1. Background
Invasive breast cancer is a heterogenous disease. This is important about responses to therapy. Invasive ductal carcinoma (IDC) is the most common type of breast cancer and accounts for 70% to 80% of them (1). Invasive lobular carcinoma (ILC) and mixed type (IDC+ILC) constitute 5% to 15% and 3% to 5%, respectively (1).
ILC is a distinct pathology that differs from IDC in risk factors, histologic features, genomic profiles, immunophenotype, and response to systemic therapy (2). Besides, ILC typically does not destroy anatomic structures or stimulate tissue responses. Thus, there is no clinically palpable mass and mammographic appearance is indistinct. Again, ILC has greater tendency for multicentricity and mulifocality (3, 4). In fact, the extent of the disease can be underestimated. There is concern with local therapeutic approaches such as, accelerated partial breast irradiation (APBI) (5, 6). It should be remembered that the reliable margin is one of the most important intraoperative radiotherapy (IORT) selection criteria.
Accordingly, ILC is placed as a cautionary criteria in the American and the European guidelines for IORT (7, 8).
The incidence of ILC is increasing (9, 10). Nevertheless, although ILC tumor size is slightly large, that is found in elderly women with a low grade, a low proliferation rate index, and positive hormone receptor (11, 12). These features made it suitable for IORT. Thus, the percentage of patients treated with IORT is high.
Various results have been reported about ILC clinical outcome after IORT. Some studies have reported excellent clinical outcome after APBI for ILC. Despite a favorable features, ILC is suggested to use cautiously.
2. Objectives
The current study compares in-breast tumor recurrence (IBTR) and clinical outcome of ILC versus IDC in early breast cancer treated with radical IORT and evaluate ILC as a suitable criterion for radical IORT.
3. Methods
A total of 191 patients with early breast cancer (ductal and lobular) were treated with breast conserving surgery and radical IORT (21 Gy) in Cancer Research Center of Shahid Beheshti University of Medical Sciences (2013 - 2017). IORT was done by a specially designated mobile linear accelerator delivering energy levels of electrons (4 to 12 MeV) via a head maneuvered by a robot arm (Liac Deliver).
Primary end point was local recurrence incidence either tumor bed or axilla. Local recurrence incidence was calculated from surgery date to recurrence date or the last follow-up date.
Secondary end point was disease-free survival (DFS) and it was evaluated, using the Kaplan-Meier method.
Pure IDC (135), ILC (42), and mixed type (14) were designated in this survey. Technical IORT parameters did not differ between the subtypes and ILC like IDC was a suitable criterion for radical IORT (Table 1). The log-rank test was used for testing the equality of survival distributions for IDC and ILC.
| Characteristics | Non-Lobular | Lobular |
|---|---|---|
| Total | 135 (70.7) | 56 (29.3) |
| Age | ||
| < 40 | 0 (0) | 1 (1.8) |
| 40 - 44 | 3 (2.2) | 5 (8.9) |
| ≥ 45 | 132 (97.8) | 50 (89.3) |
| Tumor Size | ||
| < 3 | 115 (85.8) | 49 (87.5) |
| 3 - 3.5 | 17 (12.7) | 7 (12.5) |
| > 3.5 | 2 (1.5) | 0 (0) |
| Grade | ||
| 1 | 21 (16.2) | 13 (23.6) |
| 2 | 71 (54.6) | 36 (65.5) |
| 3 | 38 (29.2) | 6 (10.9) |
| LVI | ||
| Positive | 16 (12.5) | 4 (7.3) |
| Negative | 112 (87.5) | 52 (92.7) |
| ER | ||
| Positive | 110 (82.7) | 52 (92.9) |
| Negative | 23 (17.3) | 4 (7.1) |
| PR | ||
| Positive | 104 (78.8) | 51 (91.9) |
| Negative | 28 (21.2) | 33 (17.6) |
| Her2 | ||
| Positive | 8 (6.0) | 2 (3.6) |
| Negative | 125 (94.0) | 54 (96.4) |
| KI67 | ||
| < 20% | 77 (58.8) | 40 (71.4) |
| 20% - 30% | 31 (23.7) | 9 (16.1) |
| > 30% | 23 (17.6) | 7 (12.5) |
| Luminal | ||
| Luminal A | 61 (45.9) | 25 (44.6) |
| Luminal B | 53 (39.8) | 28 (50.0) |
| HER2 positive | 3 (2.3) | 1 (1.8) |
| Triple negative | 16 (12.0) | 2 (3.6) |
. Clinical, Pathologic, and Molecular Subtype Related Characteristics for the ILC and IDC Group.
The data of each group were analyzed according to age, tumor size, molecular characteristics, adjuvant therapy, and follow-up. Clinical outcomes, including IBTR and DFS, were analyzed.
Univariate and multivariate Cox regression analysis were done and influence of tumor characteristics were evaluated. Molecular subtype analysis for estrogen receptor (ER), progesterone receptor (PR), Ki67 and human epidermal growth factor receptor 2 (HER2) expression were done as multivariate analysis.
This study was approved by ethical committee of Shahid Beheshti University of Medical Sciences.
4. Results
Median follow-up was 23.17 months for IDC patients and 21.17 months for ILC patients. The results of Mann-Whitney test shows that there is no significant difference in median follow-up between two group (P = 0.634).
Median age of patients was 60 years for the IDC and 57.28 for the ILC and 57.7 for the mixed type.
Although, median age of ILC was less than IDC, percent patients ≥ 70 years, was similar to IDC (IDC = 17.7% vs. ILC = 16.06%). Nevertheless, just 10% of the patients with ILC were under 45 years old.
Compared to IDC group, patients with ILC were lower grade (G1, 2; 87.8% vs. 71.1%), less lymphovascular invasion (92.7% vs. 87.5%), high hormonal status (ER, 92.9% vs. 82.7% - PR, 95.2% vs. 78.8%), greater HER2 negativity (100% vs. 94%), and lower proliferation index (Ki67 ≥ 30%, 11.9% vs. 17.6%) (Table 1).
In two groups, tumor sizes were alike except, the ILC was not over 3cm.
There are two patients with recurrence in IDC group (one patients with local recurrence and the other one systemic recurrence) and one local recurrence in ILC patients (Table 2).
| Pathology | Recurrence Indicator | Total | |
|---|---|---|---|
| No | Yes | ||
| IDC | |||
| Count | 134 | 1 | 135 |
| % within pathology | 99.2 | 0.74 | 100.0 |
| ILC | |||
| Count | 41 | 1 | 42 |
| % within pathology | 97.6 | 2.4 | 100.0 |
| IDC/ILC | |||
| Count | 14 | 0 | 14 |
| % within pathology | 100.0 | 0.0 | 100.0 |
| Total | |||
| Count | 188 | 3 | 191 |
| % within pathology | 98.4 | 1.6 | 100.0 |
Local Recurrence Indicator
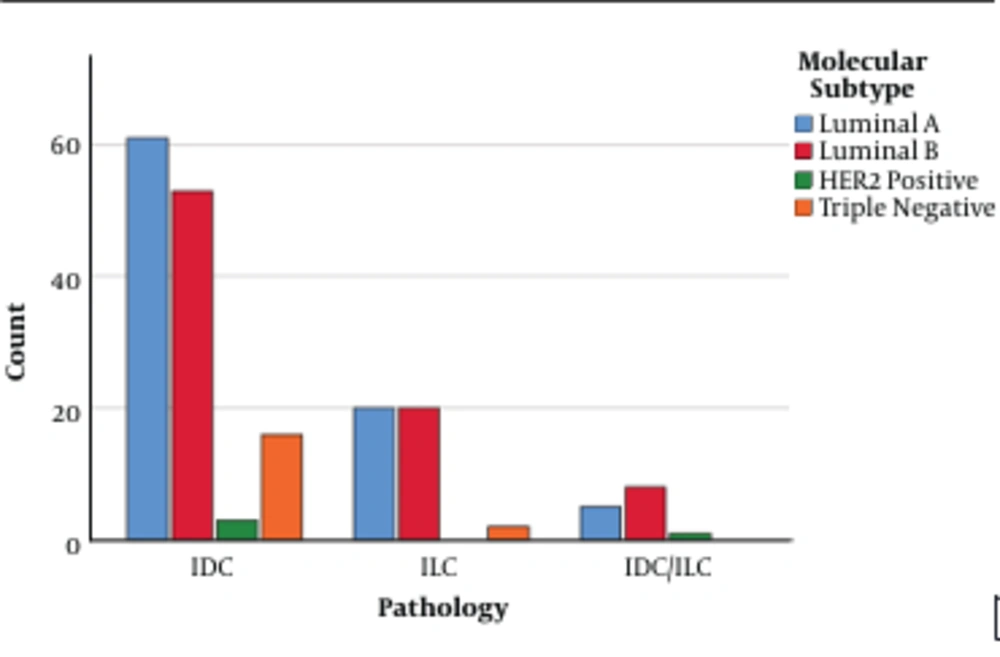
In the multivariate analysis, ER, PR, Ki67, and HER2 expression were represented by molecular subtype (Luminal A, Luminal B, HER2 positive, triple negative). Compared to the IDC group, patients with ILC were Luminal A (44.6% vs. 45.9%) and Luminal B (50% vs. 39.8%) rather than HER2 positive (1.8% vs. 2.3%) and triple negative (3.6% vs. 12%) (Table 3 and Figure 1).
| Pathology | Molecular subtype | Total | |||
|---|---|---|---|---|---|
| Luminal A | Luminal B | HER2 Positive | Triple Negative | ||
| IDC | 61 (45.9) | 53 (39.8) | 3 (2.3) | 16 (12) | 133 |
| ILC | 20 (44.6) | 20 (50) | 1 (1.8) | 2 (3.6) | 42 |
| IDC/ILC | 5 | 8 | 0 | 0 | 14 |
| Total | 86 | 81 | 4 | 18 | 189 |
Molecular Subtype of Two Group
The results of Cox regression analysis showed that the AHR for lobular patients compared to non-lobular patients was 1.34 (95% CI: 0.12 - 14.73; P = 0.813). So, there is no significant difference in the risk of recurrence between lobular and non-lobular patients.
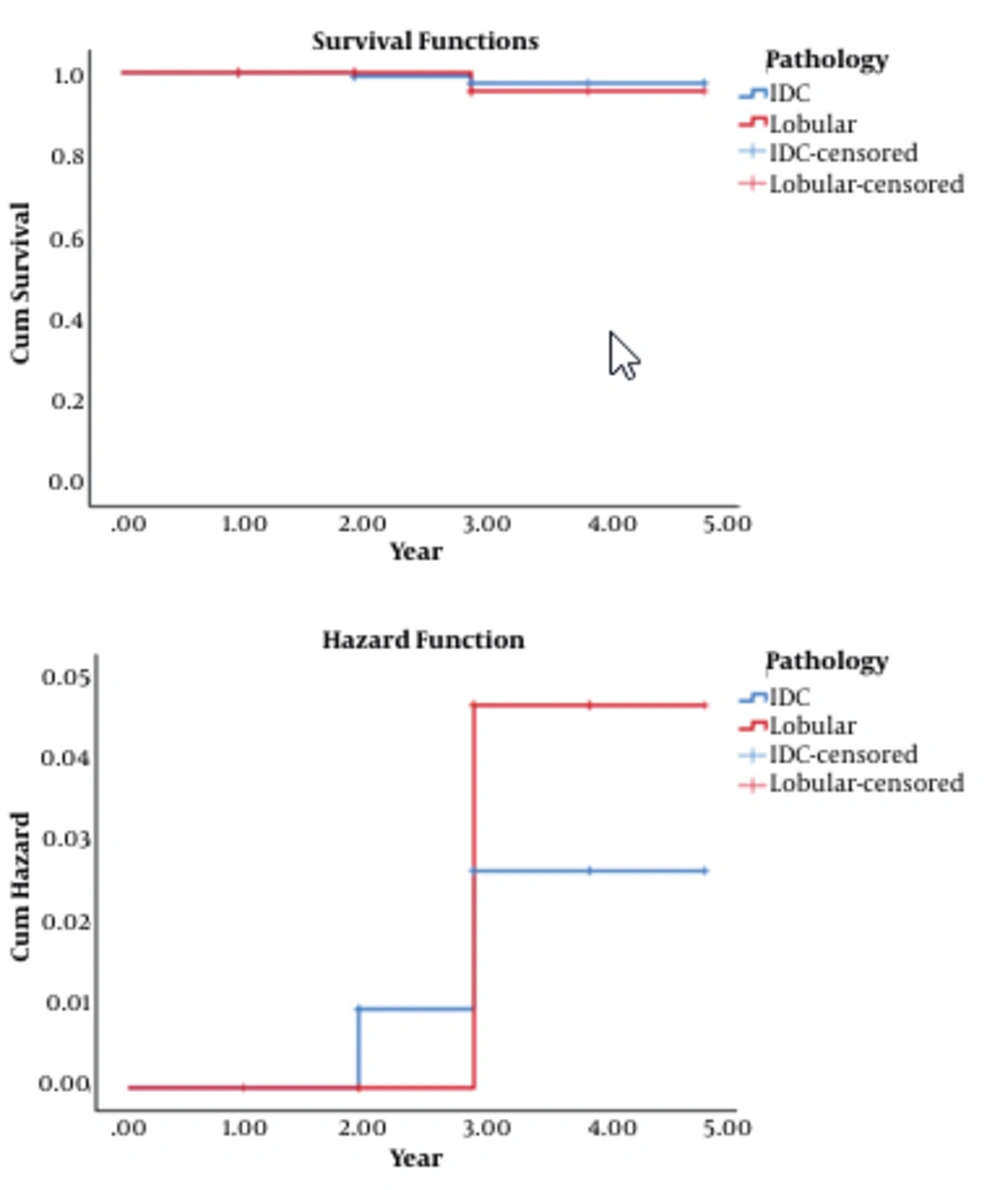
Also, there is no difference in survival distributions for the different levels of pathology. The two years DFS is 100% for lobular and 99.05% for IDC patients. The 4 years DFS is 95.45% for lobular and 97.40% for IDC patients. Therefore, there is no statistical difference in DFS of two groups within 2 years and 4 years (Tables 4 and 5 and Figure 2).
| Pathology | Meana | Median | ||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | Std. Error | 95% Confidence Interval | Estimate | Std. Error | 95% Confidence Interval | |||
| Lower Bound | Upper Bound | Lower Bound | Upper Bound | |||||
| IDC | 4.938 | 0.043 | 4.854 | 5.023 | - | - | - | - |
| Lobular | 4.909 | 0.089 | 4.735 | 5.083 | - | - | - | - |
| Overall | 4.931 | 0.039 | 4.854 | 5.008 | - | - | - | - |
Means and Medians for Survival Time
| Type of Test | Overall Comparisons | ||
|---|---|---|---|
| Chi-Square | df | P Value | |
| Log rank (Mantel-Cox) | 0.057 | 1 | 0.812 |
| Breslow (Generalized Wilcoxon) | 0.001 | 1 | 0.971 |
| Tarone-Ware | 0.011 | 1 | 0.918 |
Test of Equality of Survival Distributions for the Different Levels of Pathology
5. Discussion
In the present study, women with early breast cancer were treated with the IOERT for comparing the rate of local recurrence of ILC and IDC at the median follow-up of 23.17 and 21.7 month, respectively. There was no evidence of difference regarding local recurrence. Overall survival and disease-free survival did not differ between two groups.
As previous studies (13, 14) showed, lobular carcinoma was more likely to be ER-PR positive, low to be LVI positive, and to be absent HER2. Also, despite a less aggressive biologic phenotype, recurrence and survival were similar to IDC patients.
Prior studies afford to consider ILC as a cautionary criteria in normal routine and again APBI guidelines (15, 16). So, the most of studies like randomized trial of accelerated partial breast irradiation (RAPID), targeted intraoperative radiotherapy (TARGIT) (12, 17), and IMPORT LOW (18) did not include patients with ILC on trials. Besides, ILC patients were registered in other studies as ELIOT (19), IRMA, and Groupe Européen de Curiethérapie -European Society for Radiotherapy and Oncology (GEC-STERO)- (17, 20), while the most of them did not report any association between local recurrence and histologic type.
In Leonardi et al. study (21), patients with ILC (252; 11.6%) were compared to those with IDC (1921; 88.4%). The 5 and 10 years IBTR rate were 7.5% and 21.8%, respectively, for ILC patients versus 5.5% and 14.4%, respectively, for IDC patients. They declared patients with ILC can be used for APBI with caution.
We contrasted 42 patients with ILC to 135 patients with IDC. The 2 years DFS is 100% for lobular and 99.05% for IDC patients. Also, 4 years DFS was 95.45% and 97.40%, respectively. So, there was no statistical difference between two groups.
Many of literature about ILC reported low grade, absence of lymphovascular invasion, positive expression of hormone receptors, greater HER2 negativity, and occurrence in older patients (13, 14). Our patients with ILC were younger. It may be due to youth population of area. Our patients with ILC had low risk profile, as well. They were as young as patients with IDC.
Multivariate analysis was according to molecular subtype. Perhaps, multivariate analysis demonstrated better biologic behavior for ILC. Whereas, 44.6% of the patients with ILC were Luminal A versus 45.9% of the patients with IDC; other subtypes included Luminal B (50% vs. 39.8%), HER2 positive (1.8% vs. 2.3%), and triple negative (3.6% vs. 12%), respectively.
Table 6 shows that there is no significant difference in hazard ratio between two groups with respect to their covariate values. Hazard ratio for Luminal B is 3.419; it means the HR of Luminal B is 3.419 times more than other subtypes. As regards high percentage of Luminal B in ILC patients, it seems lobular pathology is susceptible to IBTR, whereas there is no statistical significance.
| Characteristics | Beta | Standard Error | HR | 95% CI | P Value |
|---|---|---|---|---|---|
| Age | |||||
| < 40 | |||||
| 40 - 44 | -3.098 | 11.835 | 0.045 | (0.000, 5E09) | 0.794 |
| ≥ 45 | 3.098 | 11.835 | 22.147 | (0.000, 2E+11) | 0.794 |
| Tumor Size | |||||
| < 3 | 3.276 | 7.097 | 26.474 | (0.000, 2E+08) | 0.644 |
| 3 - 3.5 | -3.239 | 7.435 | 0.039 | (0.000, 8E+05) | 0.663 |
| > 3.5 | -3.035 | 21.120 | 0.048 | (0.000, 4E+16) | 0.886 |
| Grade | |||||
| 1 | -3.344 | 6.409 | 0.035 | (0.000, 1E+05) | 0.602 |
| 2 | 4.171 | 4.758 | 64.771 | (0.010, 7E+06) | 0.381 |
| 3 | -3.664 | 5.377 | 0.026 | (0.000, 966) | 0.496 |
| LVI | |||||
| Positive | 1.280 | 1.241 | 3.598 | (0.316, 40.498) | 0.302 |
| Negative | -1.280 | 1.241 | 0.278 | (0.024, 3.164) | 0.302 |
| ER | |||||
| Positive | 3.234 | 7.478 | 25.384 | (0.000, 5E+08) | 0.665 |
| Negative | -3.234 | 7.478 | 0.039 | (0.000, 9E+05) | 0.665 |
| PR | |||||
| Positive | 3.354 | 6.212 | 28.614 | (0.000, 5E+07) | 0.589 |
| Negative | -3.354 | 6.212 | 0.035 | (0.000, 6E+04) | 0.589 |
| Her2 | |||||
| Positive | -3.141 | 11.369 | 0.043 | (0.000, 2E+9) | 0.782 |
| Negative | 3.141 | 11.369 | 23.120 | (0.000, 1E+11) | 0.782 |
| KI67 | |||||
| < 20% | -1.177 | 1.228 | 0.308 | (0.028, 3.422) | 0.338 |
| 20% - 30% | 0.591 | 1.232 | 1.805 | (0.161, 20.175) | 0.632 |
| > 30% | 0.928 | 1.225 | 2.528 | (0.229, 27.892) | 0.449 |
| Luminal | |||||
| Luminal A | -0.726 | 1.226 | 0.484 | (0.044, 5.348) | 0.554 |
| Luminal B | 1.229 | 1.230 | 3.419 | (0.307, 38.079) | 0.317 |
| HER2 positive | -3.054 | 17.667 | 0.047 | (0.000, 5.2E+13) | 0.863 |
| Triple negative | -3.161 | 8.509 | 0.042 | (0.000, 7.4E+6) | 0.710 |
Hazard Ratio between ILC and IDC Patients, According to Clinical, Pathologic, and Treatment Related Characteristics (Stratified Analysis)
5.1. Conclusions
Many of studies, which included lobular carcinoma on trial, did not report by histology. So, the current study not only did it, but also registered the ILC as a suitable criterion in the survey. According to the results, there was no significant difference in IBTR and DFS between two groups. It seems lobular carcinoma can be used for APBI and it may be a suitable criterion as the IDC. This study evaluated patients on 4 years and follow-up period was not long. Thereafter, it is better the study go on in the future and more accurate results would be reported.