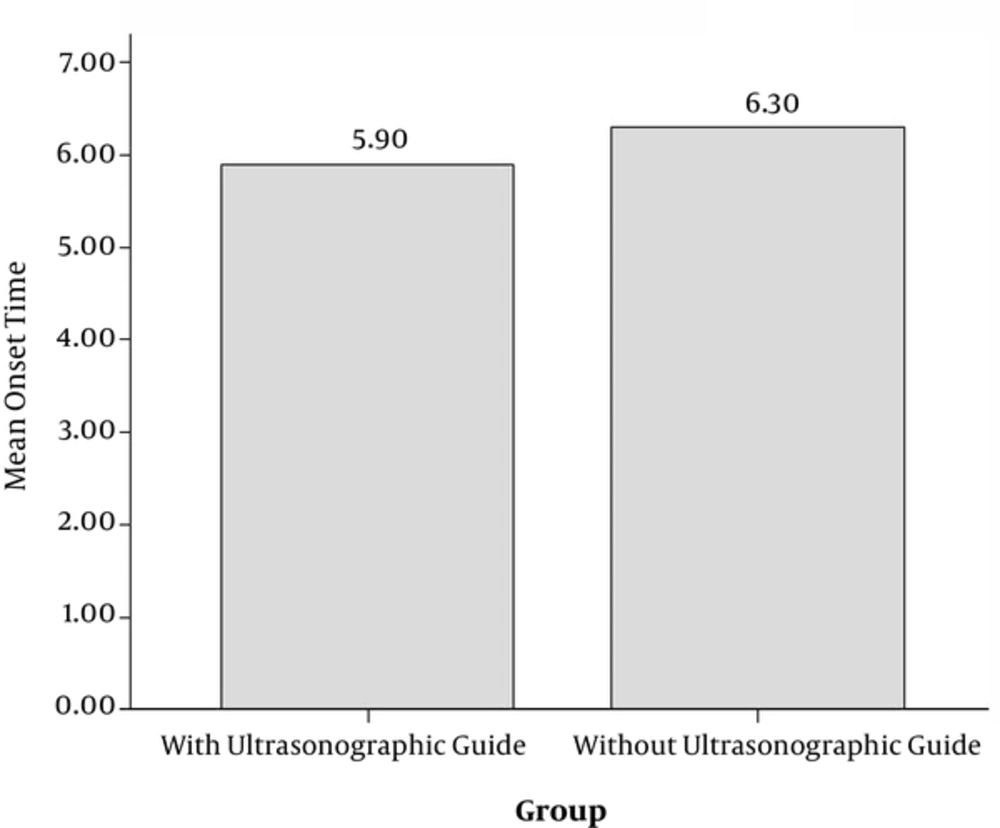
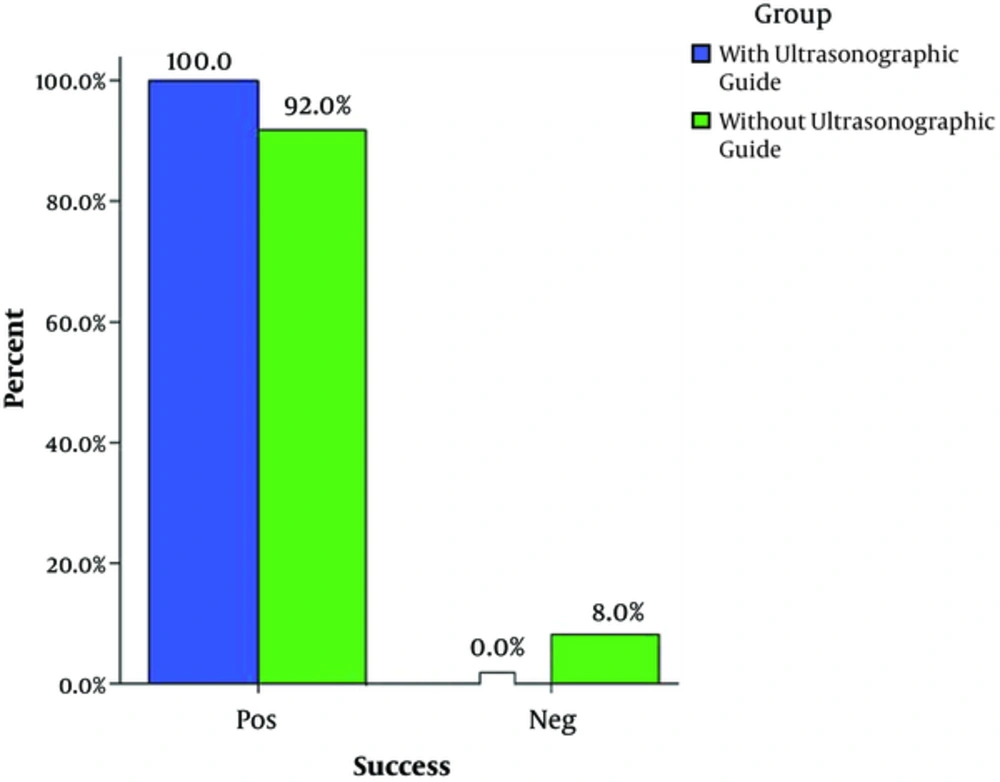
The mean age was 52.6 ± 11.8 and 53.4 ± 11.2 years in groups with and without use of ultrasonographic guide, respectively (P > 0.05). Seven (28%) and nine (36%) subjects were female in groups with and without use of ultrasonographic guide, respectively (P > 0.05). The mean duration of operation was alike (P > 0.05) between the two groups (88.6 ± 19.4 versus 92.1 ± 20.3 minutes in groups with and without use of ultrasonographic guide, respectively). So there was no statistically significant difference between these groups in general. As shown in Figure 4, although there was no statistically significant difference between the onset time in the group without guide (6.3 ± 2.2 minutes) and that in the guided group (5.9 ± 2.1 minutes), the time required for the nerve block (4.4 ± 1.3 minutes versus 1.7 ± 0.8 minutes) was significantly shorter (P = 0.001). As shown in Figure 5 the success rate in block was significantly higher in the group with ultrasonographic guide (100% versus 92%, P > 0.05).
As shown in Table 1, there were less complications in the group using ultrasonographic guide showing significant difference (P = 0.01). Limb jerking happened in four patients (16%) and bladder perforation in one (4%) in the group without sonography. There were no complications in the group with use of ultrasonographic guide. Blood loss was about < 50% ABL (allowable blood loss) without sonography (minimal), and 50 to 100% ABL in the group with use of ultrasonographic guide. No patient needed blood transfusion.

4. Discussion
The obtained results in this study demonstrated that use of ultrasonographic guide is useful to decrease the rate of complications in patients under selective obturator nerve block. It would result in lower rate of complications and is a more useful method in patients under operation for intramural tumors of urinary bladder. However, it was not assessed in our study if this method may result in higher satisfaction rate among the patients and shorter hospital stay (7).
Although it is occasionally difficult to observe obturator nerve in the ultrasound image, obturator nerve block is completed observing three muscle layers: adductor magnus muscle, adductor brevis muscle, and adductor longus muscle in the ultrasound image (7). Local anesthetics are injected between the muscle layers confirming the needle tip and spread of the solution. This technique will reduce incomplete effects or side effects of the obturator nerve block (7, 8).
The study by Seki et al. (8) in Japan among 37 subjects demonstrated that ultrasound imaging would facilitate the recognition of obturator nerves between adductor muscles as did our study. The study by Thallaj and colleagues (9) revealed that ultrasound-guided blockage of obturator nerve was successful in preventing an adductor spasm in all except one patient and patient and surgeon's satisfaction were adequate. In a single-group study among 15 subjects under ultrasound-guided blockage of obturator nerves by Akkaya et al. (10) in Turkey, it was demonstrated that ninety-three percent of the patients reported satisfaction from the block.
The study by Manassero and colleagues (11) in Italy showed that ultrasound-guided obturator nerve block may be performed after the division of the nerve and the injection of local anesthetic between the planes of the adductor muscles is equal to nerve stimulation. Helayel et al. (12), in Brazil among 22 subjects, demonstrated that ultrasound-guided obturator-nerve identification and block are technically easy and highly successful. The study by Abrahams and colleagues (13) in the United States revealed that blocks by ultrasonography guidance were more likely to be successful, took less time to perform, had faster onset, and had longer duration which is in congruence with our study.
Finally, according to the obtained results, it may be concluded that ultrasonography guidance would improve efficacy of obturator nerve block compared with conventional techniques. However, larger studies are required to determine whether or not the use of ultrasonography guidance can decrease the number of complications such as nerve injury or other complications.