1. Introduction
Nowadays, with the help of new therapies, prognosis and survival rates in women with breast cancer, has been improved significantly throughout the world (1). One of the side aspects of cancer is anxiety, stress, depression and pain in these patients. Along with psychological treatments, complementary medicine has also opened its doors to new therapies. Hence, a high percentage of patients use complementary and alternative medicine (2).
Acupuncture is an evidence-based approach that has been used around the world for two thousand years. In addition to positive therapeutic outcomes, this approach is cost effective and comes with the least side effects. The studies have shown the effectiveness of acupuncture on psychological indices such as anxiety, stress, depression and improving the quality of life of women with breast cancer (2, 3). However, some studies point out the lack of effective therapeutic effect on pain (4).
On the other hand, mindfulness-based cognitive therapy (MBCT) is one of the most common types of mindfulness-based interventions (MBI) that has attracted a lot of attention in the field of cancer care and has been reported to have significant impact on the mental indices such as improving quality of life and depression (5) and pain (6) in patients with breast cancer. Meta-analysis studies show the effectiveness and safety of mindfulness-based interventions in women with breast cancer (7).
Two studies have compared the effectiveness of cognitive-behavioral therapy and acupuncture in reducing depression syndromes. The results of the study by Guo et al. (8) showed that there is no significant difference between the effectiveness of the two treatments on the depression index in patients with subsyndromal symptomatic depression (SSD). In the study by Bergdahl et al. (9), it was reported that the comparison of the effectiveness of the two treatments of auricular acupuncture and Cognitive-behavioral therapy (CBT) on depression in patients with insomnia was not significant.
Although several studies have shown the effectiveness of auricular acupuncture and mindfulness treatment independently on breast cancer, no study has addressed the comparison of the effect of acupuncture with mindfulness-based cognitive therapy in these patients.
2. Case Presentation
This study was a single-case study in the form of A1B1C1A2B2C2 design with multiple baselines and a follow-up of 6 months (Registration Code: TCTR20180605001). Data was collected during January 2015 to December 2016. The patient was a 37-year-old woman with the diagnosis of infiltrating lobular carcinoma (ILC) with metastasis invasion of axillary lymph nodes who was under oncological resection of the right breast with modified radical mastectomy and axillary lymph node dissection of 1st and 2nd level. The patient underwent chemotherapy and doxorubicin (Adriamycin) 60 mg/m2 IV + cyclophosphamide (Cytoxan) 600 mg/m2 every three weeks, as well as a dose of tamoxifen (TMX), 20 mg daily.
Inclusion criteria were: diagnosis of breast cancer (Stage 4) defined by the American joint committee on cancer, completion of chemotherapy or radiotherapy, age above 18 years, diagnosis of dysthymic disorder based on DSM criteria, ability to read and write in completing the study questionnaires and not using any psychiatric drug or receiving psychological interventions in the three months leading up to the study. Exclusion criteria were including: psychiatric disorders such as schizophrenia, auditory tissue injury, or mental retardation that prevents sitting for 40 minutes.
Preliminary evaluation was carried out 28 days prior to the registration of the baseline included an electroencephalograph examination, blood and urine tests by a team consisting of a psychiatrist, two clinical psychologists, and a nurse. Acupuncture was performed twice a week for three weeks (six sessions) and was conducted in the form of sessions of 30 to 45 minutes before lunch. During the session, five ear points called sympathetic, Shen Men, kidney, liver and lungs were interfered. Acupuncture in both ears was performed using one-use stainless steel needles (13 mm + 0.25 mm) with a depth of 2 - 3 mm by a trained physician and acupuncturist with a degree and five-year history of treatment (Second author, K. P.). The MBCT is a combination of MBSR and cognitive-behavioral techniques, including psycho education, exercises and cognitive restructuring, and developing pleasant activities. This treatment was provided to the subject for three weeks (two sessions per week) and each session for two hours.
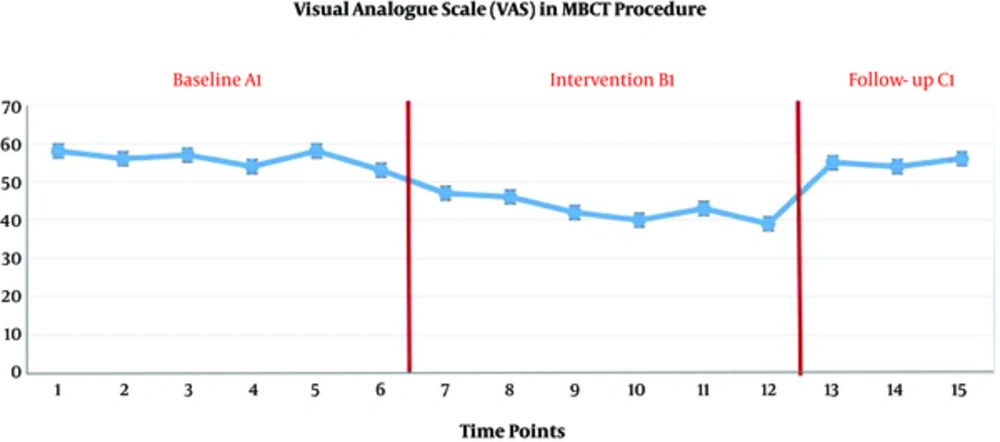
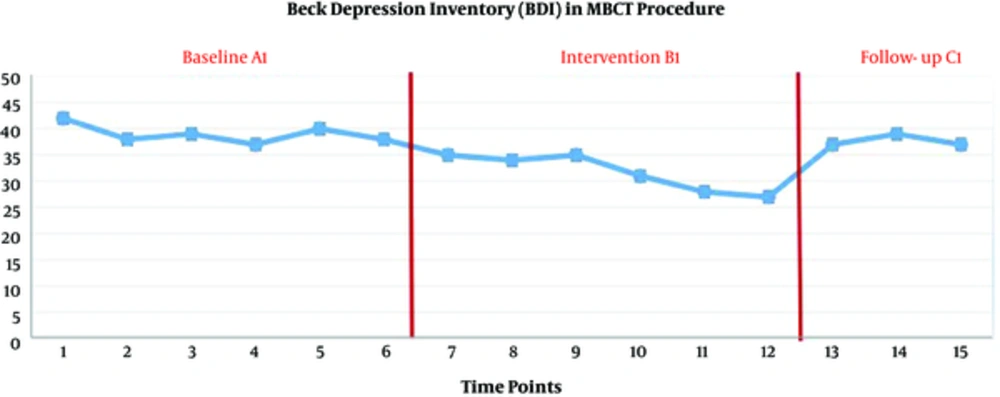
In baseline A1 and A2 (three weeks, six evaluations), only the evaluation was carried out, and no interventions were made. In phase B1 (three weeks) and B2 (three weeks), acupuncture and mindfulness-based cognitive therapy were presented, respectively. The interval between the two phases of intervention was 6 months and the six-month follow-up (C1 and C2) was done. The entire study period was 15 months and 30 evaluations were carried out. In order to collect data in this study, a structured clinical interview (SCID), researcher-made demographic questionnaire, visual analog scale (VAS) and Beck depression inventory (BDI) were used. All the data of this study were collected after agreement with the patient, and informed consent was received before the intervention and publication, and all stages of the study were based on the latest version of the Helsinki declaration. The data were analyzed using a single case study design model protocol.
The scores of visual analogue scale showed a significant decrease during the three weeks of acupuncture (B1) (P < 0.05), although this reduction was not maintained in the follow-up stage (P > 0.05). But the scores of depression index did not decrease significantly during the three weeks of acupuncture (B1) (P > 0.05).
The scores of visual analogue scale and depression in three weeks of baseline (A1), three weeks of mindfulness-based cognitive therapy (B1) and three evaluations in a six-month follow-up (C1) are presented in Figures 1 and 2.
The scores of visual analogue scale decreased significantly during the three weeks of mindfulness-based cognitive therapy (B1) (P < 0.05), although this reduction was not maintained in the follow-up stage (P > 0.05). The scores of depression index decreased significantly during the three weeks of mindfulness-based cognitive therapy (B1) (P < 0.05), although this reduction was not maintained in the follow-up stage (P > 0.05).
3. Discussion
The present study was the first study to compare the effectiveness of mindfulness-based cognitive therapy with acupuncture on pain and depression indices. The findings of this study showed that the acupuncture treatment was effective in pain relief and mindfulness-based cognitive therapy on both pain and depression indices were effective, although changes were not maintained until the follow-up stage. In line with our findings, the results of Park et al. (5) and Johannsen et al. (6) suggest the effectiveness of mindfulness-based cognitive therapy to reduce depression and pain. Contrary to the findings of the present study, the results of Pirnia et al. (4) suggest the ineffectiveness of auricular acupuncture on pain relief in a patient with trismus. On the other hand, the results of Pirnia et al. (10) showed that acupuncture was accompanied by a decrease in the back pain in colon cancer. Our findings are also in contradiction with the results of study by Guo et al. (8) and Bergdahl et al. (9), which reported the difference in the effectiveness of the two medical treatments of auricular acupuncture and cognitive therapy on depression. Cognitive-behavioral therapy can significantly reduce depression syndromes. This effect can be explained by the effect on the component of psychological stress mediator, which in the present study showed a significant reduction in cognitive-behavioral therapy.
In the present study, acupuncture had no significant effect on depression. Contrary to these findings, the results of Ormsby et al. (11) showed that the use of acupuncture is useful in women with postpartum depression. In the explanation of the ineffectiveness of acupuncture, it can be acknowledged that acupuncture efficacy is not only dependent on the duration of the needle keeping but may be dependent on several factors (2). However, more controlled studies are needed to confirm these findings. Future studies can be considered in combination of two treatments to increase the effectiveness of physical and psychological indices. Also, a controlled clinical trial is a good route for future studies.