1. Background
Esophageal cancer is the seventh most common cancer in the under-study populations (1). Despite the advances in radiotherapy and chemotherapy, surgery is still the main choice in the treatment of these patients (2). It can be a sustained relief for dysphagia and provide the best chance for treatment (2). There are several ways to perform esophagectomy generally divided into two groups of transthoracic and transhiatal (3). The question regarding which method of esophagectomy provides better prognosis in patients with esophageal cancer has created debates (4-6).
Supporters of the transthoracic approach believe that this method enables better visibility and better cancer resection and transthoracic lymphadenectomy, which improves the chance of survival and less risk of damage to the nerve, and it also enhances the final anastomosis (7).
Due to the differences in the epidemiology of esophageal cancer in Iran and the higher incidence of squamous cell carcinoma (SCC) compared to adenocarcinoma which is associated with more areas of the esophagus (8) and with paying more attention to radiotherapy as the standard treatment for esophageal SCC (9), it seems that transthoracic technique as s a less dangerous surgical procedure can be used more in treatment of esophageal cancer. Given the controversies in this case, Ganesamoni and Krishnamurthy showed that the survival rate of patients underwent transthoracic method was equal to or greater than and the surgical complications including damage to the recurrent laryngeal nerve and anastomotic leakage were reported less than transhiatal method (10).
2. Objectives
In this study, three-month and three-year survival rates as well as complications of transthoracic surgery were studied in patients with esophageal cancer.
3. Methods
In a longitudinal prospective case series study, all the patients with esophageal cancer who underwent surgery using transthoracic method and were hospitalized in the thoracic surgery unit of Shahid Modarres educational hospital, Tehran, Iran, during the years 2009 - 2012 were studied.
The patients’ data were extracted from the provided standard forms which were completed before and after the surgery in Shahid Modarres hospital as a referral center for esophageal cancer; the data were renewed and updated via periodical follow-ups. Totally, 34 patients entered the study.
Grading of dysphagia was done based on the standard questions in the evaluation of dysphagia (11).
The staging of tumor was done according to spiral computed tomography of thorax and abdomen with both oral and intravenous contrast and endoscopic sonography of tumor before surgery.
Twenty patients (58.8%) had the history of chemotherapy before the surgery.
All the operations were done by one surgeon. After doing preoperative evaluations, the surgery began under the general anesthesia. First, rigid bronchoscopy was done and then, right double-lumen tube was placed and thoracic esophagus was released via standard posterior thoracotomy. Thoracic lymphadenectomy was done, too. Then, in supine position, the surgery was ended after removing the esophagus and making esophagogastric anastomosis. Piloromiotomia and feeding jejunostomy was done for all the patients, too.
All the patients were moved to intensive care unit (ICU) after the surgery. Pain was controlled via intercostal nerve blockage during the surgery and in ICU. Feeding was started via jejunostomy from the second day post-surgery.
Short-term complications, length of hospitalization and anastomosis were recorded. In examining postoperative complications, leakage from the anastomosis, chylothorax, cardiac and pulmonary complications, esophagogastric anastomosis stricture and wound infection were recorded.
Patients were followed for about 4.5 years. They were visited one and two weeks after being discharged and then, during next years, all the patients or their relatives were phoned and asked about the survival status.
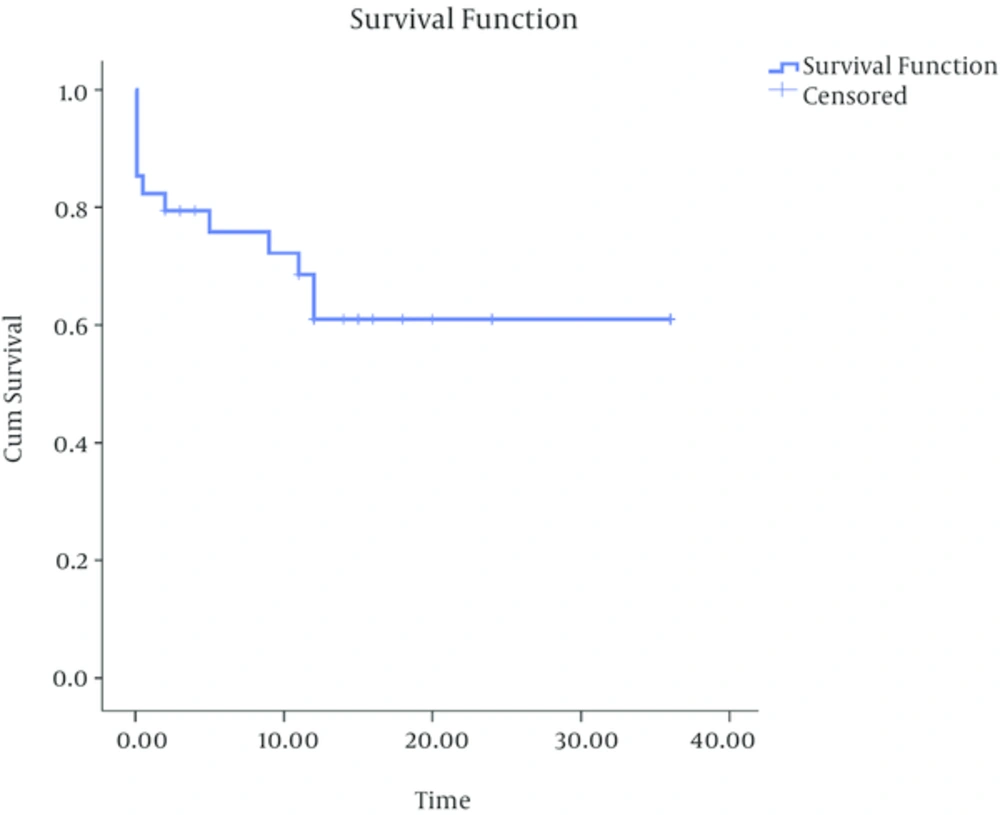
Data were analyzed using statistical tests such as Kaplan-Meier survival, the frequencies and the means via SPSS software, version 16 (SPSS Inc., Chicago, IL, and The United States).
4. Results
In this study, 23 men (67.6%) and 11 women (32.4%) with the mean age of 61 ± 10.42 years (range: 24 to 78) were enrolled. At the time of the surgery, addiction to smoking and to opium was observed in 11 (32.4%) and 5 (14.7%) patients, respectively.
In terms of dysphagia, 79.4% of the patients had dysphagia grade 3 or 4 and 17.6% had dysphagia grade II.
A history of pulmonary disease was observed in 5 patients (14.7%). In terms of the patient's blood group, 9 patients (26.5%) had blood group A, 13 patients (38.2%) had blood group B, and 12 patients (35.3%) had blood group O. In addition, 85.3% of the patients in this study were Rh positive.
The tumor was located in the middle third of the esophagus in 23 patients (67.6%), and in the lower third in 11 patients (32.4%). The mean distance of cancer from the incisor teeth was 24.4 ± 5.9 cm (range: 17 to 36).
Mean intraoperative bleeding was 654 ± 146 cc, mean time of the surgery was 408.2 ± 102.0 minutes, and mean duration of hospitalization in intensive care unit (ICU) and the ward was 6.8 ± 2.2 and 4.2 ± 1.1 days, respectively.
Regarding the histological status of cancer after resection, 28 patients (82.4%) had SCC and 6 (17.6%) had adenocarcinoma. The length of the tumor was 5.47 ± 0.86 and the diameter was 3.5 ± 0.60 cm. There was no post-resection residual tumoral tissue in 25 patients (73.5%); 7 patients (20.5%) had microscopic and 2 patients (6%) had macroscopic residual tumoral tissue.
In terms of preoperative staging in patients, most of them (58.9%) were T2, N1 (58.8%) and M0 (100%). In this study, 4 patients (11.8%) despite having negative preoperative assessments had intraoperative findings of metastasis.
Condition of the patients regarding postoperative complications is shown in Table 1.
| Complication | No. (%) |
|---|---|
| Contralateral pneumothorax | 1 (2.9) |
| Hypotension | |
| Transient | 25 (73.5) |
| Prolonged | 9 (26.5) |
| Arrhythmias | 10 (29.4) |
| Pleural effusion | |
| Right | 20 (58.8) |
| Left | 2 (5.9) |
| Both sides | 12 (35.3) |
| Vocal cord paralysis | |
| Right | 4 (11.8) |
| Left | 4 (11.8) |
| Both sides | 1 (2.9) |
6 patients (17.6%) had anastomotic leakage as delayed complication. Hospital mortality occurred in 7 patients (20.6%) and during follow up, tumor recurrence in 3 patients (8.8%) was observed; in addition, esophagogastric anastomosis stricture treated via dilatation was seen in 5 patients (14.7%). 5 patients (14.7%) also died during the long-term follow-ups.
The total survival rate of the patients within 3 years of follow-up was 61% and mortality rate (Figure 1). In this study, the three-month survival rate was 76%.
5. Discussion
In this study, the three-month and three-year survival rates of esophageal cancer in patients underwent transthoracic surgery were determined. It was shown that the three-month and three-year survival rates were 76% and 61%, respectively. In a similar study, the 5-year survival rate was 52% in transthoracic approach (10). Another similar study showed that 5-year survival rate based on the staging of the tumor, varied from 24% to 84% in patients who had surgical thoracoscopy (12). In a similar study in Mashhad, Iran, 5-year survival rate of patients with esophageal squamous cancer was 48%.9.
Anastomotic leakage occurred in 6 patients (17.6%). In the meta-analysis of Rindani et al. (13), the anastomotic leakage was seen in 10% and in Gluch et al. (5) study, in 9.1%. It was reported as 12% study on 41 patients underwent transthoracic surgery (3).
In addition, 9 patients (26.5%) had paralysis of the vocal cords following recurrent laryngeal nerve injury; of which, 4 (11.8%) were on the right side, 4 (11.8%) on the left side and 1 (2.9%) had bilateral paralysis. In Rindani et al. study, vocal cord paralysis was overall reported as 4.8%, but this measurement was done in delayed follow-ups.13 But in Niwa et al. (14) study, recurrent laryngeal nerve palsy was reported in 8% of the patients. Given that in this study, the incidence of vocal cord paralysis immediately occurred after the surgery, the higher rates of this complication can be justified. It should be noted that most of these cases had temporary paralysis and permanent paralysis was in much smaller proportion of the patients.
In our study, the macroscopic residual tumoral tissue was observed in 7 cases (20.5%) and 2 patients had macroscopic residual tumor (5.9%).
In Igaki et al study in Japan, which has similar pathology for esophageal cancer as Iran, three-field esophagectomy tended to larger survival rates because of preparing accessibility to thoracic lymph nodes (15). In the present study, the in-hospital mortality rate with transthoracic approach was 20.6% (7 cases). In similar studies, this number ranged from 9% to 13%.9 (16-18). As our hospital was a referral center for esophageal cancer and more than 30 cases of esophageal cancer were operated in this center annually, it was among the high-patient volume centers (19), so the high rate of hospital mortality can be due to the patients’ age and higher stages of the disease. In a similar survey in China, patients with higher stages of the disease who had longer postoperative hospital stay for more than two weeks had the survival of lower than five years (20). In our study, esophagogastric anastomosis stricture treated via intervention was seen in 14.7% of the patients. Similar studies reported the prevalence of esophagogastric anastomosis stricture as 26% - 42% (21). One of the most important reasons for these strictures is leakage at the site of anastomosis (22). It seems that the lower number of the cases of stricture in this study is because of the higher mortality rate. So, the patients with more risk factors of stricture were not followed.
The limitation of this study was the small sample size.
Results of the patients’ survival, and early and late complications in similar studies comparing the transthoracic and transhiatal esophagectomy were consistent (8, 23). In this study, the complications of the transthoracic techniques did not differ from other studies (14-19), and the survival of the patients without recurrence of the disease in transthoracic method was similar to those studies, too.