1. Background
Brachytherapy is an integral component of the definitive treatment of locally advanced cancer cervix. It is usually started after external beam radio therapy (EBRT) to give curative doses to the tumor and limit doses to the nearby organs at risk (OAR). Several studies have shown decreased recurrence rates and improved survival when brachytherapy is used (1).
Cervical Brachytherapy has evolved from the time when dose prescription was largely empirical, to the image based conformal Brachytherapy advocated by Groupe Europeen de Curie Therapie-European society for therapeutic radiology and oncology (GEC-ESTRO) and American Brachytherapy Society (ABS). MRI is the preferred imaging modality although CT scans are commonly used to delineate the target and the surrounding organs at risk (OAR) (2, 3).
MRI has the advantage of superior anatomy and tumor recognition but has its drawbacks like expensiveness, requirement of suitable applicators, and difficult access for many clinical centers. These drawbacks make it necessary to find alternative imaging modalities that provide similar image quality as MRI but to find one that is more easily accessible and affordable. Ultrasound (USG) is an inexpensive imaging modality that offers good soft tissue information and is widely available. Trans abdominal USG can determine uterine size, shape thickness, and diameter. There are studies that show good comparability between USG and MRI in the measurement of uterus and cervix (4, 5).
The department of radiotherapy, Dr. S. N. medical college, Jodhpur, India has traditionally practiced 2D orthogonal X-ray image based HDR Brachytherapy (Multisource HDR remote afterloading unit with a 60Cobalt radionuclide source) with dose prescription to point A. The USG machine in the brachytherapy operation theatre has been used to guide tandem application.
2. Objectives
Our present study was an attempt to use USG imaging in the brachytherapy planning (dose prescription) process in a small set of patients and to evaluate in terms of dosimetry, local disease response and toxicity.
3. Methods
Twenty-five patients with locally advanced, histo-pathologically proved squamous cell carcinomas of the cervix, (FIGO 2009 stage IB2-IIIB) attending our department (January to September 2014) for intracavitary brachytherapy (ICBT) were studied. Other inclusion criteria were: Age < 70 years and > 18 years, eastern co-operative oncology group (ECOG) performance status (0 - 1 - 2), adequate baseline organ function (hematological, renal and liver function test and Cardiac status), written informed consent, gynecologic anatomy suitable for intracavitary application and normal Chest X-Ray. Exclusion criteria were: previously treated cases, second malignancy, distant metastasis, prior radiation to pelvis, associated co-morbidities including gastro-intestinal disorders, narrow conical vagina and evidence of para-aortic lymphadenopathy on USG of abdomen and pelvis. This was a single arm prospective study. The study protocol was approved by the institutional ethical committee. All patients had received definitive 50Gy/25# External Beam Radiotherapy (EBRT) (with concurrent chemotherapy) to the pelvis.
Brachytherapy procedure was done in mini operation theatre under intravenous conscious sedation. Patients were positioned in lithotomy position for applicator insertion. Pelvic examination was done to assess disease status, size of cervix and fornices, and to determine the size of vaginal ovoid. A Foley’s catheter was inserted. The balloon was filled with 7 mL diluted contrast and positioned against the bladder neck. An enema was done prior for an empty rectum. The uterus was sounded to ascertain the required length of the tandem and the cervical canal dilated. The selected tandem and the ovoids were inserted under USG guidance. Vaginal packing was done using gauze soaked with radio opaque solution diluted with normal saline. Orthogonal radiographs (Antero Posterior and Right Lateral) were taken (by a C-Arm X-Ray Machine) in the supine position and transferred to treatment planning system (HDR Plus Version 2.5.3.) for reconstructing the applicator position and geometry.
Two plans were generated at each Brachytherapy session of the patient: (i) a standard orthogonal X-Ray based plan with dose prescribed to Point A which was 2cm superior and lateral to the most inferior source loading position in the central tandem. Doses to international commission on radiation units and measurements (ICRU) 38 bladder and rectum reference points were noted and optimization was done to keep the doses at these points below 75% of the point A dose (7.5Gy/fraction).
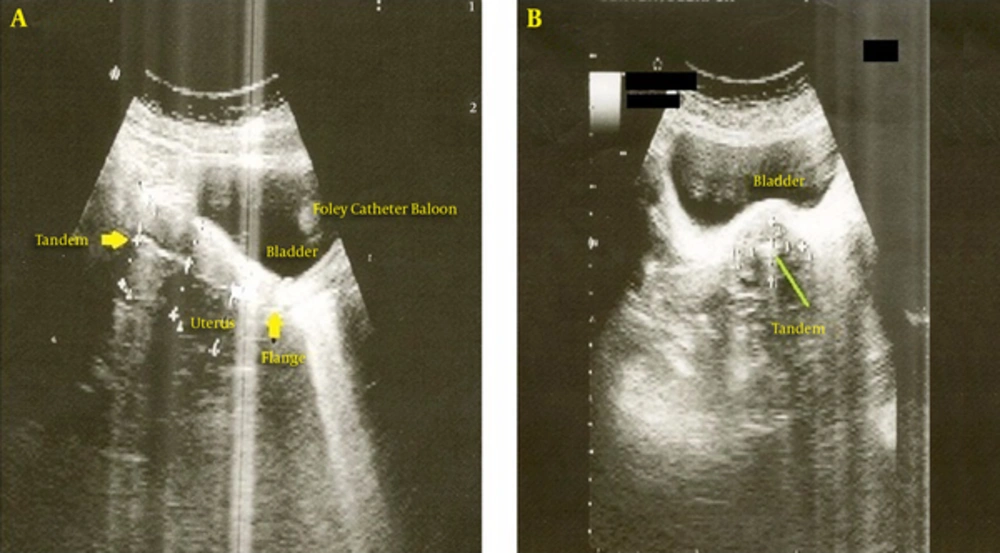
(ii) a USG based plan with details as follows: the patient had ultrasound imaging in the treatment position with the legs resting on the table. Around 250 mL normal saline was infused into the bladder. After ensuring that the tandem was centered within the uterus, tandem to uterine surface measurements in the sagittal and transverse planes were obtained. Measurement of distances between the central tandem and the anterior and posterior surfaces of the uterus were taken starting at cervical os, at 2 cm and at 4 cm from the os, and from the tandem tip to the uterine fundus (Figure 1A) by the radiologist in the brachytherapy O.T. Measurements in the axial plane were also taken at the above points (Figure 1B). USG based plans were derived based on clinical assessment of the disease (residual in cervix and vagina) at the time of brachytherapy and the observed dimensions of the uterus and cervix in USG views. A dose of 7.5Gy was prescribed to the perimeter of the USG defined target (plus the fornices observed clinically/radiologically represented by the ovoids) by manipulating the tandem and ovoid dwell weights. Traditional dose points at Point A were used to start optimization.
All patients received three fractions of HDR ICBT (7.5 Gy/Fraction). Actual brachytherapy doses were prescribed to the USG (and clinically) delineated target. Doses received at point A, ICRU 38 Bladder and Rectal points in the USG and standard X-ray plans were noted. The total doses received (EBRT + during 3 fractions of Brachytherapy) in 2Gy Equivalent Fractions i.e. EQD2 doses for the above reference points were calculated (by linear quadratic equation/LQ spreadsheets) for the two plans. Biologically effective doses (BED) for total radiation received (EBRT + ICBT) at bladder and rectal points were also calculated. The α/β ratio of 3 was taken for late complications.
The EQD2 and BEDs of the USG and Standard X-Ray plans were compared using paired-sample t tests (using SPSS Statistics 17), statistical significance considered at P value < 0.05.
All patients were assessed during every brachytherapy session and subsequent follow up at 1st, 3rd, 6th, 9th, 12th and 15th month for tumor response [WHO criteria] and normal tissue toxicity [radiation therapy oncology group (RTOG) criteria].
4. Results
The majority of the patients came from rural areas belonging to lower socio-economic strata. Patient characteristics were as follows (Table 1):
| Characteristics | (n = 25) |
|---|---|
| Mean Age (range) | 53 y (35 - 67) |
| ECOG Performance Status (PS) | 1 = 22 |
| 2 = 3 | |
| FIGO Stage | |
| IB2 | 2 |
| IIA | 1 |
| IIB | 10 |
| IIIA | 1 |
| IIIB | 11 |
| Histopathological Differentiation | |
| Well differentiated | 5 |
| Moderately differentiated | 12 |
| Poorly differentiated | 8 |
| Mean Hemoglobin level, g/dL | 10.48 |
| Mean Blood Urea level, mg/dL | 27.72 |
| Mean Serum Creatinine level, mg/dL | 1.00 |
Patient Characteristics
4.1. Comparison of Standard X-Ray and USG Image Based Plans
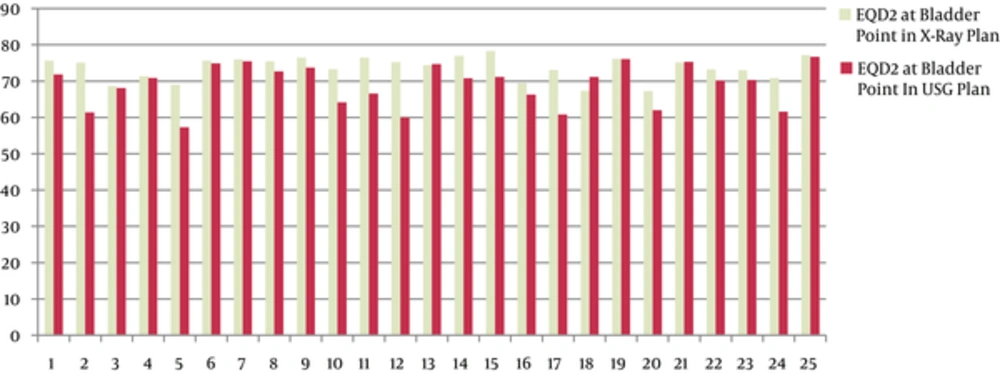
The mean EQD2 (Table 2) at point A in the USG and X-Ray plans were 78.61Gy and 82.39Gy, respectively. The mean EQD2 at ICRU 38 Bladder points (Figure 2) were 68.95Gy and 73.62Gy, respectively; and at ICRU 38 Rectal points were 68.96Gy and 72.22Gy, respectively for the two plans. There was a statistically significant difference between the two plans (USG and Standard X-ray) regarding: point A dose (P < 0.001), EQD2 at point A (P < 0.001); Bladder point dose (P < 0.001), EQD2 at Bladder point (P < 0.001) and Rectal point dose (P = 0.004), EQD2 at Rectal point (P < 0.002).
| Doses to | USG Plan | X-Ray Plan Value | P Value |
|---|---|---|---|
| Mean (Range) | Mean (Range) | ||
| Point A (EQD2) | 78.61Gy | 82.39Gy | < 0.001 |
| (72.6 - 89.1) | (77 - 82.9) | ||
| Bladder Point (EQD2) | 68.95Gy | 73.62Gy | < 0.001 |
| (57.61-76.72) | (67.26 - 78.3) | ||
| Rectal Point (EQD2) | 68.96Gy | 72.22Gy | 0.002 |
| (60.9 - 76.39) | (63.95 - 80.71) |
Comparison of Ultrasound (USG) and X-Ray Plans
The mean BED at bladder and rectal points were 115.96Gy3 and 115.63Gy3 in the USG plans. In the standard X-ray plans, mean BED at bladder and rectal points were 122.21Gy3 and 119.88Gy3 respectively. Hence, the patients received lower mean BED at the OARs than they would have received by standard orthogonal X-ray planning.
4.2. Treatment Response and Toxicity
At the end of treatment (EBRT+ICBT), (Table 3) complete response (CR) rate was 76% and 6 patients (24%) had a partial response (PR). At 15 months of follow up, disease free status was achieved by 73.68% of patients. Four patients had pelvic recurrence and one had both pevic and distant (lung) failure. 6 patients were lost from follow up. In 15 months, 2 patients had Grade 1 Bladder toxicity. No higher grades of bladder toxicity were seen. 3 patients had Grade 1 and 1 had Grade 2 Rectal toxicities at 15 months. Grade 3 and 4 bladder/rectal toxicities were not observed.
| Response and Toxicity | ||
|---|---|---|
| Genitourinary/Bladder toxicity | Gr 1 | 2 |
| RTOG criteria (15 mo) | Gr 2 | 0 |
| Lower GIT/ Rectal Toxicity | Gr 1 | 3 |
| RTOG criteria (15 mo) | Gr 2 | 1 |
| Response at End | CR | 19 |
| Of Treatment | PR | 6 |
| (WHO criteria) | SD | 0 |
| PD | 0 | |
| Disease Free Follow Up (15 mo) | 14/19 (73.68%) | |
Disease Response and Toxicity
5. Discussion
The present study aimed at utilizing a commonly available imaging modality (i.e. ultrasound for cervical brachytherapy at resource limited centre). Doses to OARs (bladder and rectum) could be reduced. Disease response and adverse effects were comparable to those available in literature (6-8).
The use of Radium sources for brachytherapy treatment of uterine cervix started in 1903. Early dosimetric systems like the Stockholm and Paris systems specified dose prescription in terms of fixed number of milligram/hours (the amount of radium in the applicators, loading arrangement and treatment duration) and ignored anatomical targets and tolerance organs (2).
Tod et al. formulated the Manchester system in 1938 (modified 1953) establishing the concept of Point A (originally defined as a point 2 cm lateral to the centre of the uterine canal and 2 cm from the mucous membrane of the lateral fornix in the plane of the uterus) and the para-cervical triangle. They were of the view that radiation necrosis was not the result of direct effects of radiation on the bladder and rectum, but high dose effects in the area in medial edge of the broad ligament where the uterine vessels cross the ureter. It was considered that the tolerance of this para-cervical triangle was the main limiting factor in the irradiation of uterine cervix and they used point A exposure to represent its average dose. This concept of dose prescription to a single point (point A), simplicity, comparability and reproducibility made this system the most acceptable brachytherapy technique (9).
However, point A is an empiric point and does not reflect dose to the tumor as the tumor itself is not imaged. The international commission on radiation units and measurements (ICRU) 38 which in 1985, gave the concept of urinary bladder and rectal reference points, recommended that reference points such as point A should not be used because such points are located in a region where the dose gradient is high and any inaccuracy while placing this points during planning would result in large uncertainties in the absorbed dose at these points. It instead recommended that doses should be specified in terms of a reference target volume which is the tissue volume encompassed by a reference isodose surface of 60 Gy (10).
Point A dosimetry gave a fixed distribution irrespective of the anatomy of the pelvis or tumour target which varies from individual to individual. So Point A may lie inside or outside the actual target volume. One may end up giving a large dose to the surrounding organs or providing inadequate coverage in case of a larger target because the tumor is not visualized.
With the widespread availability of imaging techniques (computed tomography, magnetic-resonance imaging and even positron emission computerized tomography), which allowed visualization of tumor and its extent, the pelvic organs including the surrounding organs at risk (OAR), emphasis on image based brachytherapy started.
These new imaging techniques and the development of CT or MRI compatible intracavitary brachytherapy (ICBT) applicators have allowed radiation oncologists to shape the dose distribution to conform to the target volume and reduce the dose to normal tissues. This has made it possible to decrease the probability of normal tissue toxicity and to escalate the dose to the tumor to produce greater rates of local control. The Groupe Europeen de Curietherapie and European society for radiotherapy and oncology (GEC-ESTRO) have been instrumental in advancing the use of soft tissue imaging particularly MRI (3).
In cervix brachytherapy, ultrasound is primarily used to ensure safe applicator placement. In the study to determine if transabdominal USG can be used for conformal brachytherapy in cervical cancer patients, Narayan et al. (5) treated seventy-one patients of locoregionally advanced disease with a minimum follow-up of 2.5 years. They observed 90% local control at 2.5 years. Late morbidity (RTOG grade 3, 4) was < 2%. The study showed that plans based on USG images were not significantly different from those generated by MRI. However, the USG plans had statistically significant differences (P < 0.001) in terms of doses received at point A, ICRU 38 Bladder and Rectal points when compared with standard X-Ray plans. The authors concluded that USG imaging in ICBT can substantially reduce doses to organs at risk while not compromising dose to the target volume.
Similar results were obtained in our study which used similar methods of USG image based target delineation. Statistically significant reduction in EQD2 at point A, ICRU 38 Bladder and Rectal points were achieved in the USG plans. The disease response rates and toxicity in our study were comparable to other studies with short follow up (6-8). The BEDs at bladder and rectal points were lower in our study compared to these.
To assess the potential value of US for image-guided cervical cancer brachytherapy, Umesh Mahanshettty et al. (11) compared US-findings relevant for brachytherapy to the corresponding findings obtained from MR imaging. They studied twenty patients (thirty-two applications) using nine reference points identified with respect to central tandem and flange, to delineate cervix, central disease, and external surface of the uterus. They concluded that USG had a reasonably strong correlation with MR in delineating uterus, cervix, and central disease for 3D conformal intracavitary brachytherapy planning.
Another paper by S Van Dyk et al. (192 patients, 1668 measurements of the cervix and uterus) studied images obtained by MRI and transabdominal ultrasound in the longitudinal axis of the uterus with the applicator in treatment position. Measurements were taken at the anterior and posterior surface of the uterus at 2.0-cm intervals along the applicator, from the external os to the tip of the applicator. Differences in the measurements of the cervix and uterus obtained by MRI and ultrasound were within clinically acceptable limits. They concluded that transabdominal ultrasound can be substituted for MRI in defining the target volume for conformal brachytherapy treatment of cervix cancer (4).
Epstein et al. reported the results of a European multicenter study comparing Transvaginal Scans (TVS) and MRI for delineating cervical tumor. These results showed that TVS was superior to MRI in both women with and without cone biopsy prior to surgery (12). Schmid et al. discussed using transrectal ultrasound (TRUS) to assess cervix cancer during radiation therapy (13). The cervix was examined in 17 patients using TRUS and the findings compared with those of MRI. A good agreement was found between the two modalities. A review by Juan Luis Alcazar observed that ultrasound may be a useful technique for assessing local extent of disease in cervical cancer, even with higher accuracy than MRI. This modality had limitations in assessing lymph nodes. USG could be useful for monitoring and predicting response to therapy (14).
Ideally, an imaging modality should be available for each brachytherapy insertion; it should be performed intraprocedurally, offer good organ and applicator definition, and be able to delineate residual tumor. USG fulfills most of these criteria although it has its limitations like the need of experienced operators, familiarity with applicator geometry and pelvic anatomy to ensure that images reflect the true dimensions of the applicator within the anatomical organ.
Long term results of a large study at Melbourne (292 patients) (15) using transabdominal USG guided conformal HDR brachytherapy reported five-year failure free survival and overall survival (OS) at 66% and 65%, respectively. Primary, pelvic, para-aortic, and distant failure were observed in 12.5%, 16.4%, 22%, and 23% of patients, respectively. Local control (87.5% in the study) was comparable to 89% in 2 years, 95% in 3 years, and 91% in 3 years as reported by Haie-Meder et al, Potter et al. and Lindegaard et al. respectively. All had used MRI based conformal brachytherapy using GEC-ESTRO recommendation. Kailash Narayan et al. (15) concluded that real-time imaging and treatment planning using USG would make this a method of choice for treating cancer cervix in most parts of the world where cancer cervix remains a major health problem and MRI is inaccessible.
Ultrasound image based brachytherapy could achieve significant reduction in doses at OARs. Locoregional control and treatment complications in our study were within acceptable limits. A clearer picture can only be obtained with larger study size and longer follow up. Ultrasound imaging’s potential as an imaging modality for conformal brachytherapy should be further explored, especially for high disease burden and low resource settings.