1. Background
Thyroid nodules are common clinical issues, and incidence of differentiated thyroid cancers have increased in recent years (1). Epidemiologic studies have delineated that prevalence of thyroid nodules in men and women are 1% and 5% respectively in non-Iodine deficient areas (2). The first measure for evaluation of Thyroid nodules is fine needle aspiration (FNA). In majority of cases (60% - 70%), the nodules are benign and need no further work up (3, 4). In 2007, Bethesda system categorized cytopathology reports of FNA specimens in six subgroups (3). The category III was defined as atypia of undetermined significance or follicular lesion undetermined significance (AUS/FLUS) including specimens without either enough features for malignancy or benign lesion. Although some authors suggest that diagnosis of AUS/FLUS should be no more than 7 % of all the FNA specimen of Thyroid nodules (5), patients with AUS/FLUS reports are increasingly present in surgical outpatient clinics (6). Prevalence of malignancy among AUS/FLUS shows a wide range in different studies (6% - 48%) (7). In Bethesda system, malignancy rate of AUS/FLUS is 5% - 15%; therefore, Bethesda’s recommendation for AUS/FLUS is to repeat FNA and manage the patient by new FNA report (3). However, American Thyroid Association mandates surgery for AUS/FLUS nodules with Hurthle cell (8). American clinical endocrinologist association and European thyroid association guideline suggests surgery for most Bethesda category III and IV (9). The management of nodules with AUS/FLUS is controversial based on routine recommendations and guidelines.
2. Objectives
Thus, the aim of the present study was to outline diagnostic value of repeated FNA in nodules with AUS/FLUS reports in patients with thyroidal nodules.
3. Methods
This prospective trial was done in Isfahan in 2013 - 2014. The study protocol was approved by institutional medical ethics committee (number: ir.mui.rec.1393.3.102). The target population of this study consisted of the patients with thyroid nodules who had been hospitalized and underwent thyroid surgery. There were, however, some inclusion criteria, i.e. the candidates had a thyroid nodule with AUS/ FLUS diagnosis by cytopathlogical examination, who underwent thyroid surgery (either near total thyroidectomy or lobectomy-isthmectomy) based on clinical findings, ultrasound features, and patient's preference. All the patients filled a written consent form after a fully-informative educational session.
As for procedures, in the operating room after induction of anesthesia and skin incision, the strap muscles were retracted and under direct vision by using a 25 or 27 gauge needle and a 10 cc syringe, for each performance we made three back and forth oscillations in the duration of one second. Slides were prepared by expelling and smearing the cells on the slides. The specimen was sent for cytopathology evaluation after fixing the slides with 96% ethanol. Moreover, permanent pathology examinations were performed via routine methods and H&E staining.
Furthermore, demographic information including age, sex, past history, radiation exposure, family background, nodule’s characteristics, repeated FNA result and post-operative permanent pathology results were collected. The obtained data were analyzed by SPSS software, version 22, and statistical T tests, T student, and Chi-square tests were employed to determine the sensitivity and specificity of each FNA test.
4. Results
In this study, 50 patients with AUS/FLUS thyroid nodule, with the mean age of 39.64 ± 13.3 years (range 15 - 73) were studied. Among them, 37 (74%) patients were under the age of 50 and 13 patients (26%) were 50 years of age or above. 5 candidates (10%) were men and 45 (90%) were female. The mean period of time between the onset of the symptoms and operation was 6.7 months, and the most common symptom was voice hoarseness with the frequency of 14 (28%) cases. Also, 13 patients (26%) had a previous history of thyroid disease, 1 patient (2%) had undergone a partial thyroidectomy, 25 patients (50%) took thyroid medication, and 6 patients (12%) had a family history of thyroid diseases. In Table 1 below, the distribution of demographic variables is shown:
| Variable | Number/Average | S.D |
|---|---|---|
| Age | 13.3 | |
| Mean | 39.64 | |
| Under 50 years | 37 (74) | |
| 50 years and more | 13 (26) | |
| Sex | ||
| Male | 5 (10) | |
| Female | 45 (90) | |
| The onset of symptoms | 6.7 | |
| Mean (month) | 20.52 | |
| Under 12 months | 14 (28) | |
| 12 months and more | 36 (72) | |
| Clinical signs | ||
| Hoarseness | 14 (28) | |
| Dyspnea | 11 (22) | |
| Dyspnea | 11 (22) | |
| Cough | 3 (6) | |
| Dysphagia | 4 (8) | |
| Mass | 41 (82) | |
| Neck adenopathy | 1 (2) | |
| Previous history of thyroid disease | 13 (26) | |
| History of thyroid surgery | 1 (2) | |
| Taking Thyroid medication | 25 (50) | |
| Family history of thyroid disease | 6 (12) | |
| History of radiation | 0 |
aValues are expressed as No. (%).
According to the surgical findings related to the number of thyroid nodules, 46% of the patients had 1 nodule, 40% had 2 nodules, 6% had 3 nodules, and 8% had more than 3 thyroid nodules. As for the nodules size, 10% of them were less than 1 cm, 40% were 1-3 cm and 50% were more than 3 cm.
Pathological examination of the samples revealed that in all the participants, 14 cases (28%) were benign and 36 cases (72%) were malignant while repeated FNA results showed 13 malignant and 15 benign cases, with 22 cases undetermined. All the patients with malignant result of repeated FNA showed malignant reports as well in permanent pathology specimen (n = 13). Among 15 patients with benign repeated FNA, 7 cases had benign and 8 cases had malignant reports on permanent pathology. In 22 patients with repeated report of “undetermined” in re-FNA, 7 subjects were benign while 15 of them were malignant in permanent pathology (Table 2).
| First FNA | ReFNA | Permanent Pathology | |
|---|---|---|---|
| Malignant | Benign | ||
| AUS/FLUS + benign | 15 (30) | 8 (16) | 7 (14) |
| AUS/FLUS + malignant | 13 (26) | 13 (26) | |
| AUS/FLUS + AUS/FLUS | 22 (44) | 15 (30) | 7 (14) |
| Total | 50 (100) | 36 (72) | 14 (28) |
aValues are expressed as No. (%).
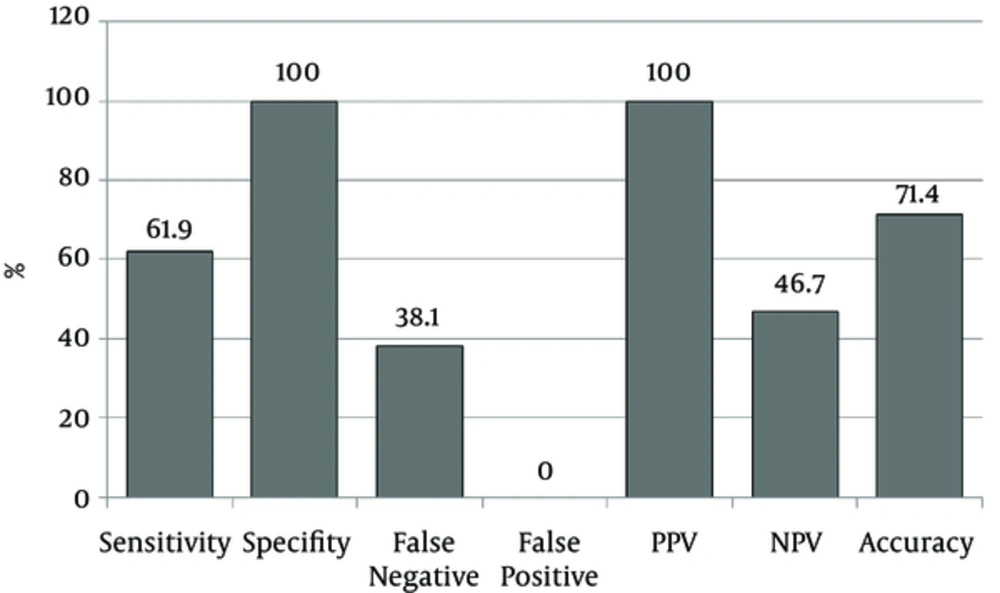
Based on the results, the repeated FNA test sensitivity was 61.9% and specificity was 100%, 0% false positive and 38.1% false negative. Also, according to the results, the positive and negative predictive value of repeated FNA were 100% and 46.7% respectively, and the accuracy of the repeated FNA test was reported as 71.4% (Figure 1).
5. Discussion
BSRTC (The Bethesda system for reporting thyroid cytopathology) is precise, and lays down clear communication between cyto-pathologists and surgeons. Thus, it should help clinicians in decision making. Diagnosis of AUS/FLUS, however, can be primarily difficult to interpret and manage from a clinical standpoint. There is some controversy over the management of this category (type III) as to repeating FNA or clinical observation, direct triage surgery. In the present study, the patients with AUS/FLUS, who were candidate for surgery due to clinical, radiological feature or patient preference, were selected. Intraoperative FNA from relevant nodules was done. Pathology and repeated FNA results were evaluated. The evaluation showed that re-FNA has low sensitivity and specifity and therefore, cannot be helpful for decision making for all patients.
The recommended approach to an initial AUS/FLUS diagnosis is to repeat FNA within 3 - 6 months (5), perhaps due to the increase in false positive rate and atypical chances in follicular cells with Re-FNA before 3 months (10). Also, surgical resection is recommended for patients with a repeated AUS/FLUS or follicular neoplasm, suspicious for follicular neoplasm or suspicious for malignancy or malignant diagnosis. Wong et al. (11) have reported the malignancy rate at first FNA as 25.6% and with re-FNA as 38.8%. They believe that repeated FNA is necessary for better selection of patients for surgery.
The proposed guideline has some disadvantages, i.e. although re-FNA diagnosis is more precise, about 20% - 25% of nodules repeatedly receive the results of AUS/FLUS (12) which end up with inaccurate judgment. Also, the malignancy rates associated with AUS/FLUS with or without repeat FNAB have been reported with variable results in different series (7, 11, 13-19).
Malignancy rate in thyroidectomy patients is different in literature (14% - 41% for single FNA and 29% - 52% for re-FNA). This rate between first FNA and re-FNA is, at the same time, unpredictable. Thus, great efforts have been made to remove the limitations of AUS/FLUS.
Chen (2014), in a study of 76 AUS/FLUS cases found out that certain cytological features warrant strong consideration for thyroidectomy instead of the routine repeat FNAB. He suggested that a high degree of cytological atypysm can guide to manage patients with AUS more aggressively. He concluded that such patients should forego repeat FNAB and undergo thyroidectomy.
It is to be noted that there is some controversy here since the management of AUS/FLUS relies on ultrasonography future of nodule. Lee et al. (2015) (20) in a study of ultrasonographic features of 213 AUS/FLUS cases recommended that diagnostic Thyroidectomy may be preferable in patients with suspicious ultrasonography features after cytopathology diagnosis of AUS/FLUS without repeat FNA. Paul et al. (2011) reported malignancy rate in AUS/FLUS with single FNA as 41% and with re-FNA as 43%, without any significant difference. So they stated that AUS/FLUS has moderate risk of malignancy and re-FNA guideline should be re-evaluated (18).
In another study on 58 AUS/FLUS cases, Park et al. (2015) (21) concluded that ultrasonographic findings in two consecutive AUS/FLUS are not helpful for the omission of surgery, meaning that surgery should be done without any attention to US findings. Also, Nagarkatti et al. (14) found that among resected patients with AUS/FLUS, malignancy rates were 15.3% and 16% for patients with and without repeat FNAB, respectively. Broome et al. (19), too, reported that malignancy rates with and without repeat biopsy were not significantly different in patients who have indications for thyroidectomy, regardless of AUS/ FLUS results, and concluded that repeat FNAB did not appear necessary. On the other hand, repeat biopsy was underutilized in AUS /FLUS cases. Ho et al. (7) reported that out of the 541 nodules with AUS/FLUS cytology, 350 nodules underwent immediate surgery with a malignancy rate of 39%, that is, more than BSRTCT.
The potential usefulness of molecular testing in these AUS/FLUS cases is, however, doubtful. Some authors suggest that molecular testing of thyroid nodules does not significantly alter the surgical management of the patients (22, 23).
In the present study, the malignancy rate of re-FNA is 26%, which is in line with that of other studies. The undetermined rate with re-FNA is 44%. Benign result with re-FNA is 16%, but 7 (53%) of these patients grew malignancy after surgery.
5.1. Conclusion
FNA of patients with thyroid nodules is not a reliable method in diagnosing the identity of nodules. It can just be used as a primitive method of screening. However, a definite diagnosis is only possible through pathological analysis of FLUS biopsies because FNA cannot help to be suspicious of malignancy. Based on the findings of the present study, surgery is the most appropriate recommendation with repeated FNA before thyroidectomy, on the basis of clinical findings and ultrasound results.